International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research - (2022)
Background: Acute heart failure in-hospital mortality varies between 3.8-28%. The Acute Decompensated Heart Failure National Registry (ADHERE) risk tree is a landmark risk prediction model for in-hospital mortality. This study compares in-hospital mortality predicted by the ADHERE risk tree with the observed mortality of patients from the Pre Heart Failure Clinic (PRECIC-Pré Clínica de Insuficiência Cardíaca) study.
Methods and findings: This is a retrospective, single-centre, observational sub-analysis of the previously reported PRECIC study. The ADHERE risk tree was applied. In-hospital predicted and observed mortality was compared in 419 patients with a mean age of 79.5 years. The majority were female and had left ventricle ejection fraction ≥ 40%. In-hospital mortality was 8.1% (n=34). After being classified in the ADHERE risk groups, the observed mortality rates between 3 groups were significantly different (p<0.001): Low, Intermediate 2, and Intermediate 1 (4.5% vs. 2.3%, p=0.0017; 12.5% vs. 5.6%, p=0.024; and 40% vs. 13.2%, p=0.003, respectively). The observed mortality was twice the predicted mortality in the Low and Intermediate two groups and threefold in the Intermediate 1 group. The small number of patients in the High group impairs solid conclusions to be drawn for this group.
Conclusion: The ADHERE risk tree cannot accurately predict the in-hospital mortality rates of patients with the characteristics of those included in the PRECIC study. This finding supports the need to locally validate risk trees to take into account different patient characteristics and healthcare settings.
Heart failure; Risk groups; In-hospital mortality
AHF: Acute Heart Failure; ADHERE: Acute Decompensated Heart Failure National Registry; HF: Heart Failure; SBP: Systolic Blood Pressure; BUN: Blood Urea Nitrogen; LVEF: Left Ventricle Ejection Fraction;
Acute Heart Failure (AHF) is a leading cause of hospital admission in the elderly, being associated with increased hospital stay and higher risk of mortality [1], and represents a significant burden on overall healthcare costs [2]. A better understanding of this high-risk patient population is therefore needed [3].
In-hospital mortality due to AHF varies between 3.8-28% in developed countries [2,3]. Several mortality predictors have been identified for outpatients with chronic Heart Failure (HF), but few risk-prediction models have been developed specifically for the hospitalised AHF population [3]. The complex pathology, incomplete prospective data, and the different epidemiological characteristics among populations make it very difficult to identify good predictors of in-hospital mortality [2].
Clinical and therapeutic decisions should be tailored to the patient’s risk for adverse outcomes. Although a clinical risk prediction model for in-hospital mortality cannot replace physician assessment, it is beneficial to guide the healthcare strategy based on the anticipated risk of death, optimising the use of healthcare resources and generating better clinical outcomes [2,4,5].
The Acute Decompensated Heart Failure National Registry (ADHERE) is a landmark study that addressed the need for prediction models of in-hospital death risk [5]. The main outcome of the ADHERE study is a risk tree, which provides clinicians with a practical bedside prediction tool for in-hospital mortality for patients hospitalised with AHF. It is based on Systolic Blood Pressure (SBP), serum Blood Urea Nitrogen (BUN), and serum creatinine parameters at the time of admission [5]. The ADHERE study was validated for the USA population, and it remains to be clarified whether its risk model can accurately predict in-hospital mortality in other populations [5].
This study aims to compare in-hospital mortality predicted by the ADHERE risk tree with the observed mortality in a cohort of Portuguese HF patients that have previously been enrolled in the PRECIC study [6].
Study sample and design
This is a retrospective, single-centre, observational study based on a sub-analysis of the previously reported PRECIC study [6]. All patients hospitalised with AHF in the Internal Medicine Department of a large tertiary university hospital for one year were considered for enrolment. Clinical records and telephone interviews were used for data collection. The study was approved by the institutional Ethics Committee, and patient confidentiality was preserved because no direct patient identifiers were collected.
Data collection and in-hospital mortality risk groups
Clinical records were analysed for data collection as previously described [6]. The ADHERE risk tree was applied to all patients based on SBP value and levels of BUN and plasma creatinine at the time of hospital admission. Patients were classified according to the five risk groups of in-hospital mortality of the ADHERE risk tree: High Risk, Intermediate Risk 1, Intermediate Risk 2, Intermediate Risk 3, and Low Risk [5]. Ten patients were excluded from the analysis due to the absence of clinical data needed for model application. All comparisons were made between the PRECIC study population and the ADHERE validation cohort [5]. For this purpose, urea levels were converted into BUN using the following equation: BUN (mg/dL)=urea (mg/dL)/2.14.
Statistical analysis
Baseline characteristics of the PRECIC sample were previously reported [6]. Fisher's exact test and univariate logistic regression model were performed to compare mortality according to the ADHERE risk groups. Chi-square and Fisher's exact test were used to compare the in-hospital mortality rates of this study population with the ADHERE validation cohort [5] in terms of ADHERE risk groups. A level of α=0.05 was used as a boundary for statistical significance in all analyses. Statistical analyses were performed using the statistical software SPSS® IBM® 22.0.
During the PRECIC study period, 429 patients were hospitalised with AHF. Of these, all the required clinical data at admission for stratification according to the ADHERE risk tree was available for 419 patients. The 419 enrolled patients had a mean age of 79.5 years, the majority were female (63.2%), and 74.7% had Left Ventricle Ejection Fraction (LVEF) ≥ 40%. The demographic and clinical characteristics of this study sample are reported together with those from the ADHERE validation cohort (Table 1). Based on the ADHERE risk tree criteria, patients were assigned to the five in-hospital mortality risk groups shown in Figure 1. Two risk groups were underrepresented: the High-risk group, with only 4 patients, and the Intermediate 1 group, with 20 patients.
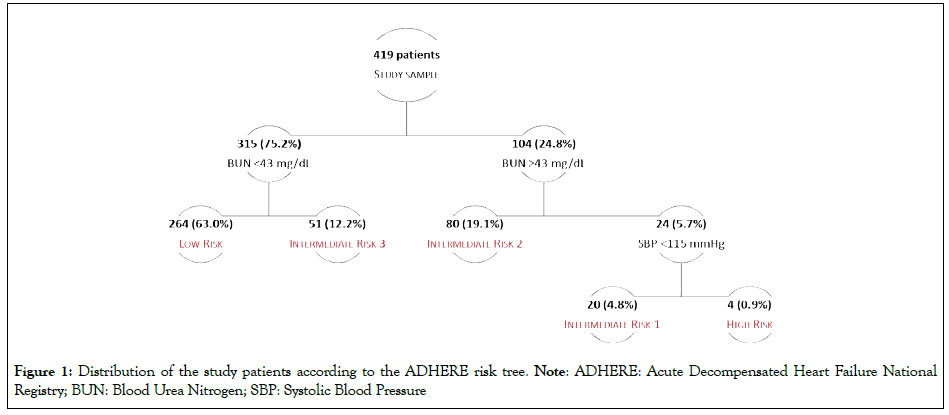
Figure 1: Distribution of the study patients according to the ADHERE risk tree. Note: ADHERE: Acute Decompensated Heart Failure National Registry; BUN: Blood Urea Nitrogen; SBP: Systolic Blood Pressure
| Baseline | Study | ADHERE |
|---|---|---|
| Characteristics | Sample | Validation cohort |
| Demographic variables | ||
| N | 419 | 32 229 |
| Mean age (SD), years | 79.5 (10) | 72.5 (14) |
| White (%) | 100 | 72 |
| Female (%) | 63.2 | 51 |
| Medical history | ||
| Hypertension (%) | 86.4 | 72 |
| Diabetes mellitus (%) | 47.3 | 44 |
| Coronary artery disease (%) | 32 | 56 |
| Atrial fibrillation (%) | 52.7 | 30 |
| Peripheral vascular disease (%) | 11.7 | 18 |
| Active cancer (%) | 8.8 | NA |
| Dementia (%) | 50 | NA |
| Clinical status | ||
| Systolic Blood Pressure(mean, SD, mmHg) | 139.4 (29) | 144.7(32.5) |
| Sodium(mean, SD, mmol/L) | 136.4 (5.8) | 138.3(4.8) |
| Serum creatinine(mean, SD, mg/dL) | 1.3 (0.7) | 1.8(1.7) |
| Blood Urea Nitrogen(mean, SD, mg/dL) | 32.9 (19.2)† | 31.5 (20.8) |
| Haemoglobin(mean, SD, g/dL) | 12 (2.1) | 12.4 (2.6) |
| LVEF ≥ 40% (%) | 74.7 | 47 |
Note: †Blood Urea Nitrogen was converted from urea by the following equation: BUN (mg/dL)=Urea (mg/dL)/2.14;
Abbreviation: ADHERE: Acute Decompensated Heart Failure National Registry; LVEF: Left Ventricle Ejection Fraction; NA: Not Available; SD: Standard Deviation
Table 1: Demographic and clinical characteristics of this study sample and the ADHERE validation cohort.
The observed in-hospital overall mortality was 8.1% (34 deaths). The leading cause of death was cardiovascular: 21 out of 34 deaths (61.8%). The assignment of patients to the ADHERE risk groups revealed significantly different (p<0.001) mortality rates between groups (Table 2) [5]. The mortality Odds Ratio (OR) of the Intermediate 1 and 2 risk groups compared to the Low-risk group were 14.0 and 3.0 (95% CI, 4.82-40.6, and 1.24-7.23), respectively. Due to the small number of patients assigned to the High-risk group (n=4), it was not possible to detect any significant difference between this and the Low-risk group (p=0.103).
| ADHERE risk group | Mortality (%) | OR | 95% CI | p value |
|---|---|---|---|---|
| Low | 4.5 | 1 | - | |
| Intermediate 3 | 5.9 | 1.312 | 0.357-4.827 | 0.682 |
| Intermediate 2 | 12.5 | 3 | 1.244-7.233 | 0.014 |
| Intermediate 1 | 40 | 14 | 4.823-40.639 | <0.001 |
| High | 25 | 7 | 0.677-72.385 | 0.103 |
Note: OR: Odds Ratio; CI: Confidence Interval
Table 2: In-hospital mortality rates, according to ADHERE risk groups.
The overall in-hospital mortality observed in this study (8.1%) was twice that reported in the ADHERE validation cohort (4.0%) [5]. The comparison between in-hospital mortality rates in this study and those reported in the ADHERE validation cohort for each ADHERE risk group also revealed statistically significant differences (Figure 2). Observed and predicted in-hospital mortality was statistically different in three risk groups: Low, Intermediate 2, and Intermediate 1. The mortality rate found in this study was twice that reported in the ADHERE for the Low and Intermediate 2 risk groups and threefold for the Intermediate 1 group.
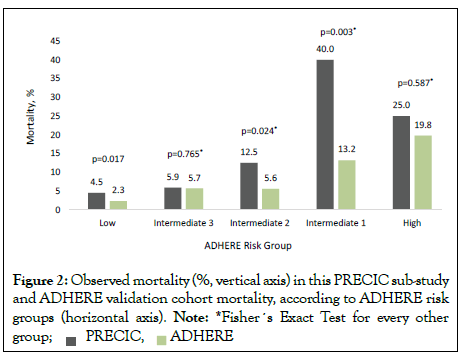
Figure 2: Observed mortality (%, vertical axis) in this PRECIC sub-study
and ADHERE validation cohort mortality, according to ADHERE risk
groups (horizontal axis). Note: *Fisher´s Exact Test for every other
group;
This study found a higher overall in-hospital mortality rate than the one reported for the ADHERE validation cohort. After the assignment into the ADHERE risk groups, the observed mortality rates between groups differed significantly. Additionally, we found that the observed mortality was twice that of the one predicted by the ADHERE risk tree in the Low and Intermediate 2 risk groups and threefold in the Intermediate 1 risk group. Due to the small number of patients assigned to the High-risk group in our study population, it was not possible to draw consistent conclusions relative to this group.
The differences between the in-hospital mortality rates found in this study and those reported for the ADHERE cohort must be interpreted in light of the size and baseline characteristics of the two study populations. In fact, our study population (n=419) was much smaller than that of the ADHERE study (n=32,229). Looking at the baseline characteristics of the two study populations, patients had similar diabetes mellitus and peripheral vascular disease prevalence, SBP mean value, and BUN, sodium, and haemoglobin levels at the time of hospital admission. In contrast, the two populations differed in clinical characteristics such as coronary artery disease, atrial fibrillation, and LVEF. This study population presented a higher mean age, with more white and female patients, a more frequent history of hypertension and atrial fibrillation, less coronary artery disease, lower mean plasma creatinine levels at admission, and substantially higher LVEF. We did not analyse the direct individual impact of those factors on the in-hospital mortality rate. Still, of these factors, only age was found to be an independent predictor of mortality at one-year in the PRECIC study [7]. Other studies have also reported age as one of the strongest independent predictors of in-hospital mortality in AHF patients [4,5,8].
The in-hospital mortality rate reported in this study is similar to those reported in other studies from Portugal and other European countries [8-10], yet higher than those reported for USA large cohorts, such as ADHERE and OPTIMIZE-HF registry [3,5]. Interestingly, the mean ages of the ADHERE and OPTIMIZE-HF cohorts were 72.5 and 73 years, respectively, and the mean age of patients who died while hospitalised in the OPTIMIZE-HF, was 78.5 years, which is similar to the rate found in this study (79.5 years) [3].
In a large French HF registry–the OFICA study–the multivariate analysis identified age, low blood pressure and renal failure as the strongest independent predictors of in-hospital mortality for AHF patients. The mean age and mortality rate of the OFICA study were similar to those reported in this study [8]. In the OPTIMIZEHF registry, Abraham, et al. developed a predictive clinical model for in-hospital mortality among a large cohort of hospitalised HF patients in the USA, and also found that increasing age, low SBP, low sodium levels, increased heart rate, and increased creatinine at the time of admission were independent predictors of higher inhospital mortality. However, the OPTIMIZE-HF cohort has some significant differences compared to this study population, mainly in respect to the lower mean LVEF and the fact that some patients were not primarily hospitalised due to AHF [3].
In the 2017 report from the European Society of Cardiology Heart Failure Long-Term Registry, among the hospitalised subgroup of patients, the highest in-hospital mortality rates were observed in cardiogenic shock patients and in those with SBP lower than 85 mmHg, at the time of admission. The latter was associated with less geographic variation, supporting its more general applicability in clinical practice [11].
The role of BUN as an independent predictor of mortality in HF patients was reinforced in the report of the BIOSTAT-CHF risk model [12]. In the preliminary observations of the ADHERE study, renal kidney dysfunction was considered a hallmark of that study population [13], suggesting that it is one of the best discriminators of mortality risk [5].The mean serum urea level (or BUN) found in this study was not very different from that of the ADHERE validation cohort. Nevertheless, our patients had higher in-hospital mortality rates.
Likewise, we did not find a lower mortality risk in female or in patients with higher LVEF, as reported elsewhere [1,8,14]. Our study population characteristics, with a high percentage of females and high LVEF values (in contrast to the ADHERE population), is in accordance with previous studies that have shown that these two characteristics are linked [14-16], and are associated with hypertension, atrial fibrillation, and non-ischemic HF aetiology [1,17]. The MAGGIC risk score, based on a meta-analysis of 31 cohort studies, found that, in HF patients with LVEF>50%, age was more predictive of mortality than SBP, but the data is mostly from stable rather than acute hospitalised HF patients [14,18]. The high prevalence of patients with LVEF ≥ 40% in our study population has already been discussed in the PRECIC study report [6] and is primarily explained by the fact that patients originated from an Internal Medicine department. Nevertheless, we do not believe this factor justifies the higher in-hospital mortality observed, as the vast majority of published studies demonstrate similar or even lower mortality rates in patients with LVEF ≥ 40% [1,8,14,17].
Although we did not find any report of mortality variation related to race among hospitalised patients with AHF, the higher percentage of White patients in our sample could be one of the factors contributing to the higher in-hospital mortality observed, as previously suggested by Lim et al. in their analysis of risk-adjusted models for in-hospital mortality, which considered key laboratory and race/ethnicity data [19].
It is essential to highlight that, in this study, 50% of patients who died while hospitalised had some degree of dementia, and that 8.8% had an active cancer. In the PRECIC population, dementia and active cancer were independent predictors of mortality in the year following hospitalisation [7]. We could not find any data for the prevalence of dementia in the ADHERE population. Nevertheless, since in our study only about two thirds of in-hospital deaths were attributed to cardiovascular causes, we believe that dementia and active cancer might have had a major impact on the mortality rates and cause of death. Besides the common association between cancer and death, it is well-known that patients with dementia are prone to die in the hospital from complications, such as infections [20].
The ADHERE risk tree could not predict the in-hospital mortality rates for patients of this study. In this study, patients were more prone to die, even those in the Low-risk group. In line with this observation, in a recent analysis investigating the performance of four predicting tools for the mortality of AHF patients, including the ADHERE, Scrutinio et al. concluded that risk assessment tools work well for stratifying patients in risk groups, but have limited clinical utility in estimating the risk of mortality for individuals [21].
Nevertheless, we believe that our data reflect real-world treatment patterns and in-hospital clinical outcomes of patients hospitalised with AHF, at our hospital. So, what differences could explain the higher overall in-hospital mortality in the Low, Intermediate 2, and Intermediate 1 ADHERE risk groups? Firstly, age differences between the two study populations might be a major factor, because of the high impact of age on mortality in AHF cohorts, as previously described [13]. Secondly, the higher prevalence of atrial fibrillation found in our study could have had a negative impact on mortality. In fact, patients with chronic HF and atrial fibrillation have a poorer prognosis than those with sinus rhythm, which is largely explained by more advanced age and HF severity [1]. Thirdly, we compared patients hospitalised with AHF at different time periods and different countries with very different healthcare systems (Europe vs. USA). For instance, in this study, patients were recruited from the Internal Medicine Department, where most AHF patients are treated in Portugal, whereas, in the ADHERE study, most of the patients were recruited from the Cardiology Department [22,23]. It is also worth noting that our in-hospital and one-year all-cause mortality rates are in accordance with those reported in the European registries [8, 24-27], and in Portuguese studies [10,26].
Given the rise in prevalence of HF, there is an unmet clinical need for tools to accurately assess the prognosis of HF patients [28]. Undoubtedly, a quick and simple tool to predict in-hospital mortality would be very attractive for supporting clinical decisionmaking, through a better knowledge of the patients’ prognosis. However, it is unlikely that any one model can be universal, as the specificities of each healthcare scenario are likely to affect the outcomes. Additionally, it has been shown that the real-world performance of prediction models is generally poorer in new patient populations when compared to the original development study population. Therefore, every mortality risk predictor model must be tested for the local population and healthcare setting before the model can be implement in routine clinical practice [29].
In short, this study addresses a relevant issue: risk prediction models must be validated in the population/healthcare setting where they will be applied in clinical practice. We should be cautious and not extrapolate the findings validated for different countries and healthcare settings to other countries and settings, such as applying the USA ADHERE risk tree to AHF patients admitted to a large tertiary university hospital in Portugal. The findings of this study also pave the way for a better understanding of the realworld practice and clinical outcomes and, therefore, of the design of intervention strategies aimed at reducing short-term mortality of AHF patients.
After assigning the hospitalised AHF patients to the ADHERE risk groups, this study found that the in-hospital mortality rates among risk groups were significantly different. Overall, the observed mortality was higher than that predicted by the ADHERE risk tree. These findings contribute to a better awareness of AHF mortality and may pave the way to better patient management strategies and, as such, better clinical outcomes. Prediction models for the in-hospital mortality of AHF are important tools that need to be locally validated before they can be implemented in routine clinical practice.
This study has four major limitations. Firstly, it is a retrospective study, which makes it challenging to analyse the causes and influencing factors of the mortality rates observed. Secondly, there is the possibility that other clinical factors relevant to inhospital mortality were not considered in the analysis. Thirdly, patients hospitalised with AHF who died in the emergency room, and patients admitted to departments other than the Internal Medicine department, were not included in this study, which could contribute to an even higher mortality rate compared to the ADHERE study. Fourthly, our study population is much smaller than that of the ADHERE.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Novartis Pharma supported the statistical analysis and medical writing through an unrestricted grant but had no access to the data and did not have any other role in the study design, analysis, or decision to submit for publication.
None to declare.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Marques I, Bertão MV, Mendonça D, Teixeira L (2022) In-Hospital Mortality in Acute Heart Failure: Predicted ADHERE Risk vs. Observed Mortality. Int J Phys Med Rehabil. S21:003.
Received: 22-Jul-2022, Manuscript No. JPMR-22-18539; Editor assigned: 28-Jul-2022, Pre QC No. JPMR-22-18539 (PQ); Reviewed: 15-Aug-2022, QC No. JPMR-22-18539; Revised: 22-Aug-2022, Manuscript No. JPMR-22-18539 (R); Published: 31-Aug-2022 , DOI: 10.35248/2329-9096.22.10.645
Copyright: © 2022 Marques I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.