Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Case Report - (2021)
Iron deficiency anemia is a common gastroenterological presentation. Endoscopic investigation is standard practice. We describe a case of iron deficiency anemia in a patient who was lost to follow‐up, before representing with clinically significant overt gastrointestinal bleeding, leading to a diagnosis of metastatic small bowel neuroendocrine tumor. Early diagnosis can lead to curative surgical management. Iron deficiency anemia in a young man is a red flag and warrants thorough investigation.
Gastrointestinal Neuroendocrine Tumours (GINET); Iron deficiency; Anaemia
Gastrointestinal Neuroendocrine Tumours (GINET) is the most common primary tumour of the small intestine. While seemingly innocuous, the indolent spread and the paucity of symptoms in non-secretory tumours equates to approximately 45%-71% of cases being metastatic at the time of diagnosis [1,2]. Furthermore, primary lesions tend to be small, and despite characteristic desmoplasia, GINET tends to elude radiographic detection or yield non-specific findings that require endoscopic or laparoscopic correlation [3]. The estimated prevalence of GINET is 9.2/1,00,000. The incidence peaks at 60 years of age 4 and it accounts for approximately 1.5% of gastrointestinal neoplasms and 0.3% of all cancers in the United States [4,5]. The incidence however has increased by approximately 350% in the last 30 years [6]; whether this can be attributed to a more ubiquitous use endoscopic surveillance or advances in diagnostic imaging, allowing these lesions to be detected incidentally, remains to be proven. High grade (poorly differentiated) lesions are associated with a predilection for metastases and invasion [7].The endocrine origin of these tumours makes them amenable to targeted therapy and therefore, even when metastatic, GINET tend to have relatively positive survival outcomes. The estimated 10-year survival rate for metastatic low grade GINET is 42% [7].
A 50 years old male patient was referred to gastroenterology outpatients for investigation of iron deficiency anaemia. Medical history was significant for a past hepatitis B infection, reflux on pantoprazole 40 mg daily and osteoarthritis treated with ibuprofen as required. He is an ex-smoker, with a 20-pack year history and has a history of excess alcohol use of 20 standard drinks per week. He had no dietary restrictions. An upper gastrointestinal endoscopy and colonoscopy were performed, both of which were unremarkable. A subsequent capsule endoscopy was organised, however he failed to attend the procedure and was lost to follow up. The patient re-presented approximately 1 year later with maroon coloured faeces, haemodynamic instability and presyncope. On examination, abdomen was soft and non-tender with the digital rectal exam revealing maroon coloured stools. An urgent upper gastrointestinal endoscopy showed non-bleeding erosive gastroduodenitis. CT Angiography was unremarkable save for minor fat stranding in the omentum.
A colonoscopy was performed with fresh blood noted in the terminal ileum. The ileum was intubated to 30 cm from the ileocaecal valve and a 10 mm submucosal lesion was found without ulceration or stigmata of recent bleeding. Decision was made to proceed to retrograde double balloon enteroscopy. An ulcerated submucosal lesion was found 150 cm from the ileocecal valve; (Figure 1a). Another three submucosal lesions were seen in the jejunum and ileum. Magnetic resonance enterography failed to identify any of the submucosal lesions. A laparoscopy was performed with the intent of small bowel resection. However extensive peritoneal carcinomatosis was found at time of surgery and a decision was made to abort the procedure. Peritoneal and omental biopsies were taken (Figure 1b and 1c).
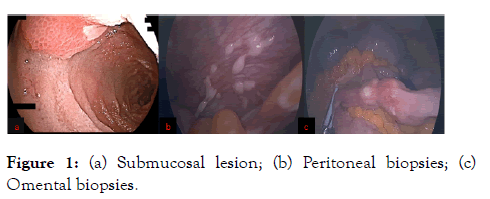
Figure 1: (a) Submucosal lesion; (b) Peritoneal biopsies; (c) Omental biopsies.
Histological findings of metastatic low-grade neuroendocrine tumour were noted, with positive immunohistochemistry for synaptophysin, chromogranin, AE1, AE3 and BerEp4. The Ki67 was<3%. Gallium dotatate was positive for uptake in the distal small bowel and peritoneum; (Figures 2 and 3). The patient was referred to the oncology team and was commenced on monthly ranleotide.
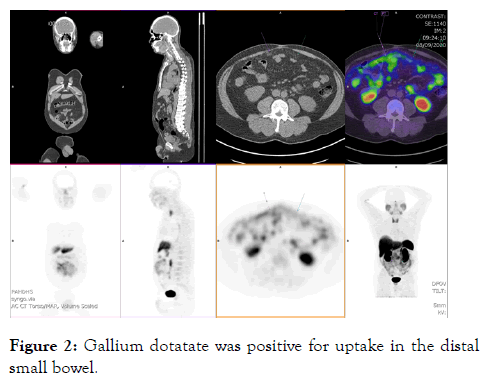
Figure 2: Gallium dotatate was positive for uptake in the distal small bowel.
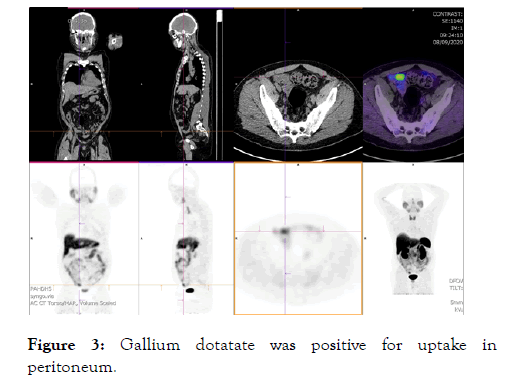
Figure 3: Gallium dotatate was positive for uptake in peritoneum.
Our patient initially presented with a seemingly languid clinical prodrome of iron deficiency anaemia and rectal bleeding. In this case, occult blood loss in the form of iron deficiency anaemia was an early sign of brewing small bowel pathology, namely a non-secretory GINET. It follows that diagnosis of GINET can be delayed due to the absence of localising symptoms and a multimodal approach is required for definitive diagnosis, including endoscopy, imaging and surgery as we have outlined. Broadly GINET are classed based on the location of the primary lesion as foregut, midgut or hindgut [7]. Midgut GINET usually arises from the ileum and the appendix [8]. Up to 40% of cases present with non-specific abdominal pain or intermittent obstruction in 25% of cases [2]. Tumours may be functional, presenting with carcinoid syndrome (diarrhoea, abdominal pain, and flushing) or non-functioning, presenting with bleeding or mass effects [4], as was observed in this case. Iron deficiency may be one of the earliest signs of gastrointestinal blood loss from GINET.
Treatment modalities are guided by the extent of disease and the degree of differentiation. Surgical resection is the mainstay for management of localized lesions [9], however if resection is not viable (in the case of metastatic disease), somatostatin analogues are usually commenced and the dose titrated to control tumour growth and paraneoplastic symptoms. If initial treatment fails, anti-VEGF or mechanistic target of rapamycin (mTOR) inhibitor therapy may be used; if somatostatin receptor positive, peptide receptor radioligand therapy can be considered as an adjunct [10]. As the endocrine origin of the tumour, it followed that targeted therapies could improve survival even with metastatic GINET.
This case demonstrates the indolent nature of small bowel neuroendocrine tumors, where iron deficiency may be the only manifestation. Early diagnosis can lead to curative surgical management. Iron deficiency anemia in a young man is a red flag and warrants thorough investigation. Subsequent sections of the report discuss four major issues that the committee considered:
• defining iron deficiency anemia and the effects of different criteria on its estimated prevalence,
• determining the prevalence of iron deficiency anemia and considering its public health importance,
• developing methods for delivering iron to children and women, and
• determining the efficacy and safety of different interventions.
Citation: Gounden S, Kaazan P, Yuide PJ, McIvor C (2021) Iron Deficiency Anaemia or a Bigger Problem? Intern Med. S4:001.
Received: 22-Jan-2021 Accepted: 05-Feb-2021 Published: 12-Feb-2021 , DOI: 10.35248/2165-8048.21.s4.001
Copyright: © 2021 Gounden S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.