Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2021)
Objective: This study investigates the clinical outcome of Triamcinolone acetonide injected intracamerally in patients with hyphema and post-surgical iridocyclitis.
Method: Retrospective chart review of all patients from 2000 to 2005 diagnosed with hyphema and post-surgical iridocyclitis were included. All patients were injected with 1 mg in 0.1 mL of triamcinolone acetonide intracamerally and given topical steroid and a broad spectrum anti-bacterial eye drops initially given 4x a day the frequency reduced according to clinical response.
Results: Twenty cases were identified (14 males, 6 females; mean age 40). Eight patients (40%) were diagnosed with hyphema while twelve patients (60%) had post-surgical iridocyclitis. The pre-treatment visual acuity is hand movement with good light projection in 11 cases (55%) and at least 20/200 for the remaining nine cases (45%). Sixteen patients (80%) exhibited improvement of visual acuity by at least 1 line by the time the hyphema or inflammation resolved. Post-treatment visual acuity in fourteen cases was better than 20/40 and two cases at least 20/200. Four patients exhibited adverse events which include transient increase in intraocular pressure, development of fungal keratitis, and endophthalmitis.
Conclusion: We recommend that intracameral triamcinolone injection may be used as an adjunct to topical corticosteroid for cases of hyphema and post-surgical iridocyclitis. It can also be considered an alternate mode of drug delivery for very severe cases of anterior segment inflammation refractory to conventional modes of steroid delivery. It is also recommended that the risk-benefit ratio be weighed before undertaking this invasive procedure because of its potential complications.
Triamcinolone acetonide; Intracameral injection; Hyphema; Post-surgical iridocyclitis
Traumatic hyphema from a contusion to an eyeball can lead to several effects, especially when a large amount of blood is in the anterior chamber. In addition to visual impairment, it frequently obscures more serious complications such as lens dislocation, glaucoma, and separation of iris root, iritis, vitreous hemorrhage, and retinal detachment among others. A lot of these problems can only be evaluated once the hyphema has been cleared. Hyphemas are classified according to the volume of blood in the anterior chamber. Several authors recommend various medical management for traumatic hyphemas. They include complete bed rest with elevation of the head [1], sufficient sedation [1], eye patch [1], oral or topical steroids [2,3], mydriatics, oral tranexamic acid [4] among others. There are numerous controversies pertaining to the optimal approach to traumatic hyphema and no standardized guidelines for its management [5]. The ultimate goal is to promote excretion of the blood and blood particles and to prevent possible re-bleeding [6,7].
Triamcinolone acetonide is a minimally water-soluble steroid in suspension form that has been used empirically as a subconjunctival, subtenon, and retrobulbar depot for cases of uveitis [8]. Throughout the past few years, it has also been used as an intravitreal injection for the treatment of posterior uveitis [9] macular edema secondary to retinal vascular disease, and intraocular proliferation such as proliferative vitreoretinopathy [10] and choroidal neovascularization from age-related macular degeneration [11]. The past few years saw its emergent use especially in pediatric eyes which received intracameral triamcinolone intraoperatively that showed significant less anterior segment inflammation and no visual axis obscuration after cataract surgery with lens implantation [12] Some surgeons also use it in controlling postoperative inflammation following phacoemulsification [13] and phacotrabeculectomy [14] procedures in adults. An extensive literature search has revealed no previous studies on the use of triamcinoloneacetonide intracamerally for the treatment of hyphema and limited researches on post-surgical uveitis. The investigators planned to undertake this study to deter-mine the possible role of triamcinolone in the management of such diseases mentioned above.
Study subjects were seen consecutively from 2000 to 2005 at the Department of Ophthalmology and Visual Sciences External Disease and Cornea Clinic of the Philippine General Hospital (PGH) were selected based on the following inclusion criteria: male or female 18 years old or older which are clinically diagnosed to have non-perforating traumatic globe injuries with hyphema, acute or recurrent anterior uveitis, and iridocyclitis associated with intra-ocular surgery. Patients were excluded if they are diagnosed to have open-globe injuries, panuveitis, and uveitis of infectious etiology and if they refuse to participate in the study.
All patients were interviewed and underwent a complete eye examination consisting of visual acuity assessment, gross orbital exam, extraocular muscle function, intraocular pressure (IOP) determination, fundoscopy, and slit-lamp examination. The clinical diagnosis was recorded.
Triamcinolone acetonide (LBS Laboratory Ltd., Bangkok, Thailand), 1 mg in 0.1 ml was injected intracamerally. All patients were given additional topical steroid - Prednisolone acetate 1% (Predforte, Allergan, Westport Co., Mayo, Ireland) at 4x a day, Ciprofloxacin 0.3% (Ciloxan, Alcon-Couvreur, Puurs, Belgium) at 4x a day, and Atropine sulfate 1% (Isopto Atropine, Alcon Laboratories, Puurs, Belgium) at 3x a day. The topical medicines were adjusted according to the response of the patient.
All patients were admitted and followed up at 24 hours, 48 hours, 72 hours, 5 days, and 7 days, 2 weeks, 4 weeks, and 8 weeks after institution of treatment. Visual acuity, hyphema level, anterior chamber reaction, intra-ocular pressure, and complications were recorded on every follow-up. Oral mefenamic acid 500 mg/capsule may be given for ocular pain and headache as needed, and if indicated, topical timolol and oral acetazolamide were given for elevated intra-ocular pressure. Resolution of the hyphema or iridocycylitis is defined as the decrease in number of anterior chamber inflammatory or red blood cells from +4 to trace number of cells plus a decrease in the level of the hyphema and or hypopyon.
Twenty eyes from twenty patients (14 males and 6 females) with mean age of 40.05 were enrolled in the study (Table 1). Eight patients were diagnosed to have contusion eyeball with hyphema while twelve patients had post-surgical iridocyclitis, and all received 1mg per 0.1 ml of triamcinolone acetonide intracamerally. All patients were seen at an average of 6.75 weeks.
| Age years (mean +/- SD) | 40.05 +/- 21.93 |
|---|---|
| Sex (M:F) n = 20 | 14:06 |
| Diagnosis | |
| Contusion eyeball with hyphema | 40% (8/20) |
| Post-surgical iridocyclitis | 60% (12/20) |
| Follow up in weeks (mean +/- SD) | 6.75 +/- 1.83 |
| Rate of resolution in days (mean +/- SD) | 7.65 +/- 6.37 |
| Range | 2-30 days |
| Percentage of eyes improved in 7 days | 80% (16/20) |
| Percentage of eyes >14 days | 100% (20/20) |
| Visual acuity average lines of improvement | 4.45 using Snellen |
| Pre-injection visual acuity of hand movement | 55% (11/20) |
| Pre-injection visual acuity of 20/200 or better | 45% (9/20) |
| Post-injection visual acuity with improvement | 80% (16/20) |
| Visual acuity better than 20/40 | 87.5% (14/16) |
| Visual acuity 20/50-20/200 | 12.5% (2/16) |
| Post-injection visual acuity with no improvement | 20% (4/20) |
Table 1: Demographic data and baseline characteristics.
The rate of resolution of hyphema or anterior chamber inflammation ranged from 2 days to 30 days. The condition resolved by the first week of treatment in 16 out of 20 patients (80%). In the remaining patients (20%), two weeks or more of continuous treatment was required before resolution of hyphema and inflammation.
The pre-treatment visual acuity is hand movement with good light projection in 11 cases (55%) and at least 20/200 for the remaining nine cases (45%). Sixteen eyes (80%) exhibited improvement of visual acuity with an average of 4.45 Snellen lines by the time the hyphema or inflammation resolved while 4 (20%) eyes showed no line improvement. Post-treatment visual acuity in fourteen cases was better than 20/40 and two cases at least 20/200. Of the 4 eyes with no improvement in visual acuity, 2 were due to pre-treatment diagnosis of neovascular glaucoma, 1 eye proceeded to phthisis despite intervention, and the 4th patient developed fungal keratitis one week after treatment. The condition eventually proceeded to corneal melt which was treated aggressively with topical antibiotics and required corneal transplantation procedure.
Four patients exhibited adverse events during the course of the treatment. One patient had increased intraocular pressure on the second day after administration of triamcinolone. The rise in IOP may be attributed to inflammation rather than the steroid, because (1) the eye had exhibited intense AC reaction/ inflammation before steroid injection, and (2) the IOP eventually decreased by the 4th day with anti-glaucoma medications even without AC washout of the steroid. One patient had increased IOP 6 weeks after the administration of triamcinolone.
This increase may be attributed to the prolonged use (6 weeks) of topical prednisolone acetate 1% (PredForte). Infection occurred in two patients. In one patient with corneal perforating injury, corneal infiltrates were detected at the corneal laceration site 4 days after triamcinolone injection. Corneal scraping revealed hyphal elements.
The cornea melted and the patient subsequently underwent corneal transplant, sectoral iridectomy, and anterior vitrectomy. In the last patient, hypopyon and vitreous abscess were seen 5 weeks after injection of steroid. Cultures grew Candida spp. The patient eventually underwent pars plana vitrectomy. No other cases of corneal toxicity or decompensation were noted in the duration of the study (Table 2).
| Percentage of eyes with complications | 20% (4/20) |
|---|---|
| Glaucoma | 10% (2/20) |
| Infectious nature | 10% (2/20) |
Table 2: Complications
The use of corticosteroid to treat intraocular inflammation and hyphema has been established a long time ago. However, when severe anterior chamber inflammation becomes unresponsive to topical medication, a sub-conjunctival depot of triamcinolone is usually given to achieve a continuous therapeutic level. The level of the drug that penetrates the scleral barrier, however, is also affected by several factors, and may be insufficient is some cases.
Therefore, for cases that require immediate and high dose of steroid delivered into a specific area, an alternative method is to give it intracamerally.
The results of the study are dramatic in majority of the cases. The initial visual acuity is hand movement with good light projection in eleven cases and at least 20/200 for the remaining nine cases. Sixteen out of twenty patients exhibited improvement of visual acuity by at least 1 line by the time the hyphema or inflammation resolved. Post-treatment visual acuity in fourteen cases was better than 20/40 and two cases at least 20/200. The average line improvement by Snellen chart is 4.45 lines after only one week.
Triamcinolone acetonide has been studied well in the past few years and was found out that when injected intravitreally, the mean elimination half-life was 18.6 days in non-vitrectomized eyes and 3.2 days for patients who had undergone vitrectomy [15]. This is an important parameter for our study for several reasons. First, this supports our result that the hyphema (Figures 1A and 1B) and post-surgical iridocyclitis (Figures 2A and 2B) have resolved by the first week of treatment in 16 out of 20 cases (80%). Consequently, as a result, it improved the visual acuity by at least one line in the Snellen chart for all 16 cases. Fourteen cases had visual acuity of 20/40 or better while two cases had 20/200. Second issue relates to the development of glaucoma in two patients. The first patient had a transient rise in intraocular pressure (IOP) two days after injection of triamcinolone which we attribute it to an inflammatory type of glaucoma. The second patient, on the other hand, developed glaucoma on the sixth week of treatment, which we attribute it to continuous use of topical corticosteroid use and not to the intracameral triamcinolone. Both cases of glaucoma were treated with oral acetazolamide and a topical beta blocker which resulted to a return in normal IOP after one week. No other IOP spikes were recorded after the treatment.
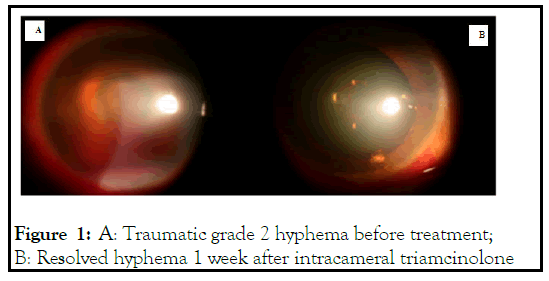
Figure 1: A: Traumatic grade 2 hyphema before treatment; B: Resolved hyphema 1 week after intracameral triamcinolone
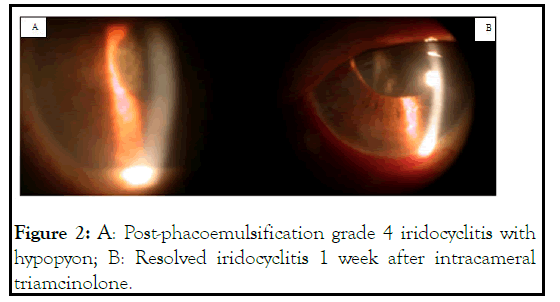
Figure 2: A: Post-phacoemulsification grade 4 iridocyclitis with hypopyon; B: Resolved iridocyclitis 1 week after intracameral triamcinolone.
Aside from rises in intraocular pressure, unwanted corticosteroid effects to the eyes include development of cataract and suppression of host defense mechanism. As a result, several organisms such as those of the normal flora and fungi may proliferate. Our results show two cases of fungal growth. The first case was a post-corneal laceration repair from a metal wire injury. The patient developed corneal infiltrates 1 week after administering triamcinolone intracamerally. This patient eventually underwent penetrating keratoplasty for the corneal ulceration. The second patient, on the other hand, developed hypopyon on the sixth week of treatment. The patient underwent pars plana vitrectomy for Candida spp. endophthalmitis. Literature shows that intravitreal injection of medications has a very low rate of developing endophthalmitis especially when it is used with topical antibiotics [16]. Similar to this case is a report by Ataka et al. has showed case of endophthalmitis due to Fusarium spp. after triamcinolone assisted pars plana vitrectomy [17].
Any drug administered into the anterior chamber may also produce toxic effects to the corneal endothelium. In our series, we demonstrated no cases of corneal toxicity or decompensation in majority of the cases for the duration of the study. This supports a previous study done by Oh et al. [18] that intracameral triamcinolone injection does not adversely affect the function of corneal endothelium in rabbits.
We recommend that intracameral triamcinolone injection may be used as an adjunct to topical corticosteroid for cases of hyphema and post-surgical iridocyclitis. It can also be considered an alternate mode of drug delivery for very severe cases of anterior segment inflammation refractory to conventional modes of steroid delivery. It is also recommended that the riskbenefit ratio be weighed before undertaking this invasive procedure because of its potential complications.
Citation: Agahan ALD, Tecson III JV, Valenton MJ (2021) Intracameral Triamcinolone for the Treatment of Hyphema and Post-Surgical Iridocyclitis. J Clin Exp Ophthalmol. 12:897.
Received: 29-Oct-2021 Accepted: 12-Nov-2021 Published: 19-Nov-2021
Copyright: © 2021 Agahan ALD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.