Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 2
Infantile neuroblastoma is a rare but significant pediatric malignancy arising from neural crest cells. This case report presents the diagnosis, management and prognosis of a 14-month-old male infant diagnosed with infantile neuroblastoma. The report emphasizes the importance of prompt diagnosis, multidisciplinary management and longterm follow-up in achieving favorable outcomes for patients with this condition. Continued research and innovation are critical in advancing our understanding of neuroblastoma biology and improving therapeutic outcomes for affected children. Liver Transplantation (LT) is the only lifesaving option. The etiology is indeterminate in almost 50% cases. Recurrent ALF with intermittent complete recovery may be caused by infections.
Infantile neuroblastoma; Pediatric malignancy; Neural crest cells; Metastasis
Neuroblastoma is the most common extracranial solid tumor in infants and young children, accounting for approximately 7%-10% of all childhood cancers. It arises from neural crest cells and predominantly affects children under the age of five years. While neuroblastoma can occur at various sites along the sympathetic nervous system, including the adrenal glands, para spinal ganglia and abdomen, infantile neuroblastoma specifically refers to tumors diagnosed within the first 18 months of life. Here, we present a case of infantile neuroblastoma highlighting its clinical features, diagnostic modalities, therapeutic interventions and long-term prognosis. However, few infantile neuroblastoma patients relapse and die of the disease. In view of this heterogeneity, understanding the characteristics of this particular pediatric tumor is crucial in choosing the appropriate therapy for individual patients.
We describe the case of a 14-month-old male infant who presented to our pediatric oncology clinic with a two-week history of irritability, poor feeding and abdominal distension. Physical examination revealed a palpable mass in the right upper quadrant of the abdomen, extending into the right flank region. The mass was firm, non-tender and associated with mild hepatomegaly. There were no palpable lymph nodes or other signs of metastasis.
Diagnostic workup
Given the clinical suspicion of a retroperitoneal mass, our diagnostic workup included imaging studies and laboratory investigations. Abdominal ultrasonography revealed a large heterogeneous mass arising from the right adrenal gland, measuring approximately 8 cm in diameter. Further characterization with contrast-enhanced Computed Tomography (CT) confirmed the presence of a solid, enhancing mass consistent with neuroblastoma (Figure 1).
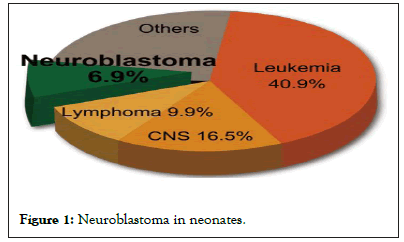
Figure 1: Neuroblastoma in neonates.
Laboratory investigations demonstrated elevated levels of urinary catecholamines, specifically Homovanillic Acid (HVA) and Aanillylmandelic Acid (VMA), indicative of catecholamine-secreting tumors such as neuroblastoma. Bone marrow aspiration and biopsy were performed to evaluate for bone marrow involvement, which was negative [1].
Treatment and management
Multidisciplinary management involving pediatric oncologists, surgeons, radiation oncologists and specialized nursing staff was initiated promptly following the diagnosis of infantile neuroblastoma. The patient was staged according to the International Neuroblastoma Staging System (INSS) as stage 2A, indicating a localized tumor with incomplete resection [2].
Given the size and location of the tumor, the patient underwent neoadjuvant chemotherapy with a regimen consisting of Vincristine, Doxorubicin and Cyclophosphamide (VDC). This was followed by surgical resection of the primary tumor, which achieved gross total resection with negative surgical margins [3].
Postoperatively, the patient received further chemotherapy with a multidrug regimen including Cisplatin, Etoposide and Ifosfamide (PEI), aimed at eradicating residual disease and preventing recurrence. Serial imaging studies and surveillance assessments were performed to monitor treatment response and detect any evidence of disease progression or relapse.
Intervention in infantile neuroblastoma
Infantile neuroblastoma is a rare form of cancer that affects infants and young children, typically under the age of two. Neuroblastoma arises from immature nerve cells found in various parts of the body, most commonly in the adrenal glands, which are located above the kidneys. While the exact cause of neuroblastoma remains unknown, it is believed to result from genetic mutations during fetal development.
The interventions for infantile neuroblastoma depend on several factors, including the tumor's size, location and whether it has spread to other parts of the body. Treatment strategies often involve a multidisciplinary approach and may include surgery, chemotherapy, radiation therapy and other targeted therapies.
Surgery is often the primary intervention for neuroblastoma, especially when the tumor is localized and can be safely removed without causing significant damage to surrounding tissues. Surgeons aim to excise as much of the tumor as possible while preserving important organs and structures.
Chemotherapy is frequently used to shrink the tumor before surgery, making it more manageable to remove. It may also be administered after surgery to eradicate any remaining cancer cells and reduce the risk of recurrence. Chemotherapy drugs are delivered either orally or intravenously and work by targeting rapidly dividing cancer cells throughout the body.
Radiation therapy utilizes high-energy beams to destroy cancer cells and shrink tumors. It may be employed in cases where the tumor is to target residual cancer cells following surgery.
In cases where neuroblastoma has spread to other parts of the body, such as the bones, bone marrow or lymph nodes, additional interventions may be necessary. This could include targeted therapy, immunotherapy or stem cell transplantation, depending on the specific characteristics of the tumor and the patient's overall health.
Targeted therapies aim to disrupt specific molecular pathways involved in cancer growth and progression. Immunotherapy utilizes the body's immune system to recognize and attack cancer cells, while stem cell transplantation may be considered to replenish the bone marrow following high-dose chemotherapy.
The choice of intervention and treatment plan for infantile neuroblastoma is highly individualized and may evolve over time based on the child's response to therapy and any changes in the disease's progression. Close collaboration between pediatric oncologists, surgeons, radiation oncologists and other specialists is essential to ensure the best possible outcomes for children diagnosed with this challenging condition. Early detection, advances in treatment modalities and ongoing research into the underlying biology of neuroblastoma offer hope for improved outcomes and quality of life for affected children and their families.
Follow-up and prognosis
The patient responded favorably to multimodal therapy, with significant reduction in tumor size and resolution of symptoms. Subsequent imaging studies demonstrated no evidence of residual disease or distant metastasis. Long-term follow-up is essential to monitor for late effects of treatment, including potential neurocognitive and psychosocial sequelae, as well as to detect any recurrence or late relapse of the disease [4,5].
The prognosis for infantile neuroblastoma varies depending on several factors, including age at diagnosis, stage of disease, tumor biology and response to therapy. While localized tumors generally have a favorable prognosis with high rates of long-term survival, advanced-stage disease and unfavorable biological features confer a poorer prognosis with increased risk of recurrence and metastasis.
Infantile neuroblastoma represents a distinct subset of neuroblastoma characterized by unique clinical and biological features. Early diagnosis, accurate staging and appropriate risk stratification are crucial in guiding therapeutic decisions and optimizing outcomes for patients with this condition. The role of multimodal therapy, including surgery, chemotherapy and radiation therapy, has evolved over time with the aim of achieving maximal tumor control while minimizing treatment related morbidity and long-term sequelae [6].
Recent advances in molecular profiling and targeted therapy hold promise for improving risk stratification and tailoring treatment approaches based on individual tumor biology. Ongoing research efforts aimed at unraveling the molecular pathogenesis of neuroblastoma may lead to the development of novel therapeutic agents and personalized treatment strategies in the future.
Infantile neuroblastoma is a rare but significant pediatric malignancy associated with distinct clinical and biological characteristics. Multidisciplinary collaboration and comprehensive management are essential in achieving optimal outcomes for patients diagnosed with this condition. Long-term follow-up is necessary to monitor for late effects of treatment and detect any evidence of disease recurrence or late relapse. Continued research and innovation are critical in advancing our understanding of neuroblastoma biology and improving therapeutic outcomes for affected children. Acute Liver Failure (ALF) in children is a life-threatening complication, and the prognosis is often guarded. Sometimes, Liver Transplantation (LT) is the only lifesaving option. The etiology is indeterminate in almost 50% cases. Recurrent ALF with intermittent complete recovery may be caused by infections, immunological diseases, toxins and metabolic liver diseases such as fructose intolerance, mitochondrial energy defects such as respiratory chain disorders, fatty acid oxidation defects and carnitine cycle.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kumar R, Watson L, Willington A (2024) Infantile Neuroblastoma: A Long Term Follow-up and its Significance in Pediatric Malignancy. Clin Pediatr. 09:262.
Received: 22-Feb-2024, Manuscript No. CPOA-24-29844; Editor assigned: 26-Feb-2024, Pre QC No. CPOA-24-29844 (PQ); Reviewed: 11-Mar-2024, QC No. CPOA-24-29844; Revised: 18-Mar-2024, Manuscript No. CPOA-24-29844 (R); Published: 25-Mar-2024 , DOI: 10.35248/2572-0775.24.09.262
Copyright: © 2024 Kumar R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.