Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 1
Aim: This study aimed to explore the potential involvement of endogenous testosterone levels in the etiopathogenesis of Central Serous Chorioretinopathy (CSCR).
Materials and methods: Conducted as a case-control study with 82 participants selected from a tertiary care center in North India, the subjects were categorized into 41 cases and 41 controls. Fasting blood samples were collected in the early morning to assess serum testosterone levels, measured using the chemiluminescent immunoassay method.
Results: The mean age for CSCR patients and controls was 35.71 ± 5.82 years (range 22-49 years) and 33.71 ± 8.42 years (range 20-50 years), respectively. The median serum testosterone level in cases was 4.79 ng/ml, with an odds ratio of 3.16. However, the 95% Confidence Interval (CI) of the odds ratio, ranging from 0.31 to 31.7, indicated no significant association between endogenous testosterone levels and central serous chorioretinopathy.
Conclusion: This study concludes that there is no statistically significant correlation between Central Serous Chorioretinopathy (CSCR) and elevated endogenous serum testosterone levels.
Chorioretinopathy; Testosterone; Eye; Retinal pigment epithelium
Central Serous Chorioretinopathy (CSCR) is a condition within the pachychoroid spectrum, characterized by fluid leakage through the Retinal Pigment Epithelium (RPE) into the sub-retinal space as shown in Figure 1. Typically observed in young males, CSCR is associated with various risk factors, including elevated glucocorticoid levels due to psychosocial stress, type A personality, steroid therapy, cushing syndrome and pregnancy as shown in Figure 2. Laboratory evidence indicates that human RPE and mammalian choroidal cells possess androgen receptors. Testosterone, influencing syndecan expression, may play a role in epithelial cell adhesion to the extracellular matrix [1]. Central Serous Chorioretinopathy (CSCR) is a complex eye disease with unclear pathogenesis, believed to involve alterations in choroid circulation and Retinal Pigment Epithelium (RPE) function. Evidence from fluorangiography and Optical Coherence Tomography (OCT) indicates increased capillary permeability and choroid vessel pressure (Figures 1 and 2).
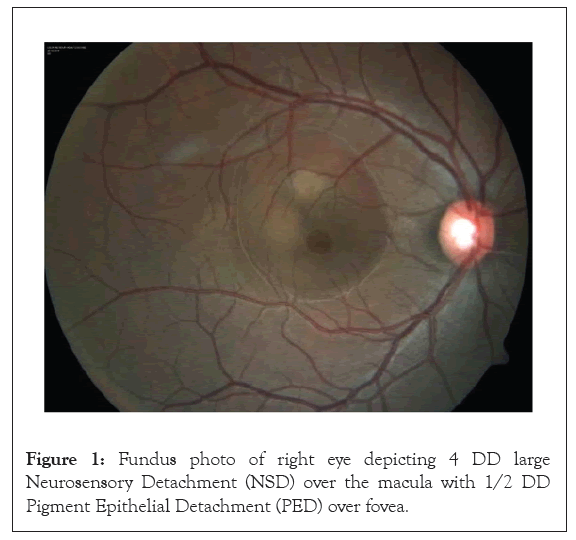
Figure 1: Fundus photo of right eye depicting 4 DD large Neurosensory Detachment (NSD) over the macula with 1/2 DD Pigment Epithelial Detachment (PED) over fovea.
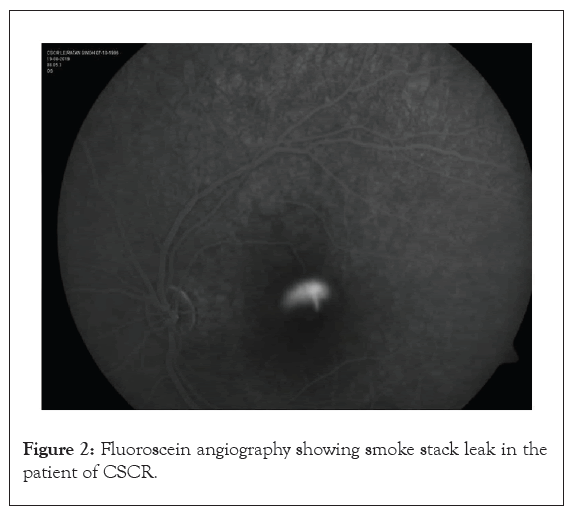
Figure 2: Fluoroscein angiography showing smoke stack leak in the patient of CSCR.
The higher prevalence of CSCR in men suggests a direct association with androgens. A study by Nudleman, et al., [2] found exogenous testosterone therapy to be a probable independent risk factor for CSCR, with symptoms resolving upon discontinuation. Kumar, et al., [3] case-control study proposed that increased cortisol concentration might affect testosterone binding, influencing CSCR development.
Studies by Zakir, et al., [4], Natung, et al., [5] and others explored cortisol and testosterone levels in CSCR patients, revealing normal hormone levels in most cases. Haimovici, et al., [6] identified mineralocorticoid dysfunction as a feature of CSCR. Ahad, et al., [7] reported the first case linked to systemic testosterone therapy, showcasing a temporal association between elevated testosterone and CSCR development.
Grieshaber, et al., [8] case report highlighted a woman developing CSCR due to exogenous testosterone for fatigue. The hypothesis suggested androgen receptors in the retinal pigment epithelium and associated testosterone levels contribute to CSCR, especially in males and those with high-stress personalities.
Tufan, et al., [9] investigation into cortisol and testosterone levels in chronic CSCR revealed weak associations. Lin, et al., [10] reported a rare case of bilateral CSCR induced by long-term testosterone treatment, emphasizing the importance of reviewing medical conditions and medications.
In summary, research points to a multifaceted relationship between sex hormones, particularly testosterone and CSCR development, offering insights into potential risk factors and alternative treatments. Intrigued by the relationship between testosterone and CSCR, we undertook a study to examine if endogenous testosterone levels have any impact on causation of CSCR.
A case-control study was conducted at a tertiary care hospital in North India from September 2018 to September 2019, adhering to the Declaration of Helsinki, institutional ethical committee approval was obtained. The study included 41 cases with Central Serous Chorioretinopathy (CSCR) and 41 controls without the condition. Criteria for inclusion were age between 20-50 years, diagnosed CSCR cases and inclusion of both genders. Exclusion criteria involved individuals on exogenous steroids/testosterone, ocular/systemic diseases causing steroid disturbance, recent surgery and pregnant females. Comprehensive eye examinations and diagnostic tests were performed on a single day, including automated refraction, Best Corrected Visual Acuity (BCVA), slit lamp biomicroscopy, indirect ophthalmoscopy, fundus fluorescein angiography, OCT and fundus autofluorescence.
For serum testosterone analysis morning testosterone levels were obtained at 8:00 am, utilizing the DiaSorin LIASON testosterone kit via chemiluminescent immunoassay. Normal ranges were established for males (1.20-10.19 ng/ml, 18-49 yrs; 1.95-8.95 ng/ ml, >50 yrs) and females (0.05-0.73 ng/ml, 18-49 yrs; 0.08-0.51 ng/ml, >50 yrs).
Statistical Package for Social Sciences (SPSS) version 20 was used for statistical analysis in our case-control study with 82 subjects (41 cases, 41 controls). The average age was 35.71 years as shown in Figure 3. Median serum testosterone levels in cases were 4.79 ng/ml as shown in Figure 4. The odds ratio was 3.16, with 7.3% of CSCR patients and 2.4% of controls showing elevated testosterone. However, the 95% CI (0.31 to 31.7) suggested no significant association between endogenous testosterone levels and central serous chorioretinopathy (Figures 3 and 4 and Tables 1 and 2).
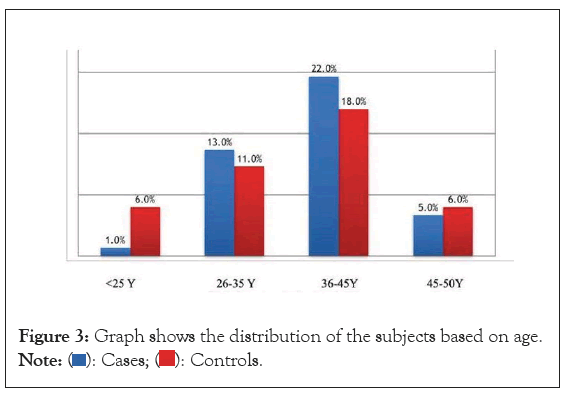
Figure 3: Graph shows the distribution of the subjects based on age. 
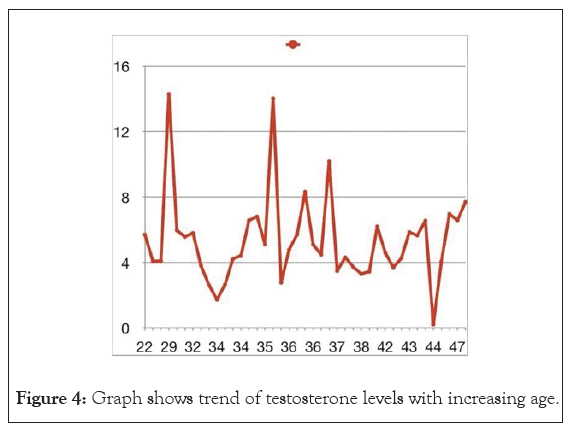
Figure 4: Graph shows trend of testosterone levels with increasing age.
| Testosterone levels | Case | Control | |
|---|---|---|---|
| Abnormal | 3(a) | 1(b) | |
| Normal | 38(c) | 40(d) | |
| Total | 41 | 41 | |
| Odds ratio=3.16 | 0.985 | 0.985 | |
| Category | Value | 95% confidence interval | |
| lower | Upper | ||
| Odds ratio for testosterone levels (abnormal/normal) | 3.16 | 0.31 | 31.7 |
Table 1: Table showing odds ratio.
| Categories | Natung 2012-14 | Tufan, et al. 2013 | Zakir 2009 | Haimovici 2003 | Our study |
|---|---|---|---|---|---|
| Type of study | Descriptive study | Observational study | Case control study | Observational study | Case control study |
| No. of cases | 30 acute/chronic | 6 | 23 | 24 | 41 |
| No. of controls | - | - | 12 | - | 41 |
| Mean age of patients | 42.43 | Median-48 | 37.1 | 43.0 | 35.71 |
| Method testosterone estimation | Chemi | Chemi | RIA | RIA | Chemi |
| Results | |||||
| Mean testosterone value | 5.88 | 549.5 normal levels | 3.85 ± 1.81 | 1 out of 24 had high testosterone value | 5.44 |
| P value | >0.05 | 0.58 | OR-3.16 with 95% CI (0.31-31.7) | ||
| Conclusion | Not significant | Not significant | Not significant | ||
Note: RIA: Radioimmunoassay; OR: Odds Ratio; CI: Confidence Interval
Table 2: Comparative table of various studies and our study.
The etiopathogenesis of Central Serous Chorioretinopathy (CSCR) remains an enigma for ophthalmologists, presenting a multifaceted challenge with numerous factors contributing to its initiation. The higher prevalence in men suggests a potential link between testosterone levels and the etiopathogenesis of CSCR. Upon scrutinizing the existing literature, we discerned pertinent details from studies by Nudleman, et al., [2], Grieshaber, et al., [8], Ahad, et al., [7], Lin, et al., [10] and Chen, et al., [11], which established a connection between exogenous testosterone and CSCR.
Despite documented instances of CSCR emerging post-exogenous intake of steroids or testosterone therapy, cases without recognizable comorbidities or recent surgeries underscore the implicit association between testosterone and CSCR. However, the lack of definitive studies delineating the precise role of testosterone in CSCR remains conspicuous.
The question raised is “Are endogenous levels of testosterone in the human body also responsible for retinopathy?” To address this query, we conducted a case-control study to determine any potential relationship between serum testosterone levels and CSCR. Comprehensive history, clinical examination and laboratory investigations were carried out, revealing that none of the subjects had an existing systemic illness. During the study, five subjects on exogenous steroid intake were excluded, adhering to the exclusion criteria. All individuals were then subjected to early morning overnight fasting serum sample collection for the assessment of serum testosterone, following a methodology akin to the study by Tufan, et al., [9].
Haimovici, et al., [6] estimated serum testosterone levels in CSCR patients, finding normal levels in 96% of their patients. Similarly, Zakir, et al., [4] were the first to compare serum testosterone levels in CSCR patients with age and sex-matched controls, observing mean serum levels within the reference interval in both cases and controls. They noted that about 32% of CSCR patients and 18% of controls had levels lower than the reference interval.
Concluding studies by Zakir, et al., [4], Natung, et al., [5], Haimovici, et al., [6], Tufan, et al., [9] and others revealed that serum testosterone levels were within the normal physiological range in CSCR patients, failing to establish a definitive association. Similarly, our study found that of the total 41 CSCR patients, serum testosterone was elevated in 7.3% and in 2.4% of the control group. No statistically significant association between endogenous testosterone levels and CSCR was found, as determined by an odds ratio of 3.16 with a 95% confidence interval of 0.31 to 31.7.
This implies that serum testosterone levels and CSCR are not correlated; the presence of high endogenous testosterone levels does not raise the odds of CSCR and conversely, the presence of CSCR does not raise the odds of raised serum testosterone value. No correlation between high testosterone and CSCR was observed. The age group in our study ranged from 20 to 50 years, with an average age of 35.71 years.
In contrast, a study by Kumar, et al., [3] on 23 CSCR patients discovered that two patients with high 8:00 AM cortisol levels also had testosterone levels higher than the reference interval. The majority of patients in their study showed testosterone within the reference interval and no statistical significance was found when correlating serum cortisol levels with serum testosterone levels. Two of the three females showing high testosterone levels were in the menopausal age group, suggesting a protective role of reproductive hormones in pre-menopausal females.
Consistent with the studies by Ahad, et al., [7], our study also demonstrated a preponderance of CSCR in men. However, Zakir, et al., [4] found that about 32% of CSCR patients and 18% of controls had serum testosterone levels lower than the reference interval, a trend not observed in our CSCR patients.
Notably, 68.2% of our patients had only unilateral eye involvement. Out of 41 cases, 24 were acute cases and all three cases with abnormal values were acute cases, hinting towards a potential link between deranged testosterone levels and acute cases more than in chronic cases. Out of 82 eyes, 40(48.7%) had 6/6 vision and exhibited symptoms of micropsia, metamorphopsia, scotoma or decreased contrast sensitivity.
Our study discovered higher endogenous testosterone levels in cases, albeit statistically insignificant and this trend was observed primarily in acute cases. This may suggest a potential role of testosterone in acute onset cases more than in old, chronic cases and particularly in the male population, where it is a pivotal hormone. The majority of our patients had serum testosterone levels within the normal range, but three out of 41 had deranged values, not statistically significant in our study. Tufan, et al., [9] also analyzed serum testosterone of six CSCR patients on a chemiluminescent immunoassay system, finding normal levels in their study. The complexity of the relationship between testosterone and CSCR necessitates further comprehensive research to unravel the intricacies of this intriguing association.
Our study, with a substantial sample size of 41 cases, stands as the first of its kind in contrast to previous investigations on this topic. Our findings indicate no statistically significant association between Central Serous Chorioretinopathy (CSCR) and elevated serum testosterone levels. This suggests that raised endogenous testosterone might not be a contributing factor. To solidify this conclusion, larger prospective studies are essential. Further investigations are required to establish a range of endogenous testosterone levels that could predict the likelihood of CSCR in the future.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Gupta R, Kurumkatti R, Trehan HS, Mohapatra T, Singh PK, Yadav Y (2024) Investigating the Impact of Endogenous Testosterone Levels on Central Serous Chorioretinopathy. J Clin Exp Ophthalmol. 15:970.
Received: 29-Dec-2023, Manuscript No. JCEO-23-28175; Editor assigned: 01-Jan-2024, Pre QC No. JCEO-23-28175 (PQ); Reviewed: 15-Jan-2024, QC No. JCEO-23-28175; Revised: 22-Jan-2024, Manuscript No. JCEO-23-28175 (R); Published: 30-Jan-2024 , DOI: 10.35248/2155-9570.24.15.970
Copyright: © 2024 Gupta R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.