Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2020)Volume 5, Issue 2
Granular Cell Tumor (GCT) is a tumor with neuroectodermal differentiation, and it has been classified into the peripheral nerve sheath tumor group of 2013 by World Health Organization (WHO) soft tissue tumor classification. It can arise in any part of the body. Paediatric GCTs have been less reported, and deep soft tissue is a rare location. An eight-year six-month boy had an asymptomatic subcutaneous-like solid mass in the axilla. The mass was characterized as a walnut shape, and the focal skin color was normal with normal skin temperature. The left upper limb function was preserved. The postoperative pathology diagnosed as a benign intramuscular GCT at deep latissimus dorsi muscle in the axilla.
Results: It needs to be differentiated from lymphadenectasis, lymphadenectasis, and fibroma. MRI is helpful in making the diagnosis combined with other multiple approaches, such as a physical exam, ultrasound, and enhancecontrast CT. Soft-tissue GCT has the infiltrating pathological feature and tends to be more aggressive than other types of GCTs despite the benign behavior at the first diagnosis.
Granular cell tumor; Neuroectodermal tumor; Paediatric
Granular cell tumor (GCT) manifests at all ages but with a peak incidence in the fourth through sixth decades [1]. Most of the GCTs are benign, and lesions are often found in the subcutaneous and submucosal tissues, most commonly in the skin, tongue, upper extremities, and breast [2,3]. GCT is usually small in size (≤ 3 cm) with a static growing pattern. Patients usually asymptomatic, increasing the clinical diagnosis challenges [4]. Paediatric GCT presenting at the intramuscular muscle of axilla is a rare case reported worldwide. Therefore, this report is to describe the complete clinical manifestation of this rare case, aiming to provide the clinical evidence.
An eight-year-old boy has been found with an asymptomatic left axially mass incidentally during the bath by his parents for one week. The mass was characterized as a walnut shape, and the focal skin color was normal with normal skin temperature. The left upper limb function was preserved.
Physical Examination
A subcutaneous walnut-shaped mass was identified under the left axilla, about 3.0 cm × 3.0 cm × 3.0 cm. The firm mass was characterized by poor mobility and a clear boundary. The patient reported no associated pain. No focal skin changes were observed.
Imaging Findings
No apparent abnormalities were found in the chest radiograph. Color Doppler ultrasound revealed the echo of a mix-echoic visible mass on the left axilla with a size of about 24.4 mm × 23.0 mm × 20.1 mm, having a clear boundary and regular margin. The lesion presented a heterogeneous internal echo with hyperechoic predomination. Also, Color Doppler Flow Imaging (CDFI) showed the spot-like blood flow signals within the mass (Figure-1 and 2). Contrast-enhanced chest Computed Tomography (CT) scan demonstrated a circular soft-tissue lesion at the left underarm, which measured 19 mm × 24 mm in size with a clear margin. The lesion had an iso-density to surrounding muscles with CT value measured as 52 HU (Figure-3 and 4). After contrast injection, CT value increased to 62 HU, showing a similar enhancing pattern to the adjacent muscular tissue.
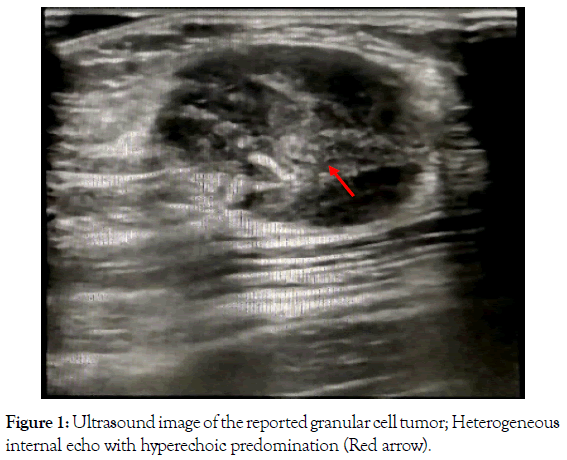
Figure 1. Ultrasound image of the reported granular cell tumor; Heterogeneous internal echo with hyperechoic predomination (Red arrow).
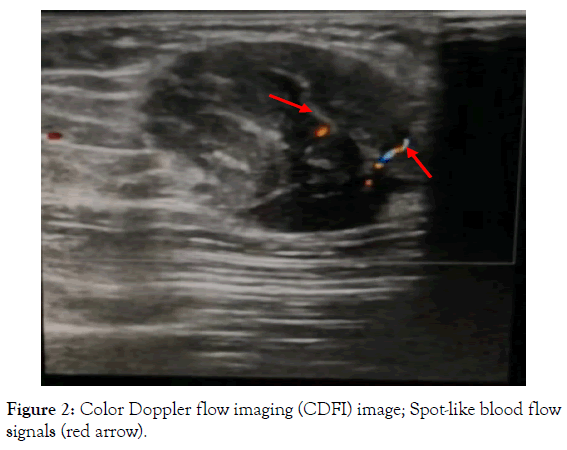
Figure 2. Color Doppler flow imaging (CDFI) image; Spot-like blood flow signals (red arrow).
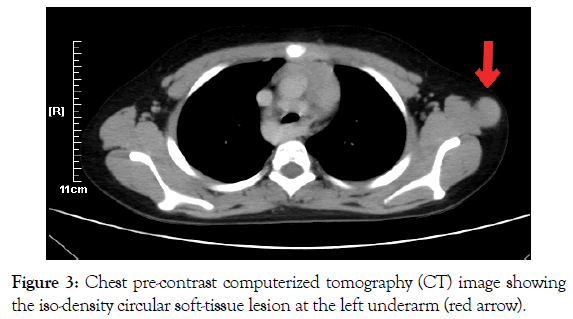
Figure 3. Chest pre-contrast computerized tomography (CT) image showing the iso-density circular soft-tissue lesion at the left underarm (red arrow).
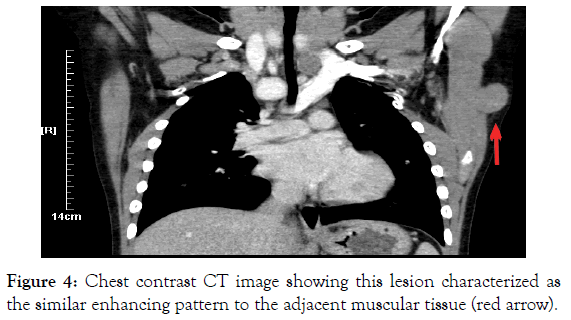
Figure 4. Chest contrast CT image showing this lesion characterized as the similar enhancing pattern to the adjacent muscular tissue (red arrow).
Surgical Operation
At surgery, an incision was performed parallel to the lesion, up to 4 cm. The solid mass, grayish-white, and of a hard texture, in the deep latissimus dorsi muscle under the axilla, was excised. There was no clear boundary of the mass itself with the adjacent muscular soft tissue.
Pathological Examination
Postoperative pathology reported that abundant eosinophilic tumor cells were distributed in a piece or nest with adipose tissue infiltration. Tumor cells were granulated in granular shape (Figure-5 and 6) with oval nucleus Immunohistochemistry: AE1/ AE3 (-), ALK (D5F3 Ventana IHC (-), CD68 (-), ki-67 (+, about 10%), S-100 (+) (Figure-7 and 8). The report confirmed a benign granular cell tumor invading the surrounding tissue.
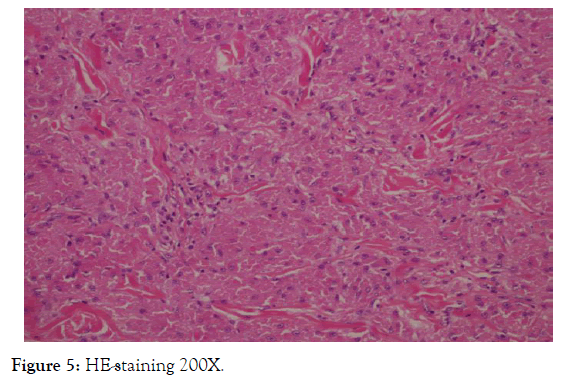
Figure 5. HE-staining 200X.
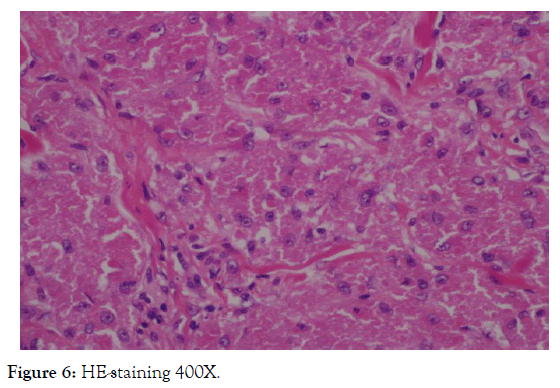
Figure 6. HE-staining 400X.
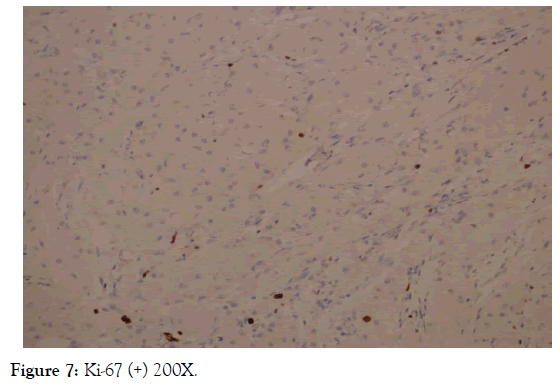
Figure 7. Ki-67 (+) 200X.
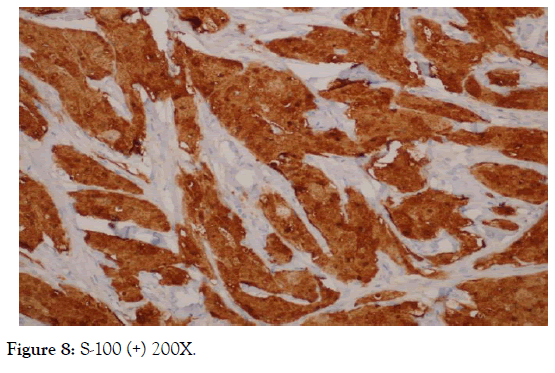
Figure 8. S-100 (+) 200X.
Clinical Follow-up
The patient has been followed up for two months. The color Doppler ultrasound showed no recurrence.
This study reported a rare case of paedratic intramuscular GCT, situated in the deep latissimus dorsi muscle under the axilla, in an 8-year-6-month boy. Most of the GCTs occur in the subcutaneous soft tissue up to 80%, but less than 20% located within the muscular tissue [1,5,6]. Moreover, compared with adults, intramuscular GCT in children is very rare [6], and this study may be the first case report about paedratic intramuscular GCT. Therefore, this study aims to provide clinical evidence of paedratic intramuscular GCT regarding diagnosis and prognosis to advance the clinical management of soft-tissue tumors in children.
GCTs of soft tissue tend to have more infiltrative, and more often have positive margins showing the distinct behaviors from subcutaneous and submucosal lesions [6]. The intraoperative and histological performances of this mass are consistent with the character of soft tissue GCTs, such as the unclear margin with the adjacent tissue and adipose tissue infiltration. Soft-tissue GCTs usually have the atypical and malignant behaviors due to the nature of the mass itself, especially for intramuscular GCTs [1,5,7]. However, these previously reported cases were in adults.
For this paedratic case, it was defined as the benign tumor despite having an invading growing pattern according to the GCT malignancy definition proposed by Fanburg-Smith [8]. He claimed that malignant GCT should have at least three of the following histopathological features: Necrosis, spindling of tumor cells, vesicular nuclei with large nucleoli, increased mitotic rate (greater than two mitoses/10 high-power fields), high nuclear to cytoplasmic ratio, and pleomorphism. However, the historical-begin GCT of soft tissue has been reported with the focal recurrence since the first diagnosis5 and metastasis [9,10]. The intramuscular GCT in the present study had no recurrence after the surgery rection, which may indicate the behavior variants of GCTs of soft tissue between adults and children. However, long-term and close clinical follow-up is also crucial as it may recur after several years [5]. The reports of soft-tissue GCTs in children are scarce, and observational studies with larger sample sizes are warranted.
Preoperative diagnosis of intramuscular GCTs in children is also tricky as the discordance of imaging findings and intraoperative results were observed in this case. Although the gold-standard diagnosis of GCTs relies on pathological reports, optimal preoperative imaging approaches can better characterize tumor tissue and help clinicians make an effective clinical management plan to decrease unnecessary invasive risks before the intervention. For the imaging features of GCTs, malignant tumors have more identifiable characteristics than benign ones. Singh et al. have found that many malignant GCTs commonly present central hypodense areas consistent with necrosis or cystic changes in CT [11]. However, benign lesions are lack of typical diagnostic imaging features indicating GCT. Chest X-ray, ultrasound, cardiac CT of this boy did not show characteristic signs; moreover, the clear boundary identified by different imaging modalities was not consistent with the invaded pattern observed during the surgery.
For soft-tissue GCTs, preoperative Magnetic Resonance Imaging (MRI) is recommended as its excellent differential capability of soft tissue from subcutaneous lesions [12], especially of intramuscular GCTs. T2-weighted sequences can identify a slight difference between heterogeneous tissue components and ill-defined margins, such as fat, muscle, and fibrosis/collagen, intervening in the tumor cells [13]. Peripheral high intensity is another highly specific features of GCTs from intramuscular origin [12,13]. However, this case did not go through an MRI scan before surgery, and the results missed by CT scan and ultrasound may be caught up by MRI. Therefore, MRI is suggested to be the essential radiological modality for patients with suspicious soft-tissue tumors. Furthermore, MRI is a nonradiative tool with high spatial resolution, which is much safer than other modalities for children.
We report this case to describe the clinical manifestation of paediatric intramuscular GCT, which has not been reported by the previous literature. As its unique location mimicking the subcutaneous lesions and asymptomatic performance, it increases the diagnostic challenges. It needs to be differentiated from lymphadenectasis, lymphadenectasis, and fibroma. MRI is helpful in making the diagnosis combined with other multiple approaches, such as a physical exam, ultrasound, and enhancecontrast CT. Soft-tissue GCT has the infiltrating pathological feature and tends to be more aggressive than other types of GCTs despite the benign behavior at the first diagnosis. Thus, the close follow-up for a long time is recommended for a benign intramuscular GCT. Pediatric intramuscular GCT is poorly understood, and further cohort studies are needed.
All authors listed on the manuscript have approved the submission of this study. They took full responsibility for the whole study period. Xiong Yongqiang wrote the draft of the manuscript. Zhou Xiang and Wei Qiang followed up the patient clinically. Zhang Xiaodong collected relevant imaging data and pathological data. Jia Xinjian revised the manuscript.
The author(s) received no financial support for the research, authorship, and publication of this article.
The authors declared that we had obtained the written consent from the parents of the patient for publication of the related clinical data.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest concerning the research, authorship, and publication of this article.
Citation: Xiong Yongqiang, Zhou Xiang, Wei Qiang, Zhang Xiaodong and Jia Xinjian (2020) Intramuscular Paediatric Granular Cell Tumor Presenting as an Axillary Mass: A Case Report. Clin Pedia OA 5:163 doi: 10.35248/2572-0775.20.5.163.
Received: 13-Dec-2019 Accepted: 02-Apr-2020 Published: 09-Apr-2020 , DOI: 10.35248/2572-0775.20.5.163
Copyright: © Yongqiang X, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Competing interests: The authors have declared that no competing interests exist.