Advanced Techniques in Biology & Medicine
Open Access
ISSN: 2379-1764
ISSN: 2379-1764
Research Article - (2023)Volume 11, Issue 1
The Waon Therapy (WT) has dominated over Thermal Therapy (TT) for chronic heart failure. Whole-body TT using Hot Packs Thermal Therapy (HPTT) may improve blood flow to the whole body. However, changes in blood flow with HPTT have not been verified. This study aimed to compare Lower-Extremity Blood Flow (LEBF) before and after HPTT and WT using venous occlusion plethysmography. We recruited 11 healthy men (28.3 ± 6.2 years). The participants underwent either HPTT or WT for 24 h. The HPTT protocol involved patients in a supine position on a bed for at least 10 min. Hot packs were then applied to the back, lower abdomen, and popliteal region for 15 min (warming). They were removed after 15 min, and the participants continued bed rest for 30 min (heat retention). The WT was performed as previously reported. LEBF was measured in the right lower leg using venous occlusion plethysmography before and after TT. Both TT approaches significantly increased LEBF (HPTT: 1.29 ± 0.48 ⇒ 2.75± 1.07%/min, p=0.001; WT: 1.51 ± 0.85 ⇒ 2.83 ± 0.90%/min, p<0.001). There was no significant difference between the pre and post-implementation values of either TT, and no interaction effect was observed. HPTT increased LEBF by approximately twice as much as that at rest and its effect was comparable to that of WT.
Thermal therapy; Hyperthermia; Hot pack; Waon therapy; Blood flow
Thermal Therapy (TT) is a commonly used physical therapy method [1,2]. TT is roughly categorized by its warming degree into local TT, such as hot pack or microwave, and whole-body therapy, such as sauna therapy [3], hot water immersion [4,5] or sauna suits [6,7]. A hot pack is a physical therapy device available at general facilities. When using a hot pack heated to 80–85°C in a thermostatic bath, a method used in the past, it is classified into “dry” and “wet” methods [1,2]. In the “dry” method, a warmed hot pack is wrapped in a plastic bag and then doublewrapped in a bath towel. In the “wet” method, a heated hot pack is wrapped directly in three or four bath towels. According to previous studies [8,9], both methods increase the temperature directly under the skin to 40–42°C, leading to increased skin blood flow and decreased muscle hardness [10-14]. However, the general method of applying hot packs is localized and superficial, with heat conduction only at the contact site and difficulty increasing the temperature of other areas, increasing the deep whole-body temperature, or improvement in blood flow to other parts of the body [15,16]. Therefore, we investigated whether whole-body TT using a combination of hot packs and aluminum sheets (HPTT) would increase the deep body blood flow velocity and temperature and produce a vasodilatory response comparable to that of Waon Therapy (WT), a commonly used TT for chronic heart failure [17]. Although whole-body heating with this method is expected to decrease systemic vascular resistance and increase systemic blood flow by increasing the deep body temperature [18,19], no reports to date have evaluated HPTT.
This study hypothesized that HPTT would be as effective as WT at increasing Lower-Extremity Blood Flow (LEBF). This study aimed to evaluate LEBF using Venous Occlusion Plethysmography (VOP) among subjects who cooperated in a study examining cardiovascular responses to HPTT and WT. If HPTT were to increase blood flow as well as deep body temperature, it may confirm the effectiveness of TT using hot packs and help provide a simple and inexpensive approach to improving impaired blood flow and circulation.
The participants were 11 healthy men who agreed to undergo LEBF measurements during the study (mean age, 28.3 ± 6.2 years; mean height, 170.0 ± 6.9 cm). The participants underwent HPTT or WT in a random sequence (randomized crossover study). HPTT and WT were separated by a minimum of 1 d and maximum of 1 month. The cases and measurement records for this study were collected from participants in our previous study.
Thermal therapy
The study protocols for both thermal therapies were summarized in a previous study [17]. The participants avoided physical exercise, eating, and smoking for 3 h before the treatment, and they avoided caffeine consumption 6 h prior to the procedure on the day of therapy. This study was performed in a quiet room at 28–30°C. Participants wore hygroscopic gowns.
Whole-body HPTT
Hot packs that had been warmed to 80°C were used after wrapping a plastic bag and towel around them (Minatopack KPA1076, 25 × 30 cm, hydro advertiser HC-6U; Minato Ikagaku Inc., Osaka, Japan).
The HPTT protocol involved a participant lying in the supine position on a bed for at least 10 min. The participants were covered with thin aluminum foil sheets (heat-retaining aluminum sheets; JTH-1321, 130 × 210 cm; IRIS OHYAMA, Sendai, Japan). Subsequently, hot packs were applied to the participant’s back (on the third lumbar vertebra), lower abdomen (anterior superior iliac spine), and popliteal regions for 15 min (warming phase). After 15 min, the hot packs were removed and the participants continued bed rest for 30 min (heat retention phase). During the warming and heat retention phases, the participant remained covered with thin aluminum foil sheets and a blanket.
Waon therapy
We used far-infrared dry sauna equipment for the WT (CTW-5000; Fukuda Densi, Tokyo, Japan). The WT protocol involved patients lying in the supine position on a bed for at least 10 min. Subsequently, they were seated in dry sauna for 15 min. During the heat retention phase, they rested supine on the bed for 30 min wrapped in a blanket.
Physiological measurements
The variables measured included Heart Rate (HR), Blood Pressure (BP), Body Weight (before and after TT), Tympanic Temperature (measured every minute), and Leg Blood Flow (before and after TT).
Tympanic temperature
We continuously measured tympanic temperature as an index of the deep-body temperature at the right ear during both thermal therapies [20-22]. We inserted the thermistor probe into the right ear and confirmed its position when a participant reported a “scratching noise” or “sharp pain” when the head of the probe touched the tympanic membrane.
Lower-extremity blood flow
We used VOP to measure the LEBF (EC6 Strain Gauge and Photoplethysmography System; D. E. Hokanson, Inc., Bellevue, WA, USA). To measure the LEBF, the right lower limb was lifted and the foot rested on a 10-cm-high cushion in the supine position. The strain gauge was wrapped around the bulge of the lower leg and the cuff was wrapped around the right thigh (Rapid Cuff Inflation System; D. E. Hokanson, Inc.).
The LEBF was measured at least twice (at rest and after 30 min of heat retention). We measured the electrical potential from the strain gauge after the cuff was momentarily pressurized at 50 mmHg. We calculated the blood flow from the obtained electrical potential of the circumferential change.
Statistical analysis
The data are presented as mean ± standard deviation. Statistical analyses were performed using Statistics for Excel 2012 (Social Survey Research Information Co., Tokyo, Japan). Four measurement timings (rest, at the end of warming, and after 15 and 30 min of heat retention) of tympanic temperature, systolic and diastolic BP, and HR were extracted from the data of previous studies. Statistical analyses included two-way analysis of variance and post-hoc Bonferroni correction. Statistical significance was identified at values of p<0.05. Body weights and LEBF before and after the therapies were compared using a paired t-test, with significance identified at p<0.05.
No adverse events such as low-temperature burns, tympanic injury, or postural hypotension were observed in this study. Likewise, no significant differences in baseline measurements, such as body weight, BP, and HR, were observed between the HPTT and WT groups.
Body weight
Body weight was significantly reduced in both thermal therapies (HPTT: from 63.65 ± 9.86 [57.83–69.48] to 63.39 ± 9.92 [57.53– 69.25] kg, p=0.002; WT: from 63.35 ± 9.72 [57.59–69.10] to 63.09 ± 9.75 [57.33–68.85] kg; p<0.001). The mean decrease in body weight was approximately 0.25 kg in both groups and did not differ significantly between them (HPTT: 0.25 ± 0.21 [0.14–0.39] vs . WT: 0.25 ± 0.11 [0.19–0.32] kg, p=0.844).
Tympanic temperature, BP and HR
In the HPTT group, the tympanic temperature increased and was significantly higher after 15 min of heat retention versus at rest. In contrast, the tympanic temperature during the WT increased dramatically during the warming phase and remained significantly elevated during the heat retention phase. The tympanic temperature was significantly higher in the WT versus HPTT between 15 min of warming and 15 min of heat retention. However, it was not significantly different at 30 min of heat retention.
Blood flow
TT significantly increased the mean LEBF (HPTT: 1.29 ± 0.48 [1.01–1.57] to 2.75 ± 1.07 [2.12–3.38]%/min, p=0.001; WT: 1.51 ± 0.85 [1.00–2.01] to 2.83 ± 0.90 [2.30– 3.36]%/min, p<0.001). There was no difference between the TT in LEBF before versus after treatment.
Systolic BP did not change significantly during either TT. The mean diastolic BP decreased during heat retention in both groups.
The HR during HPTT rose continuously and was significantly higher after warming versus at rest. On the other hand, the HR during the WT rose immediately during the warming phase; however, during the heat retention phase, it declined and then plateaued. The mean HR in the WT was significantly higher than that in the HPTT at warming; however, after 30 min of heat retention, the HR was significantly higher in the HPTT than WT group (Table 1).
| Characteristics | Rest | Warming | 15 min of heat retention | 30 min of heat retention | |
|---|---|---|---|---|---|
| Tympanic temperature (°C) | HPTT | 36.48 ± 0.31 | 36.71 ± 0.26 | 36.81 ± 0.25 | 36.85 ± 0.32 |
| [36.30-36.66] | [36.55-36.86] | [36.66-36.95] | [36.65-37.04] | ||
| WT | 36.45 ± 0.27 | 37.85 ± 0.40* | 36.93 ± 0.25 | 36.90 ± 0.26 | |
| [36.29-36.6] | [37.61-38.08] | [36.78-37.07] | [36.75-37.05] | ||
| Systolic BP (mmHg) | HPTT | 110.1 ± 9.7 | 112.6 ± 10.2 | 111.7 ± 7.1 | 112.5 ± 10.0 |
| [104.3-115.8] | [106.6-118.6] | [107.5-115.9] | [106.6-118.5] | ||
| WT | 107.9 ± 7.5 | 111.4 ± 15.4 | 107.5 ± 8.3* | 105.5 ± 6.1* | |
| [103.4-112.3] | [102.2-120.5] | [102.6-112.5] | [101.9-109.2] | ||
| Mean BP (mmHg) | HPTT | 85.3 ± 7.5 | 84.8 ± 8.0 | 82.5 ± 7.5 | 85.5 ± 7.9 |
| [80.9-89.8] | [80.1-89.6] | [78.1-87] | [80.8-90.1] | ||
| WT | 84.4 ± 6.1 | 89.3 ± 8.1*† | 81.5 ± 7.7 | 82.6 ± 6.7 | |
| [80.8-88] | [84.5-94.1] | [77-86.1] | [78.7-86.6] | ||
| Diastolic BP (mmHg) | HPTT | 66.6 ± 6.0 | 65.5 ± 6.5 | 63.4 ± 5.9† | 63.9 ± 5.8† |
| [63.0-70.2] | [61.6-69.3] | [59.9-66.8] | [60.5-67.3] | ||
| WT | 64.6 ± 5.9 | 67.9 ± 6.5† | 62.9 ± 5.3 | 61.5 ± 4.7*† | |
| [61.1-68.1] | [64.1-71.7] | [59.8-66] | [58.8-64.3] | ||
| Heat rate (bpm) | HPTT | 65.9 ± 7.3 | 69.9 ± 9.1 | 71.3 ± 8.9 | 76.7 ± 9.3 |
| [61.6-70.2] | [64.5-75.3] | [66.1-76.6] | [71.2-82.2] | ||
| WT | 65.7 ± 7.9 | 89.7 ± 12.6* | 69.9 ± 7.7 | 70.5 ± 8.6 | |
| [61.1-70.3] | [82.2-97.1] | [65.3-74.4] | [65.4-75.6] | ||
Note: Values are shown mean ± standard deviation [95% confidence interval]. BP- blood pressure, bpm- beats per minute. *p<0.05 vs. HPTT and †p<0.05 vs. rest.
Table 1: Changes in deep body temperature, blood pressure and heart rate after Waon therapy (WT) versus Thermal Therapy using Hot Packs (HPTT).
Furthermore, there was no significant difference between the TT in the mean before and after difference (HPTT: 1.46 ± 0.76 [1.00–1.91]%/min; WT: 1.32 ± 0.51 [1.02–1.63]%/min) or increase (HPTT: 222 ± 68 [182–262]%; WT: 228 ± 104 [167–290]%) (Figures 1a-1c).
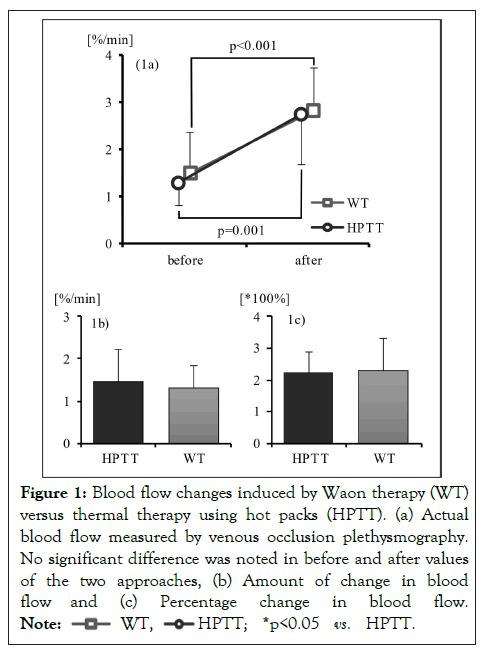
Figure 1: Blood flow changes induced by Waon therapy (WT)
versus thermal therapy using hot packs (HPTT). (a) Actual
blood flow measured by venous occlusion plethysmography.
No significant difference was noted in before and after values
of the two approaches, (b) Amount of change in blood
flow and (c) Percentage change in blood flow. 
This study is the first to report changes in LEBF induced by HPTT and WT. The HPTT resulted in approximately double the LEBF versus the resting state. Although this was a beforeand- after comparison, the effects of HPTT were comparable to those of WT, indicating the possibility of its ability to improve LEBF.
Increased blood flow
The HPTT resulted in approximately double the LEBF at the end of treatment versus resting state. Although there were individual differences in the degree of blood flow increase, the LEBF increased in all participants. In a previous study, the brachial artery dilated by approximately 10% and HR increased by approximately 20% during HPTT [17]. The increase in deep body temperature also suggests a decrease in cutaneous and systemic peripheral vascular resistance [3,18]. In addition, various factors, including nitric oxide from endothelial cells, cause vasodilation through their actions on the vascular smooth muscles. Vasodilation by transient receptor potential channels in endothelial cells is involved in the first vasodilatory reaction to TT [23,24]. The combined effect of these factors seems to have led to the increase in LEBF.
Therapeutic effect of increased blood flow
In the case of wounds associated with impaired peripheral blood flow, WT can have a wound healing effect [25,26]. HPTT also increased LEBF to the same extent as WT, suggesting that this therapy was effective at wound healing.
For patients who have difficulty receiving direct TT on the wound site or assuming a seated position, the use of an aluminum sheet to keep the area warm provides a thermal therapeutic effect distal to the actual thermal stimulation site. Thus, the effect of TT can be achieved with fewer burdens on the wound.
However, this study showed an increase in the blood flow after TT. As the HR and autonomic nerve responses differ between HPTT and WT, the change in blood flow that occurs during the process is unclear. Changes in blood flow also require examination.
Study limitations and future study directions
The present study had some limitations. First, the blood flow assessments were available only before and after TT because we used the VOP; thus, it is unclear whether the temporal changes differ between the approaches.
Second, it is unclear whether the benefits of HPTT are equal to those of WT in patients with peripheral artery disease or heart failure because the participants of this study were limited to healthy men.
HPTT increased LEBF by approximately twice as much as at rest, and the effect of the increased LEBF was comparable to that of WT. These findings suggest that HPTT can conveniently improve blood flow without the need for special equipment. It will be desirable to conduct further research on the differences in changes in blood flow and their long-term effects in patients with cardiovascular or other chronic diseases. Therefore, it will be desirable to evaluate blood flow using an infrared blood flow meter or similar device in future studies.
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the ethical committee of Hakodate National Hospital (approval number: H28-1114006). Informed consent was obtained from all participants for their participation in the study and the publication of this report. The authors confirmed that the participants could not be identified via the paper and their identities were fully anonymized. Furthermore, the authors affirm that all mandatory health and safety procedures were complied with in the course of all experimental work reported in this study.
We would like to thank Editage for assistance in English language editing.
The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
This study received no funding from the for-profit or not-forprofit sectors. The study was performed at the Department of Clinical Research, National Hospital Organization Hakodate Hospital, Hakodate, Japan.
The authors declare no conflict of interest.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]2005;112:2286-2292.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Kominami K, Noda K, Takahashi N, Izumi T, Yonezawa K (2023) Increased Blood Flow in Whole-Body Thermal Therapy with Hot Packs Versus Waon Therapy. Adv Tech Biol Med. 11:395.
Received: 20-Jan-2023, Manuscript No. ATBM-23-21476; Editor assigned: 24-Jan-2023, Pre QC No. ATBM-23-21476 (PQ); Reviewed: 07-Feb-2023, QC No. ATBM-23-21476; Revised: 14-Feb-2023, Manuscript No. ATBM-23-21476 (R); Accepted: 23-Mar-2023 Published: 23-Feb-2023 , DOI: 10.35248/2379-1764.23.11.395
Copyright: © 2023 Kominami K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.