Journal of Medical & Surgical Pathology
Open Access
ISSN: 2472-4971
ISSN: 2472-4971
Case Report - (2023)Volume 8, Issue 1
Introduction: Intramuscular myxoma is a benign soft tissue tumour of the musculoskeletal system that is relatively uncommon. The majority of patients are in their fourth to eighth decades of life, with a slight female predominance. The large muscles of the thigh, shoulder, buttocks, and arms are the most commonly affected by swelling. Only histopathology can provide a definitive diagnosis of the tumour. Local recurrence following excision is unusual.
Case report: A 63-year-old female patient presented to us with a swelling measuring approximately 17 × 10 × 3 centimetres in the left thigh. She was thoroughly examined, and the swelling was excised in toto. Histopathology revealed that the solid-cystic swelling excised was an intramuscular myxoma.
Conclusion: The tumor's rarity and its significance in the differential diagnosis of nerve sheath myxomas, sarcomas, intramuscular lipoma, hemangioma, hematoma, and desmoid tumour is the emphasis for this case report presentation. Another distinguishing feature is that, it can only be accurately diagnosed after excision followed by histopathological examination.
Intramuscular myxoma; Soft tissue swelling; Benign
Myxomas are uncommon benign tumours. They can be found in heart, bones, skin, subcutaneous and aponeurotic tissues, the urogenital tract, and skeletal muscle. They are thought to be derived from primitive mesenchymal cells that lose their ability to produce collagen but produce an excess of hyaluronic acid and immature collagen fibres instead [1]. These tumours typically affect the muscles of the thigh, arm, buttock, and shoulder [2-5]. The tumour has a slight female predilection and a peak incidence between the fourth and eighth decades of life [6]. An IM usually manifests as a single lesion [7], but in up to 5% of cases, it can manifest as multiple tumours [6]. Patients typically report a slowgrowing, palpable, painless mass [5,7]. Intramuscular myxomas involve larger muscle groups, can be seen in the elderly, and can reach relatively large sizes, as seen in many soft tissue sarcomas, making differentiation difficult. Despite its apparent encapsulation and well-defined borders, the lesion microscopically infiltrates the muscle [8].
A 63 year old female patient presented to us with a swelling of the left thigh. The swelling was painless and had gradually increased in size since its appearance 6 months prior to presentation to us. The swelling measured about 17 × 10 × 3 centimetres in anterior, superior 1/3rd and was soft in consistency and was mobile in the vertical plane. Its size reduced on active muscle contraction. Ultrasound examination revealed heteroechogenic lesion with cystic component. The patient was investigated with MRI, which revealed a 15 × 7 × 6 cm hetero intense, multi-lobular lesion, left thigh between vastus medial is and intermedius without any distant lesions.. FNAC revealed features suggestive of a benign spindle cell lesion. A trucut biopsy showed myxoid areas with occassinal spindle cells. Hence a wide excision was planned for further confirmation and evaluation the soft tissue lesion. CT chest–normal study. Routine blood and urine examination had not revealed any abnormality. An excision of the tumor in to under spinal anesthesia was done, taking care to avoid damaging the vessels lying in close proximity to it. It was a well encapsulated cystic mass. Patient had no post- operative complications and was discharged after a couple of days. The irregular greyish white wide excision specimen was sent to histopathology for examination. Grossly the specimen received for HPE was a single irregular greywhite soft tissue mass measuring 11.5 × 10 × 4.5 cm with overlying elliptical skin bit (anterior margin) measuring 5.0 × 1.0 cm, lateral margin had a long silk thread and superior margin had a short silk thread (Figure 1). Cut surface showed a well encapsulated solid- cystic lesion measuring 8.5 × 5.0 × 4.0 cm. The globular solid area was placed in superior part was measuring 5.5 × 5.5 × 4.0 cm and it was tan white glistening. The inferior multiple cystic area were filled with gelatinous material (Figure 2). Bits were given from the lesion (solid, cytic areas), skin, superior and lateral margins. Microscopy showed an encapsulated tumor free from overlying skin, interspersed between striated muscles. The tumor is predominantly hypocellular comprising bland cells and occasional spindle cells with basophilic mucoid matrix and few capillaries in the background. No evidence of hyper-cellularity, atypia, mitosis and lipoblasts. Periphery shows collagenous capsule and striated muscle fibers (Figures 3 and 4). To confirm the diagnosis Vimentin and CD-34 was done and to rule out Dermal nerve sheath myxoma S100 and Desmin was done and the result was negative.
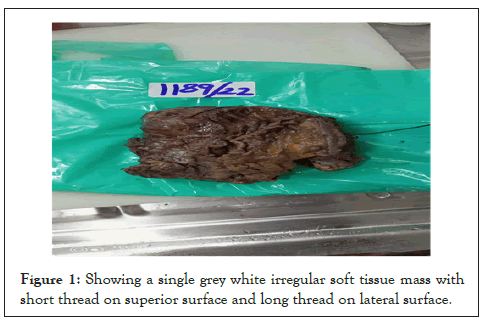
Figure 1: Showing a single grey white irregular soft tissue mass with short thread on superior surface and long thread on lateral surface.
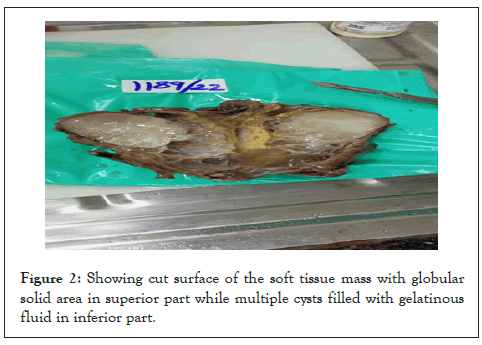
Figure 2: Showing cut surface of the soft tissue mass with globular solid area in superior part while multiple cysts filled with gelatinous fluid in inferior part.
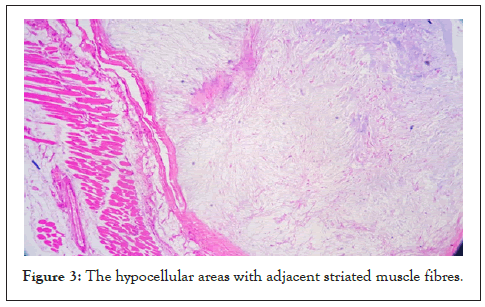
Figure 3: The hypocellular areas with adjacent striated muscle fibres.
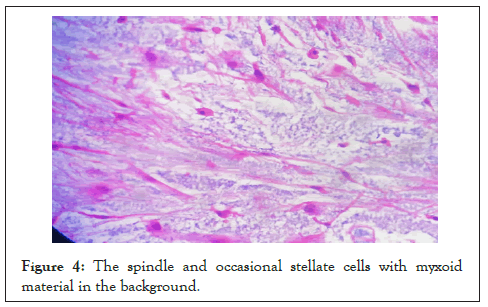
Figure 4: The spindle and occasional stellate cells with myxoid material in the background.
Virchow in 1871 used the term myxoma to describe a tumor that histologically resembled the mucinous substance of umbilical cord [9]. The IM is a rare tumour with an incidence of approximately one per million [10]. It can occur in any skeletal musculature, but it prefers the large, proximal groups of the extremities. While approximately half of all incidences occur in the thigh musculature, it has previously been estimated that less 10% occur in upper arm [11]. The aetiology of the IM is still unknown [7], although there is evidence that it may be associated with mutations in the Guanine Nucleotide Binding Protein, Alpha Stimulating (GNAS ) gene [6,12]. It is common in the 5th and 6th decade of life. There is a slight female predominance [13]. The tumour may present as a solitary mass [7] or very rarely as multiple lesions [6]. Single or usually multiple IMs may occur in conjunction with fibrous dysplasia, known as Mazabraud’s syndrome [14], and it has therefore been recommended to routinely examine patients who are diagnosed with an IM for the presence of fibrous dysplasia [2]. Clinically, an IM most frequently manifests itself as a slow-growing, palpable, painless mass [5-7] as was the case with the patient presented in this report.
X-ray examinations may be normal or show a non-specific intramuscular mass that rarely contains calcifications [5,15]. On ultrasound images, an IM typically appears as a well-circumscribed, hypoechogenic or heteroechogenic mass, sometimes with a cystic component [2,14]. CT examinations usually show a well-defined, homogenous, low-density lesion [2,4]. On MRI images, an IM typically presents as a hypointense signal mass on T1-weighted images and with a hyperintense signal on T2-weighted images [2,4]. In the case reported here, the ultrasound examination thus revealed typical findings of an IM in the form of a well-defined, heteroechogenic lesion with a cystic component. Although imaging techniques are necessary in the diagnostic workup, histopathological examination is the only way to reach a definitive IM diagnosis. Prior to treatment, a core needle biopsy may be useful for differential diagnosis. Macroscopically, IMs typically appear as oval, greywhite, gelatinous masses with a firm consistency [2,4]. Microscopically, the lesions are usually hypocellular and hypovascular [2,6,16] and contain spindle- and stellateshaped cells with small, hyperchromatic nuclei that are embedded within an abundant myxoid stroma [2,7]. Generally, mitotic activity and pleomorphism are absent [2,6]. In our case, the histopathological results were consistent with these typical findings of IMs .The treatment of choice for IM is radical surgical excision. Complete excision of the lesion with clear small margins of surrounding tissue is essential whenever feasible [5]. Incomplete resections may result in local recurrences [4]. Conversely, recurrence of the tumour is extremely rare after radical excision [4,6]. IMs do not show potential for malignant transformation and do not have a tendency to metastasize [5].
Thus, intramuscular myxoma is a relatively uncommon benign musculoskeletal lesion. Excision surgery is both necessary and curative. An elderly patient with a solitary soft tissue tumour should be thoroughly investigated to rule out soft tissue sarcomatous conditions, which mimic intramuscular myxoma in many ways. These facts are well-explained in the preceding case report.
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
[Crossref][Google Scholar][PubMed].
Citation: Dhanalakshmi MNK, Rajendran K, Balamurugan S (2022) Intra-Muscular Myxoma: A Rare Begnin Soft Tumor; Case Report. J Med Surg Pathol. 7:251.
Received: 06-Oct-2022, Manuscript No. JMSP-22-19478; Editor assigned: 10-Oct-2022, Pre QC No. JMSP-22-19478 (PQ); Reviewed: 25-Oct-2022, QC No. JMSP-22-19478; Revised: 24-Mar-2023, Manuscript No. JMSP-22-19478 (R); Published: 31-Mar-2023 , DOI: 10.35248/2472-4971.23.8:265
Copyright: © 2022 Dhanalakshmi MNK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.