
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2021)Volume 12, Issue 7
Background: Hypotension is a common side effect of general anaesthesia, and when severe, it may lead to adverse outcomes. Ultrasonography of Inferior Vena Cava (IVC) is an effective, non-invasive method of assessment of intravascular volume status and hence the risk of hypotension at induction of anaesthesia. This study investigated whether preoperative ultrasound guided IVC measurements could predict hypotension after induction of anaesthesia.
Methods: After ethical committee approval, this study was conducted at Sri Ramakrishna Hospital, Coimbatore. Written and informed consent was obtained. Forty six (46) adult patients, conforming to American Society of Anaesthesiologists physical status I to II, scheduled for elective surgery under general anaesthesia were recruited. Maximum IVC Diameter (dIVCmax) and Collapsibility Index (CI) were measured preoperatively. Before induction, Mean Blood Pressure (MBP) was recorded. After induction, MBP was recorded for 10 consecutive minutes. Hypotension was defined as greater than 30% decrease in MBP from baseline or MBP less than 60 mmHg.
Results: IVC could not be visualized in 6 patients. Data from remaining 40 patients were analysed, of whom 26 patients (65%) developed hypotension. The incidence of hypotension in patients with CI>40% was 100% and when CI<40% it was 4%. The mean value of IVC maximum diameter was 1.60 cm and the mean value of IVC minimum diameter was 1.02 cm. The optimal cut-off value was 40% for CI among the patients who developed hypotension. CI was positively associated with a percentage decrease in MBP.
Conclusion: Preoperative ultrasound IVC-CI measurement is a reliable predictor of hypotension after induction of general anaesthesia, and CI greater than 40% was highly significant in causing post induction hypotension.
COVID-19; CVT; Hypercoagulability; Stroke; Homocysteinemia
Hypotension is common during surgery in patients under anesthesia and may cause organ hypo perfusion and ischemia [1,2]. A surgical patient’s preoperative volume status may vary due to physical status, comorbidities, and preoperative treatment such as bowel preparation and fasting, time gap between fasting and onset of surgeries, to mention a few [3,4]. Severe episodes of intraoperative hypotension have been proposed as an independent risk factor in the development of postoperative adverse outcomes such as myocardial infarction, stroke, heart failure, acute kidney injury, prolonged hospital stay, and even increased 1-yr mortality rates both in patients undergoing cardiac surgery and noncardiac surgery [5-18].
Ultrasound has revolutionised the practice of medicine and reduced the need for invasive procedures for assessment and diagnosis of several conditions. Ultrasound measurements of Inferior Vena Cava (IVC) diameter with respiration, which includes (1) Maximum Diameter of the IVC (dIVCmax) at the end of expiration during spontaneous respiration
(2) Collapsibility Index (CI), have been recommended as a rapid and non-invasive method for estimating volume status [17,18]. These parameters have been proposed as repeatable and easily obtainable parameters by operators with little experience in echocardiography [12-18].
Ultrasound measurement of the IVC reflects volume status more closely than other parameters based on arterial system analysis such as blood pressure, pulse rate, diameter of aorta, and others. Several studies have demonstrated dIVC max and CI as reliable indicators of intravascular volume status [19-22].
Therefore, we hypothesized that preoperative dIVCmax and its respiratory variation, that is, Collapsibility Index (CI), could predict the incidence of hypotension after induction of general anaesthesia, with a high degree of sensitivity and specificity [22-25].
Aim
The aim of this study was to establish a correlation between the IVC diameter and collapsibility index with the incidence of hypotension following general anaesthesia in elective surgeries.
Objective
Primary objective: To assess the volume status of the patient before induction of general anaesthesia by using IVC ultrasonography, and predict the risk of hypotension in the immediate post induction period.
Secondary objective: To correlate the collapsibility index of IVC with that of hypotension.
This prospective observational study was conducted at Sri Ramakrishna Hospital, Coimbatore, from January 2018 to June 2018.
Inclusion criteria
Patients undergoing elective surgery under general anaesthesia, aged between 18 to 60 years, BMI between 18-30, ASA Grade I and II, and who provided consent were included in the study.
Exclusion criteria
1. Patient refusal to consent.
2. Patients with acute abdomen like appendicitis, intestinal obstruction, pancreatitis, ascites etc.
3. Pregnant patients.
4. Patients with implanted pacemaker/cardioverter.
5. Patients with pre-existing hemodynamic instability, ventricular dysfunction and sepsis.
6. Patients with major peripheral vascular disease, severe vascular disease, ejection fraction <40%.
Sample size
The retrospective data is used to estimate the population size and its proportional variance the retrospective data states that the existing population is 50 and one-year proportion is calculated for prospective data with expected margin of error.
The following formula is used to estimate the sample size (n).
The values given to compute the sample size is as follows; Margin of Error (E)=5 %
Confidence level (Z)=95%,
Population (N)=50
Sample proportion (r)=10%.
Therefore, obtained sample size is 36, by substituting in the above formula. For ease of calculations and sake of consistent result, sample size has been taken as 46. And not in all patients IVC can be easily visualized, so an arbitrary number of 10 have been added to the sample size to avoid procedural bias.
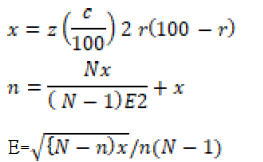
After obtaining the approval of institutional ethical committee and written informed consent from every patient, a total of 46 patients undergoing non abdominal surgery under general anaesthesia were included in the study (Figure 1). Universal fasting guidelines were followed.
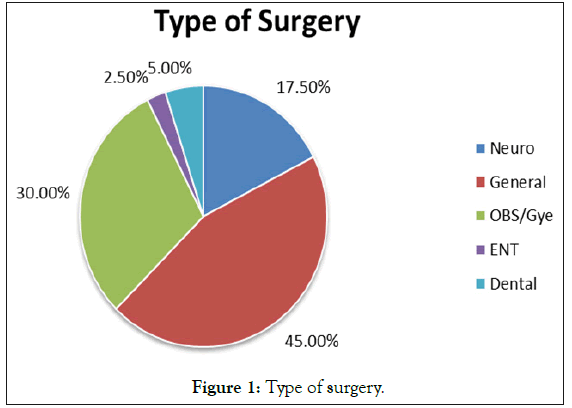
Figure 1: Type of surgery.
Patients were received in the preoperative area with an intravenous access in situ (18 G or 20 G).All patients enrolled in study were premedicated with intravenous midazolam at a dose of 0.01 mg/ kg to relieve anxiety.
The procedure of ultrasonographic assessment of the IVC was explained to the patient and the area prepared in the presence of a chaperone. They were then under observation in the preoperative receiving area for duration of 10 minutes.
IVC ultrasonography
All patients were conscious, lying supine, and spontaneously breathing for 10 minutes before IVC examination. Ultrasound measurements were performed using a GE machine and a 3 To 5 Hz curved linear phased array transducer (GE Inc.) set to abdominal mode. All IVC measurements were performed by primary operator who had basic level 1 experience in echocardiography. The IVC was visualized using a paramedian long-axis view via a subcostal approach according to the methodology described by the American Society of Echocardiography. A two-dimensional image of the IVC as it entered the right atrium was first obtained. Pulse wave Doppler was used to differentiate the IVC from the aorta.
Variations in IVC diameter with respiration were measured using M-mode imaging, performed 2 to 3 cm distal to the right atrium [26-30]. The M-mode image was generated at a medium sweep speed. To ensure consistent IVC measurements, three scans were performed in each patient. If there was a difference of more than 0.2 cm in dIVCmax measurements between any two of the images, then that patient’s data were excluded from the study. The whole IVC scan procedure took less than 10 min. For each patient, the best quality scan image was chosen. Maximum and minimum IVC diameters over a single respiratory cycle were measured manually. The CI was calculated as CI=(dIVCmax–dIVCmin)/dIVCmax and was expressed as percentage. After assessing IVC diameter and collapsibility index, patients were shifted inside operation theatre.
Anesthesia management
All patients involved in study were attached with ASA standard monitors including electrocardiogram (ECG), Non-Invasive Blood Pressure (NIBP), peripheral oximeter readings (SpO2), end-tidal carbon dioxide (etCO2), and airway pressures were monitored. Normal saline or Ringer lactate infusion was started at a rate of 10 ml/kg.
After preoxygenation, patients were induced using a regimen of 2 mcg/kg fentanyl followed by 2 mg/kg propofol. Tracheal intubation was facilitated using a nondepolarizing muscle relaxant, atracurium 0.5 mg/kg. The Mean Blood Pressure (MBP) reading immediately before induction was defined as baseline. Patients with a baseline MBP lower than 70 mmHg were excluded.
Blood pressure was recorded during the postinduction study period for 10 consecutive minutes; Patients remained supine throughout the study, and only mild-level stimulation, such as urinary catheterization and surgical area prepping, was allowed. No airway manipulation or endotracheal intubation was done during the 10 minutes study period, to avoid hemodynamic alteration to intubation response. Severe (i.e., MBP less than 55 mmHg) or prolonged (i.e., duration greater than or equal to 2 min) episodes of hypotension was treated with intravenous boluses of ephedrine (3 mg) or phenylephrine (100 μg). Atropine (0.6 mg) was used for significant bradycardia (HR less than 40 beats/min). Episodes of hypotension in the period after induction of anesthesia were defined by a more than 30% decrease in MBP from the baseline level or any recorded MBP lower than 60 mmHg.
Statistical analysis
Statistical Package for Social Sciences (SPSS) version 20 was employed to analyze data. Continuous data will be analyzed for its mean, median and standard deviation (summary statistics). Categorical variables will be analyzed using chi-square test and ‘p’ value of ≤ 0.05 will be considered as statistically significant.
Out of 46 patients enrolled in our study, IVC could not be identified clearly and respiratory variations could not be calculated with ease in 6 patients (13%), so they were excluded from the study. There were 25 female and 15 male participants taking part in the study with a mean age of 44.95 (Figure 2).
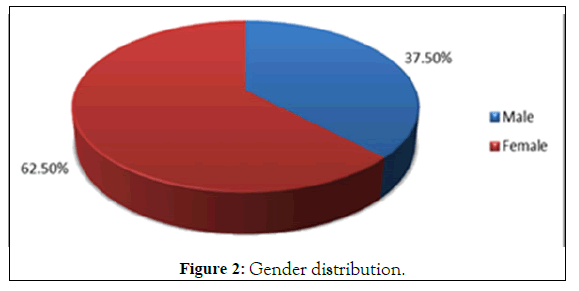
Figure 2: Gender distribution.
Parameters assessed
Preoperatively using ultrasonography, the IVC diameter (maximum and minimum) was recorded during a single breath. Post induction, the mean arterial blood pressure was recorded every minute for the first 10 minutes following induction. The maximum MBP prior to induction was 126 mm of Hg and minimum MBP prior to induction was 84 mm of Hg and its mean value among 40 patients were 97 mm of Hg with a standard deviation of 10.86. The maximum IVC diameter during expiration was 2.21 cm and minimum IVC diameter during expiration was 0.97 cm and its mean value among 40 patients was 1.60 cm with standard deviation of 0.34 (Table 1). The Maximum IVC diameter during inspiration was 1.33 cm and minimum IVC diameter during inspiration was 0.56 cm and its mean value among 40 patients was 1.03 cm with standard deviation of 0.22. The Maximum Collapsibility Index was 61% and minimum Collapsibility Index was 12% and its mean value among 40 patients were 34% with standard deviation of 0.13. Hypotension and its Incidence: Out of 40 patients involved in study, 26 patients developed hypotension which was defined as more than 30% decrease in MBP from the baseline level or any recorded period of MBP lower than 60 mmHg (Figures 3–5).
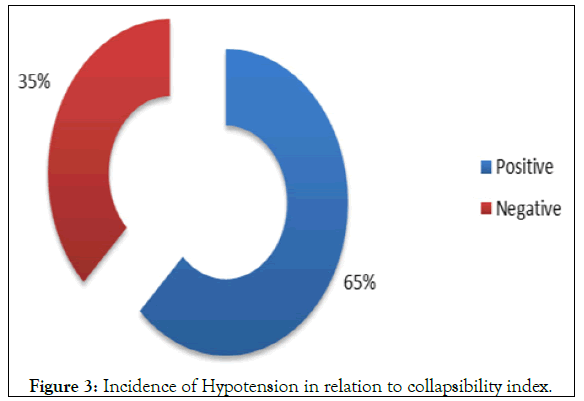
Figure 3: Incidence of Hypotension in relation to collapsibility index.
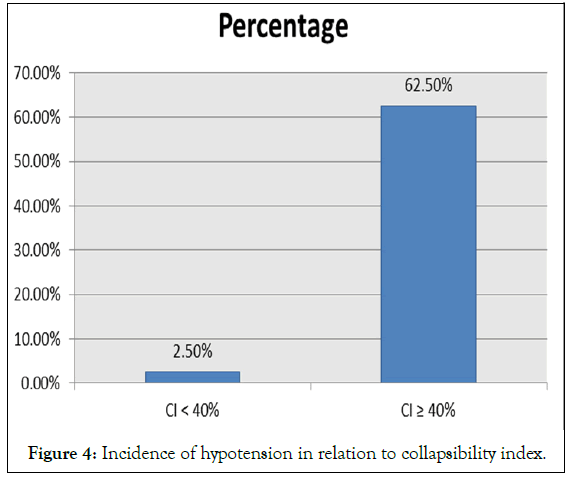
Figure 4: Incidence of hypotension in relation to collapsibility index.
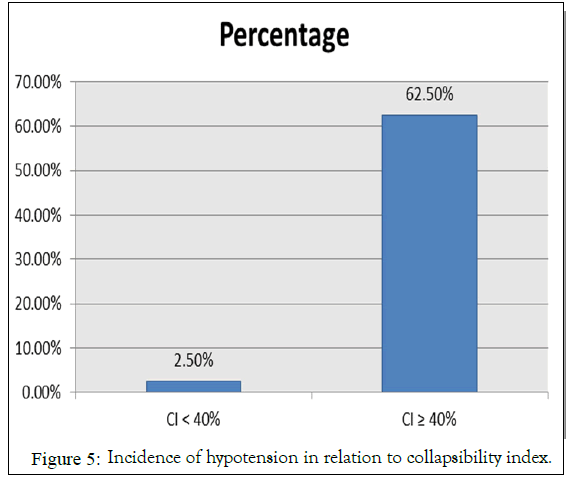
Figure 5: Incidence of hypotension in relation to collapsibility index.
| Mean | SD | |
|---|---|---|
| IVC max | 1.6 | 0.34 |
| IVC min | 1.03 | 0.22 |
| CI | 34% | 0.13 |
| MBP prior | 97.03 | 10.86 |
Table 1: Parameters assessed: IVC diameter in cms.
Co-relation between collapsibility index and hypotension
Among the 26 patients who developed hypotension, it was characteristically noted that 25 of these patients had a Collapsibility Index (CI) of 40% and above (Table 2). Similarly in those 14 patients, who did not develop hypotension for 10 consecutive minutes after induction, their Collapsibility Index (CI) was less than 40%; with exception being 1 patient whose collapsibility index which was 38% (Figure 4). We have observed that patients with an IVC-CI ≥ 40% had 100% incidence of post induction hypotension, whereas when the IVC-CI was less than 40%, the occurrence of hypotension was only 4%.
| Incidence of hypotension | No. of cases | Percentage |
|---|---|---|
| Positive | 26 | 65% |
| Negative | 14 | 35% |
| Total | 40 | 100.00% |
Table 2: Incidence of hypotension.
Hypotension on induction of anaesthesia is nearly inevitable. It has been recognized as an anticipated side effect of general anaesthesia. In the emergency department, post intubation hypotension is considered an adverse event with an incidence of 60%. It has been linked to increased length of stay in the ICU, post-operative requirements for mechanical ventilation and mortality [26]. Various factors have been identified as predictors of significant hypotension in patients scheduled for surgery under general anaesthesia. Among them, induction agent propofol has been found to cause hypotension even when used in small doses [27]. However; propofol still continues to remain as the induction agent of choice in most scenarios including ambulatory and daycare surgeries due to its rapid onset and quick recovery with fewer side effects. It has also been observed that the hypotension caused by propofol is more responsive to fluid boluses rather than administration of vasopressors like ephedrine [28].
Several studies have been identified which observed the effect of IVC ultrasonography in predicting post induction hypotension in adult patients in the emergency department. Krause I evaluated the usefulness of IVC diameter measured by Echocardiography to estimate hydration status in children on haemodialysis [29]. We studied the significance of IVC ultrasonography in patients scheduled for elective surgery. These patients are kept nil per oral as per the fasting guidelines, may have a low volume status and are hence more prone to post induction hypotension.Since overnight fasting can be associated with hypovolemia even in American Society of Anaesthesiologists physical status 1 and 2, an IVC-CI cut off value of 40% was expected to be a better predictor of post induction hypotension.
We observed that 100% of patients with IVC-CI ≥ 40% had post induction hypotension as compared to 4% of patients who had IVC-CI<40%. These results are comparable to previous studies which have predicted the incidence of post induction hypotension in emergency department patients. Our results are similar to the results of the study conducted by Arthur [30]. Where the cut off value for IVC CI was 50% the incidence of hypotension was 76% when the IVC CI>50% and hypotension was defined by a systolic blood pressure <90 mmHg.
The use of ultrasonography in medicine has expanded in the last few decades. Being non-invasive and radiation free are the primary advantages of ultrasound. To quote the American society of Echocardiography, the learning curve for ultrasonography measurements of IVC diameter and Collapsibility Index is fast and can be used by beginners in the emergency department as well as in the operation theatre.
IVC diameter assessment by ultrasound is as reliable as CVP and GEDVI in assessing the preload according to the study conducted [30]. IVC-CI is useful in the management of circulatory failure in patients with septic shock. However, further studies are needed to establish this observation and compare the effect of IVC-CI in hypovolemic shock versus vasodilatory septic shock. This may help reduce the need for invasive monitoring of preload and hence the complications associated with it. Clinically, preoperative CI measurements were easy and rapid (i.e., scan time less than 10 min) to obtain with point-of-care ultrasound becoming moreand- more readily available in anesthesia induction areas. Thus, in patients at high risk of complications resulting from intraoperative hypovolemia and hypotension, measurement of IVC-CI may provide clinically useful information. Based on our observations, we may conclude that ultrasonographic measurements of IVC diameter and Collapsibility Index are very effective in predicting post induction hypotension. This cut off value of 40% for IVCCI is an excellent predictor of identifying patients at risk of post induction hypotension undergoing elective surgeries under general anesthesia with propofol as induction agent.
Thus, we may conclude that preoperative ultrasound guided measurement of IVC diameter and collapsibility index is a reliable predictor of post induction hypotension in ASA I and II patients posted for elective surgeries under general anaesthesia. The threshold for predicting hypotension was a CI greater than 40%. CI was also positively associated with a percentage decrease in MBP after induction. Future research based on CI measurements is needed to determine the best intravenous fluid strategies to reduce postinduction hypotension.
Single centric study
Sample size is small and only ASA I and II patients were included. Hence, the results may not be extrapolated to other patients. We were unable to measure IVC collapsibility reliably after induction because the patient’s ventilation changed from spontaneous to positive pressure. Thus, changes in CI after induction are lacking in the study.
Citation: Jothiprakash VK, Parameswari R, Udayakumar P (2021) Inferior Venacaval Ultrasonography to Detect Pre-Operative Hypovolemia as a Predictor of Postinduction Hypotension. J Anesth Clin Res. 12:1010.
Received: 01-Jul-2021 Accepted: 16-Jul-2021 Published: 23-Jul-2021 , DOI: 10.35248/2155-6148.21.12.1014
Copyright: © 2021 Jothiprakash VK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.