Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 2
Infantile pyknocytosis is a rare blood disorder that primarily affects newborns and infants. Characterized by the presence of abnormal red blood cells called pyknocytes, this condition can cause mild to severe symptoms, including anemia and jaundice. While infantile pyknocytosis is typically benign and self-limiting, understanding its causes, symptoms and management is crucial for proper diagnosis and care. Diagnosis is exclusively based on the detection of a higher proportion of pyknocytes in peripheral blood smear. IP is a self-restricted disease. In this case series study we present the diagnostic approach. IP should be included in the differential diagnosis in case of prolonged neonatal jaundice not well explained by other common of hemolytic anemia.
Jaundice; Anemia; Irritability; Poor weight gain
Infantile pyknocytosis is a rare cause of neonatal jaundice associated with transient hemolytic anemia, with a favorable outcome after 4 to 6 months. Diagnosis is based on cytology that usually shows numerous pyknocytes and exclusion of other causes. Pathophysiology is unclear and probably involves oxidative stress, as illustrated by this case with numerous Heinz bodies. IP is a self-restricted disease. In this case series study we present the diagnostic approach, therapeutic intervention and outcome of two neonates, presented with unconjugated hyperbilirubinemia and major hemolysis. Infantile Pyknocytosis (IP) is responsible for 10% of neonatal anemia cases with unidentified etiology. The disease is characterized by the presence of pyknocytes in the peripheral blood smear. Pyknocytes were initially described as much distorted, completely irregular, densely stained erythrocytes, usually appreciably smaller than the undistorted cells and having several spiny projections.
Infantile pyknocytosis
Infantile pyknocytosis, also known as familial hypoketotic pyknocytosis, is a hematological disorder characterized by the presence of pyknocytes in the bloodstream. Pyknocytes are abnormally small and dense red blood cells with irregular shapes. These cells can be observed under a microscope in blood smear (Figure 1).
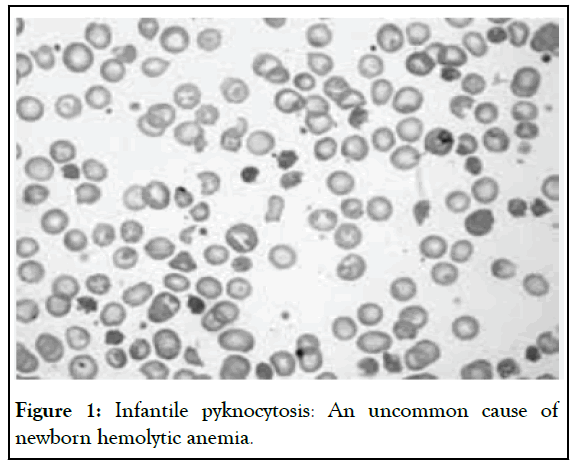
Figure 1: Infantile pyknocytosis: An uncommon cause of newborn hemolytic anemia.
This condition is most commonly diagnosed during the first few months of life, typically within the first three months after birth.
While the exact prevalence of infantile pyknocytosis is unknown, it is considered rare, with only a small number of cases reported worldwide.
Symptoms of infantile pyknocytosis
Infantile pyknocytosis can present with a range of symptoms, which can vary in severity from mild to severe. Common symptoms may include:
Jaundice: Yellowing of the skin and whites of the eyes due to elevated levels of bilirubin in the blood. Jaundice is often one of the first noticeable symptoms of infantile pyknocytosis.
Anemia: A decrease in the number of red blood cells or hemoglobin levels, leading to fatigue, pale skin and weakness. Anemia may be mild or severe, depending on the extent of red blood cell destruction.
Enlarged spleen: Some infants with infantile pyknocytosis may develop an enlarged spleen (splenomegaly) due to the increased breakdown of red blood cells within the organ.
Poor weight gain: Infants may experience difficulty gaining weight or fail to thrive due to the effects of anemia and decreased oxygen delivery to tissues.
Irritability: Babies with infantile pyknocytosis may appear fussy or irritable, particularly if they are experiencing symptoms such as anemia or jaundice.
It's essential to note that not all infants with infantile pyknocytosis will experience all of these symptoms and the severity of symptoms can vary widely among affected individuals.
Causes of infantile pyknocytosis
The exact cause of infantile pyknocytosis is not fully understood. However, it is believed to be an inherited condition with an autosomal dominant pattern of inheritance. This means that a child only needs to inherit one copy of the mutated gene from either parent to develop the disorder.
The genetic mutation associated with infantile pyknocytosis affects the structure and function of proteins involved in red blood cell production and maintenance. As a result, red blood cells produced by affected individuals are more prone to abnormalities, including the formation of pyknocytes.
Diagnosis
Diagnosing infantile pyknocytosis typically involves a combination of clinical evaluation, blood tests and microscopic examination of blood smears. A healthcare provider may suspect infantile pyknocytosis based on the presence of characteristic symptoms such as jaundice and anemia in a newborn or young infant [1-3].
Blood tests, including a Complete Blood Count (CBC) and peripheral blood smear, can reveal abnormalities such as low hemoglobin levels, elevated reticulocyte count (indicating increased red blood cell production) and the presence of pyknocytes in the bloodstream.
In some cases, additional tests may be performed to rule out other potential causes of symptoms, such as hemoglobinopathies or enzymatic deficiencies.
Treatment and Management
Infantile pyknocytosis is typically a self-limiting condition, meaning that it often resolves on its own without the need for specific treatment. However, supportive care may be provided to manage symptoms and complications associated with the disorder.
Phototherapy: For infants with jaundice, phototherapy may be recommended to help lower bilirubin levels in the blood. This involves exposing the baby's skin to special lights that help break down bilirubin and facilitate its excretion from the body.
Monitoring: Close monitoring of the baby's health is essential to ensure that symptoms such as anemia and jaundice are properly managed. This may involve regular blood tests to assess hemoglobin levels [4].
Blood transfusion: In severe cases of anemia or hemolysis (destruction of red blood cells), a blood transfusion may be necessary to replenish red blood cell levels and improve oxygen delivery to tissues. However, blood transfusions are typically reserved for cases where symptoms are severe or life-threatening.
Nutritional support: Ensuring adequate nutrition is essential for infants with infantile pyknocytosis, particularly if they are experiencing poor weight gain or failure to thrive. Breastfeeding or formula feeding may be supplemented with additional nutrients as needed.
Follow-up care: Regular follow-up appointments with a healthcare provider are important to monitor the baby's growth, development and overall health. This allows for early detection of any complications and adjustments to the treatment plan as necessary [5].
The prognosis for infants with infantile pyknocytosis is generally favorable. In most cases, the condition resolves spontaneously within the first few months of life as the baby's red blood cell production and metabolism mature [6].
While some infants may experience recurrent episodes of anemia or jaundice, particularly during periods of illness or stress, the long-term outlook for individuals with infantile pyknocytosis is typically excellent, with no lasting effects on health or development.
Infantile pyknocytosis is a rare blood disorder characterized by the presence of abnormal red blood cells called pyknocytes. While the exact cause of the condition is not fully understood, it is believed to be inherited in an autosomal dominant manner.
Symptoms of infantile pyknocytosis may include jaundice, anemia, enlarged spleen, poor weight gain and irritability, diagnosis is based on clinical evaluation.
Infantile pyknocytosis remains a rare but clinically significant hematologic disorder affecting newborns and infants. Characterized by the presence of abnormally shaped red blood cells, this condition can lead to anemia, jaundice and other complications if left untreated.
While the exact etiology of infantile pyknocytosis remains uncertain, early recognition and diagnosis are essential for initiating appropriate management strategies. With advancements in diagnostic techniques and treatment modalities, healthcare providers can effectively manage this condition and improve outcomes for affected infants.
Further research into the underlying mechanisms of infantile pyknocytosis is warranted to enhance our understanding of the disorder and develop targeted therapeutic interventions. By raising awareness and promoting collaboration among researchers and healthcare professionals, we can strive to improve the quality of care for infants with pyknocytosis and ultimately enhance their long-term prognosis and quality of life.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Saeidian H (2024) Infantile Pyknocytosis: The Presence of Abnormal Erythrocytes in Newborn and Infant. Clin Pediatr. 09:265.
Received: 23-Feb-0004, Manuscript No. CPOA-24-30274 ; Editor assigned: 26-Feb-2024, Pre QC No. CPOA-24-30274 (PQ); Reviewed: 11-Mar-2024, QC No. CPOA-24-30274 ; Revised: 18-Mar-2024, Manuscript No. CPOA-24-30274 (R); Published: 25-Mar-2024 , DOI: 10.35248/2572-0775.24.09.265
Copyright: © 2024 Saeidian H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.