Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Case Report - (2023)Volume 12, Issue 2
Type 1 Diabetes Mellitus (T1DM) is one of the most widespread chronic disease affecting children, and young adults International Diabetes Federation, (IDF). It is a heterogeneous disorder characterized by damage of pancreatic beta cells, terminating in absolute insulin deficiency. T1DM is a challenging illness and requires lifelong diabetes self-care which includes self-monitoring of blood glucose, daily multiple insulin injections, close monitoring of food intake, regular exercise, investigations, and visits to Health Care Professionals (HCPs). In addition, there are impending risks of hypoglycemia, weight gain, and complications. Genetic, metabolic, and environmental factors act together to precipitate the onset of the disease. The global incidence of T1DM in children and adolescent is rising with an estimated overall annual increase of approximately 3%. T1DM accounts for about 10% of all cases of diabetes, occurs most commonly in people of European descent. The lowest incidence has been found in Asia and Oceania. About 128,900 children (0-19) years are estimated to develop T1DM annually world-wide.
Diabetes; Adolescents; Mortality rates; Socioeconomic; Environment
T1DM is also on increase like type 2 diabetes, even though not in the same proportion, but still with a trend of 3%-5% increase/year.
India, USA, and Brazil have the largest number of children and adolescents (0-14) with prevalent and incident T1DM. Selfmanagement of T1DM over a lifetime is complex and challenging even in best of the circumstances and the social environment can be a powerful determinant of health behaviors and outcomes [1-3].
T1DM care in India poses many challenges as there is intermittent or no supply of insulin and no government support for supplying test strips, syringes, and HbA1c testing. Additional obstacles include poverty, limited literacy, and unavailability of educational resources leading to unawareness, cultural factors, and paucity of expert doctors, nurses, and diabetes educators in rural settings. There is limited data on complication and mortality rates, but evidence suggests they are often high relative to adequate resource settings [4,5].
The social determinant of childhood environment, education, socioeconomic status, gender, ethnicity, and culture of public health demonstrate an inverse socioeconomic mortality gradient and increased morbidity for people with lower socioeconomic groups having poorer outcomes, contributing to disengagement from treatment regimens, the development of complications at comparatively early age and higher rate of death.
Ms. SB is an Asian Indian Muslim female of 18 years with type 1 diabetes, weight loss and recurrent episodes of diabetic ketoacidosis due to unavailability of insulin injection. Confidentiality would be upheld by keeping the identity anonymous. Neither the organization nor the person involved would be specified by name. The author is engaged in management of this patient.
Ms. SB was apparently asymptomatic 2 days ago when she complained of pain in her abdomen. She also complained of nausea and loss of appetite. On further questioning, she reported missed insulin dosages for 3 days as she was not able to buy it. Two days ago, when she presented with the same symptoms, pointing towards an imminent ketoacidosis, we sat her down and questioned her history of insulin and drug intake. She reported unfortunately, that due to her father’s reluctance towards getting her treated, and being financially constrained, she was unable to buy insulin as prescribed. Added to the misery was a lack of government funded insulin supplies in primary health centers, and regular check-up for children with diabetes in the remote area where she lived [6].
Pertinent and antecedent history
SB, daughter of a bangle-maker, hails from a remote part of rural Eastern India. She has four siblings, two older sisters and a younger brother and a sister. All the sisters help their father in the small bangle-making cottage industry in the outskirts of their village. There is no family history of diabetes.
The child first reported of pain in abdomen, with burning sensation in urine and nausea, loss of appetite with frequent bouts of vomiting 6 months back. She was hospitalized for the same in the local nursing home and discharged with a diagnosis of diabetic ketoacidosis, which was assessed through her previous prescriptions and investigation slips, as attached (Table 1) [7-9].
| WBC (TLC) | 18000/cc |
| Neutrophil, lymphocyte, eosinophil, monocyte | 85, 15, 0, 0 (%) |
| Blood sugar (random) | 487 mg/dl |
| HbA1c | 11.8 g% |
| Urine examination | Protein-trace, ketone-3+ |
| Urine culture | E. coli (105) |
| Serum creatinine | 1.2 mg/dl (Normal<1.5 mg/d) |
| SGPT | 88 IU/L |
| Note: (Serum BHB was not tested) | |
Table 1: Different tests and their levels.
She was put on basal bolus insulin regimen but unfortunately, due to a lack of proper follow up and insulin intake, there were frequent episodes of such attacks followed by a period of hospitalization and release. She reported to this diabetes center after one such attack 4 months back. On questioning, there was a lack of proper lifestyle plan, dietary regimen with no idea about insulin-carbohydrate ratio, neither regular insulin intake in adequate dosage by the child. She was prescribed a meal plan, lifestyle modifications, and a basal bolus insulin regimen with education about insulin-carbohydrate ratio and food-calorie exchange. She was asked to report again within 2 weeks. She did not report leading to a loss to follow-up [10-13].
Physical examination
The team of diabetes care program in this centre, consisting of physician-diabetologist, physician assistant, diabetes educator, and dietitian, fended to her immediately when she reported.
Ms SB was alert, anxious, a febrile with O2 saturation of 99% while breathing ambient air (Tables 2-4).
| Pulse | BP | RR | Height | Weight | BMI | Waist | Skin |
|---|---|---|---|---|---|---|---|
| 84/min | 110 mmHg | 14/min | 5'3" | 49 kg | 19.1 kg/m2 | 28 cm | NAO |
Table 2: Physical examination.
| Cardiovascular | NAD |
| Respiratory | NAD |
| Neurological | No focal neurological deficit. Fundus NAD |
| Gastrointestinal | NAD |
| Musculoskeletal | NAD |
Table 3: Systemic examination.
| Creatinine (ma/dL) | 0.8 |
| Uric acid (mg/dL) | 4 |
| Na (meq/L) | 134 |
| K (meq/L) | 4.4 |
| SGPT (lU/L) | 34 |
| SGOT (IU/L) | 32 |
| Alk. Phos. (lU/L) | 94 |
| Cholesterol (mg/dL) | 168 |
| LDL (ma/dl) | 110 |
| HDL (mg/dL) | 38 |
| TG (mg/dL) | 170 |
| VLDL (mg/dL) | 36 |
| Urine examination | Trace ketone |
| UACR (mg/g) | <30 |
| TSH (mlU/L) | 3 |
| Blood sugar (fasting) (mg/dL) | 280 |
| HbA1c | 13.2% |
| Fastina C peotide (nmol/L) | 0.05 |
| (Hb: 11 g%; TLC: 8000; N: 65%; L: 30%; E: 3%; M: 2%) | |
Table 4: Investigation of test levels of a person.
Outline of care
This team of diabetes care program ensured monthly supply of free insulin for her. The team further counselled her father to help us in the endeavour to treat his child. They asked him to pay SB for the work she did at their cottage industry instead of procuring free labour. In that way, the money SB earned could be used in buying the medical supplies for her diabetes (Figure 1). The team also reasoned with the father how this disease can be fatal if not regulated with care. The details of our treatment approach have been elaborated below [14-16].
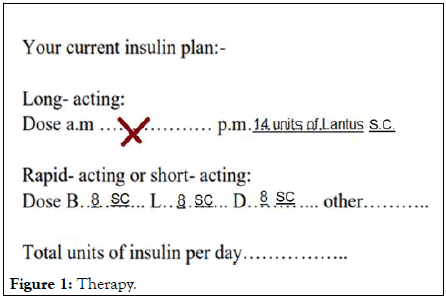
Figure 1: Therapy.
Focus of care
To deal with a girl-child hailing from a low educational background with poor means of living, the team first needed to define the various roadblocks that would form their focus of care in the treatment plan. This was the first step of approach in diabetes care.
Several problems that were affecting a successful treatment of the child came to light when they spoke to her about the hindrances she was facing during her treatment.
One of the major hurdles was her father’s reluctance to provide proper treatment for the child. He was unwilling to buy a regular supply of insulin and ensure a proper diet plan for SB. He said all of it would be a considerably costly affair which the family cannot afford, and his child’s inactivity in the workplace would lead to further loss. Primary focus of this care team, therefore, was to counsel the father for the same.
Another bottleneck that delayed the course of treatment was the gender bias, due to a low educational background, a sad consequence of poor socio-economic state, known as the feminization of poverty. It was seen the family did not pay attention to the health conditions, meal patterns of the girl-child as compared to their son. This is a common finding in rural, remote areas of India. A girl with diabetes is not preferred owing to wrong beliefs regarding physical and reproductive health. In South Asian countries like India, knowledge, and awareness about T1DM in general population is extremely poor. The focus of discussion with the family was regarding the need to provide equal health-care opportunities to their child irrespective of the long-held myths and beliefs [17-20].
Further the pertinent care towards the child was directed by the team, providing her with adequate support for her physical and mental well-being. It is very important to look for depressive symptoms in adolescent girls with type 1 diabetes owing to the daily social taboos they must deal with. The team attempted an individual-directed care which was the basis for step 2 of the course of treatment.
Person centered care approach
The goal was to acquaint the child to the disease and lay down specific measures for her to follow to control the frequent fluctuations in her health. It was essential to address the resistance faced in the society, associated mental agony that contributes to “diabetes distress” which has an adverse impact on glycemic control and overall quality of life of an individual, especially female, living with T1DM.
The team started simple. A healthy lifestyle plan was laid down. She was introduced to a meal plan, the basis of which was explained to her via an insulin-regimen with proper insulincarbohydrate ratio. The basics of food-calorie exchange was also taught to her. All was done keeping in mind that dietary management should be individualized: Family habits, religious or cultural needs, finances, physical activity, and the patient's and family's abilities in numeracy, literacy, and self-management should be considered. It was assumed she would not be able to assimilate a bulk of information at one go. Hence, to counter the communication gap between the patient and the doctor, a small pamphlet was prepared which had all the essential information she needed along with her diet and lifestyle planning, and the insulin regimen (Tables 5 and 6). A model of which has been attached below [21-23].
| HbA1c | 13.2% |
| BP | 110 mmHg/70 mmHg |
| LDL cholesterol | 110 mg/dl |
| Diet | 45% carbohydrate (start with 1400 K), 35% Protein, 20% Fat |
| Exercise | 60 minutes, aerobics, graded-daily 10 mins, resistance exercise thrice a week |
| BMI | 19.1 kg/m2 |
| Sleep | 10 PM-6 AM (8 hours) |
| Relaxation | Yoga, meditation, recreational games |
Table 5: Lifestyle planning, and the insulin regimen of a human.
Your new insulin plan
• Insulin to carb ratio: You will need 1 unit of rapid acting or short
acting insulin for each 8 grams of carbs.
• Blood glucose correction factor (insulin to correct high
blood glucose): 1 unit of rapid acting insulin for each 2.1
points (mg/dl) your blood glucose level is over target of 120 m
g/dl.
• Your pre-meal target blood glucose: 120 mg/dl.
Step 1: Calculate an insulin dose for food.
• Add up the grams of carbohydrate in the foods you will eat.
• Divide by your insulin to carb ratio.
(Total grams od carbohydrate to be eaten)/(Insulin to carb ratio)=Correction dose
=80/10
=8 units of insulin for food (carbs)
Step 2: How to use 'correction' factor to reach your target blood glucose.
• Subtract your target blood glucose from your current blood
glucose.
• Divide the difference by your correction factor.
(Current blood glucose-target blood glucose)/Correction
factor
=Correction dose
= (280 mg/dl-120 mg/dl)/75
= 160/75
=2.1
2.1 units of insulin will bring blood glucose of 280 mg/dl down to your target blood glucose of 120 mg/dl.
Step 3: Add the insulin needed for carbs to the insulin to correct high blood glucose for your total dose. 8 units of insulin +2.1 units to correct high blood glucose.
Total dose=10.1 units
| Breakfast | ||
| Menu | Quantity | Carbohydrates |
| Roti | 2 pc (50 gm) | 34.7 |
| Sabji | 1 bowl (100 gm) | 5.1 |
| Poha | 1 plate (120 gm) | 23.7 |
| Chila | 3 pc (60 gm) | 24.8 |
| Daliya | 1 plate (100 gm) | 22.1 |
| Suji upma | 1 plate (120 gm) | 37.3 |
| ldly | 2 pc (60 gm) | 22.8 |
| Sambhar | 1 bowl (80 gm) | 17.2 |
| Chutney | 2 spoon (10 gm) | 3.9 |
| Sprouts (chana moong) | 1 small bowl (30 gm) | 17.6 |
| Egg | 1 pc (50 gm) | 0 |
| Paneer | 50 gm | 0.6 |
| Milk | 1 glass (200 ml) | 8.8 |
| Cornflakes | 1/2 bowl (15 gm) | 16.8 |
| Lunch | ||
| Menu | Quantity | Carbohydrates (gm) |
| Rotil | 2 pc (50 gm) | 34.7 |
| Rice | 1 bowl (30 gm) | 23.7 |
| Daal | 1 bowl (100 mI) | 17.2 |
| Curd | 1 small bowl (100 gm) | 3 |
| Salad | 1 plate (100 gm) | 3.7 |
| Teesi | 4 tsp (20 gm) | 5.7 |
| Vegetable | 1 bowl (100 gm) | 5.1 |
| Chicken | 4 pc (60 gm) | 0 |
| Fish | 2 pc (50 gm) | 2.2 |
| Egg | 1 pc (50 gm) | 0 |
| Dinner | ||
| Menu | Quantity | Carbohydrate |
| Roti | 2 pc (50 gm) | 34.7 |
| Sabji | 1 bowl (100 gm) | 5.l |
| Salad | 1 plate (100 gm) | 3.7 |
| Daal | 1 bowl (80 gm) | 17.2 |
| Teesi | 4 tsp (20 gm) | 5.7 |
| Milk | 1 cup (150 ml) | 6.6 |
Table 6: Health diet of a human.
She was taught insulin techniques and an illustration of the same was handed over to her for reference. The sick day rules were discussed and given to her in written format.
Proper education of self-care must be given to the child so that the child can cope with his/her existing disease, maintain self-confidence, ensure self-management, and adapt with life at large. There has been evidences that recommend exercise for all children and adolescents with type 1 diabetes with the goal of 60 min of moderate to vigorous intensity aerobic activity daily, with vigorous muscle-strengthening and bone-strengthening activities at least 3 days per week (Centers for disease control and prevention. However, stringent monitoring should be achieved by educating the family as well as the patient about frequent patterns of glycaemia during and after exercise, which may include initial transient hyperglycemia followed by hypoglycemia, the prevention and management (with a pre-exercise glucose level of 90 mg/dl-250 mg/dl) of which should be taught, and provision of accessible carbohydrates before, during, and after engaging in activity should be individualized according to the type/intensity of the planned physical activity.
At the end of the interactive session, the child was educated about her daily routine and the need of support from her family to see the treatment through. The DAWN2 study necessitates the involvement of family members for the improvement of glycemic control especially in treating an adolescent girl-child. Both the parents were requested to join the team for a shared decision-making session, the third step towards the diabetes care approach [24].
Shared decision making
Women with type 1 diabetes are wrongly perceived as sick, disabled, dependent persons with reduced life expectancy, unsuitable for marriages and likely to have complicated pregnancies with the possibility of having children with diabetes.
The major challenges remain in the development of approaches to the prevention and management of T1DM and its complications. This would need regular interaction between parents, doctor, and the child, which must be assured for close monitoring.
During the session with the child and her parents, it was emphasized how contribution of mother and father carves an essential niche of cure in the progress of a successful treatment. The appropriate balance between adult supervision and independent self-care should be defined at the first interaction and re-evaluated at subsequent visits. The aspect of following a set pattern of lifestyle modifications were laid down at the beginning of the session, with a special emphasis on the “tripod” of effective diabetes care: diet, exercise, and a proper insulin regimen. The plan, likewise, was explained and the different options of dietary and lifestyle modifications were discussed, according to the needs, dietary choices, socio-cultural and economic aspects of the family. It was essential to actively include the father during the decision-making process, to counter his hesitancy in getting his girl-child treated. Attention to family dynamics, is essential in developing and implementing an optimal diabetes treatment plan.
The father was asked to pay his child some amount of money for the work she did in their cottage industry. This would make her independent. Diabetes self-management education and support requires periodic reassessment, especially as the youth grows, develops, and acquires the need for greater independent self-care skills. A shared decision-making regarding the adoption of regimen components and self-management behaviors can improve diabetes self-efficacy, adherence, and metabolic outcomes.
Plan for future
Type 1 diabetes mellitus can still be a death sentence for some patients if they, or their family, are unable to purchase insulin.
The practice of “insulin rationing” is highly dangerous for people with type 1 diabetes. This has been especially seen in lowincome families where the main earning member is uneducated. The girl-child suffers due to stiff rules of the household where she is expected to run errands, irrespective of her health condition. She is usually married off early, the family unbeknownst of the grave disease only the child is privy to. The chances of unsuccessful marriages are also high in case of arranged marriages, especially among girls. Reluctance in getting the girl-child treated, before or after marriage, usually arises from the need of a woman to run the family, without whom the household comes to a standstill. Diabetes is a social taboo and is a “flaw” especially in women in rural India.
It is important to look for depressive symptoms, and individual perception of sexuality. Future partners should be acknowledged about the problems and management of diabetes. The common myth of diabetes to be a communicable disease should be removed from the minds of people involved in care of the girl-child. Along with the patient, her family should know the complications of the disease and how to deal with the same. The diabetes care team must be capable of evaluating the educational, behavioral, emotional, and psychosocial factors that impact implementation of a treatment plan and must work with the individual and family to overcome barriers.
The primary care giver should be as well informed as the patient herself. Insulin regimen should not be missed, and all doses should be taken as prescribed by the doctor to prevent fatal episodes of ketoacidosis. Such challenges of adverse complications are not global but specific to developing countries. This coup d’état is due to a differential distribution of insulin, blocking the resource to poor sections of the society. Weak health systems, poor access to health facilities, health care delivery of diabetes care and pricing are all impeding access to insulin. Remote rural, uneducated areas of developing countries are the most vulnerable zones, of which the female sections are most prone to the catastrophe of complications due to inaccessibility to healthcare.
The patient, a meagre girl-child of just 18 years, is the victim of the same. She belongs to the disadvantaged sections amongst those already impoverished. Women are more likely to report difficulties in visiting the doctor than men because they are more likely to be housebound. All of which eventually leads to an inability to get access to adequate treatment.
The social apathy towards the girl-child, absence of government funded insulin dosage for the poor and gross illiteracy in the weaker sections of resource limited areas in rural India contribute to an impaired cause-treatment follow up and care.
The team tried to bridge the gap by education and provision of resources. An individualized approach along with team interaction with the family brought the whole session to a fruitful conclusion.
The father agreed to comply with the needs of his girl-child. Free insulin cartridges with insulin pens were provided by the clinic until SB was fit enough to resume her daily work of bangle making.
There should be a lead to ensure comprehensive clinical and psychological care for all children with T1DM. The final aim of all such programs should be that no child should die of diabetes.
Aim of the diabetes care program is to push boundaries beyond the privileged urban section into the darkness of illiteracy and poverty of rural India. Wide disparities in socioeconomic levels and educational background need to be sealed with provision of care to those living with diabetes.
The team started with a girl-child from underprivileged sections, and shall move deeper to attain a sustainable treatment plan for families living in poverty who must also budget to feed, clothe and care for their families.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mukherjee S, Mukherjee B (2023) Inequalities Galore: A Girl with T1DM and Repeated Diabetic Ketoacidosis. Endocrinol Metab Syndr. 12:377.
Received: 05-Jan-2023, Manuscript No. EMS-23-21273 ; Editor assigned: 09-Jan-2023, Pre QC No. EMS-23-21273 (PQ); Reviewed: 23-Jan-2023, QC No. EMS-23-21273 ; Revised: 16-Mar-2023, Manuscript No. EMS-23-21273 (R); Published: 23-Mar-2023 , DOI: 10.35248/2161-1017.23.12.377
Copyright: © 2023 Mukherjee S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.