Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2019)Volume 9, Issue 3
Introduction: Tumoral calcinosis is a rarely described metabolic condition, characterized by the accumulation of calcium hydroxyapatite crystals in the soft tissues. The purpose of this paper is to present a case of a tumoral calcinosis with uncommon characteristics in order to discuss the diagnosis and treatment options.
Case report: We report the case of a 65 years-old patient with a multifactorial avascular necrosis of the femoral head, to which a hip replacement was planned. Due to the images observed preoperatively, infection was ruled out and after the studies; an isolated tumoral calcinosis was identified and confirmed with histopathological findings.
Conclusion: Tumoral calcinosis is a benign pathology that can create confusion due to the nonspecific characteristics. Metabolic profile studies and multimodal imaging are recommended to diagnose this condition adequately. In some cases, biopsy or aspiration can also be helpful to confirm the diagnosis.
Calcinosis; Joint Diseases; Magnetic Resonance Imaging; Hip Joint/diagnostic imaging; Primary tumoral calcinosis; Soft tissue mass
Tumor calcinosis is a rare pathology characterized by the accumulation of calcium hydroxyapatite crystals in the soft tissues. It is frequently caused by errors in phosphorus metabolism associated with conditions such as hyperphosphatemia, or in sporadic cases has been related with mutations in the gene GALNT3, FGF23 or KL, with expression usually autosomal recessive.
The majority of cases have been recorded in patients younger than 20 years old, and it is rare to observe this condition in patients older than 50 years old [1]. In general, the most affected joints are the hips, shoulders and occasionally the spine. In small joints and the skin, painful masses can be identified [2].
The diagnostic images show calcifications in the soft tissues which are usually nonspecific. In ultrasound, levels compatible with fluid sedimentation can be found [3]. The axial tomography can show images of cystic calcifications. Other functional studies such as bone scans or PET are usually inconclusive [4].
Due to the non-specificity of the radiological and clinical findings, tumor calcinosis can be confused with calcified traumatic lesions, devitalized tissue, or even with infectious or tumoral lesions [5]. Therefore, a high suspicion is necessary when abnormal peri-articular calcifications are observed [6]. The objective of this article is to present a case of tumoral calcinosis and discuss the diagnostic approach and treatment based on the current literature.
A 65-year-old female patient with a medical history of moderately differentiated infiltrating ductal breast cancer IIIB diagnosed 21 years ago, attended to the clinic with 15-months history of severe right inguinal pain, that limited the walking and weight bearing.
She was treated with neoadjuvant chemotherapy, followed by a modified radical mastectomy, adjuvant chemotherapy for three cycles, radiotherapy, and hormone therapy with tamoxifen until 2006. In 2017, limping and pain in the right hip were documented, in association with progressive limitation of the range of movement.
Imaging studies were taken, and a collapse of the femoral head compatible with avascular necrosis with important arthritic changes was identified in x rays (Figure 1).
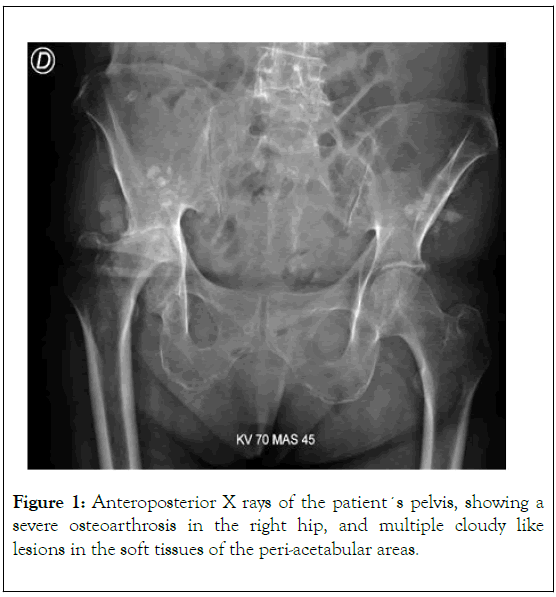
Figure 1. Anteroposterior X rays of the patient´s pelvis, showing a severe osteoarthrosis in the right hip, and multiple cloudy like lesions in the soft tissues of the peri-acetabular areas.
Bone scan only showed degenerative changes ruling out metastasis or other bone alterations (Figure 2).
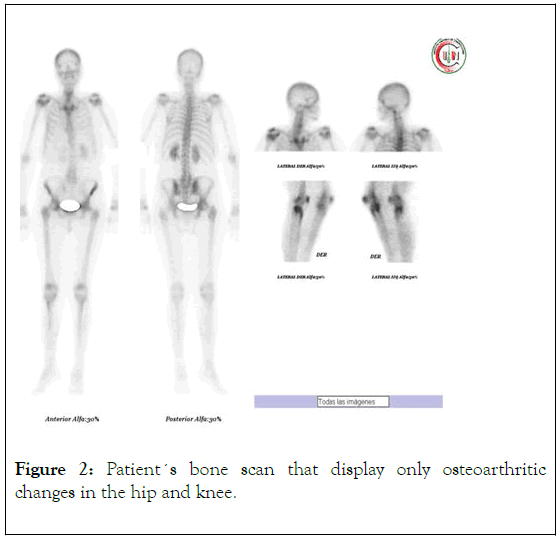
Figure 2. Patient´s bone scan that display only osteoarthritic changes in the hip and knee.
MRI images demonstrated a round lesion close to the right acetabulum with a low intensity in T1, and heterogeneous characteristics in T2, with a liquid level; these images were initially interpreted as possible post-traumatic calcifications on fluid collections in the peri-articular tissues (Figure 3).
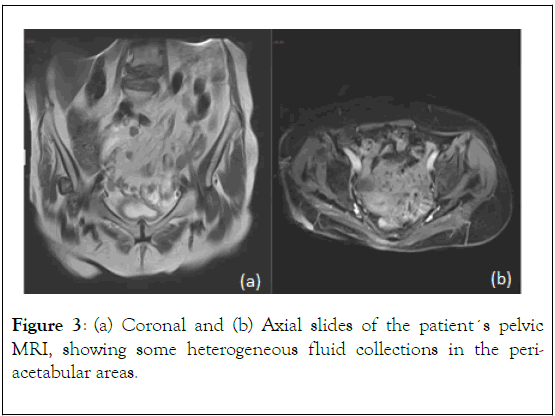
Figure 3. (a) Coronal and (b) Axial slides of the patient´s pelvic MRI, showing some heterogeneous fluid collections in the periacetabular areas.
A multifactorial right femoral head avascular necrosis was considered as the first diagnostic impression. After discussing the case, the decision was to perform a conventional hip replacement to treat the sequelae, however, due to the images observed in the soft tissues, local infection had to be ruled out.
The initial studies were inconclusive to confirm infection or metabolic issues (Table 1). Therefore, a two-stage hip replacement was selected in order to obtain samples and control pain in an effective manner.
| Variables | Values | Variables | Values | Variables | Values |
|---|---|---|---|---|---|
| Creatinine | 0.3 mg/dL | Potassium | 3.3 mEq/L | Phosphorus | 4.1 mg/dL |
| BUN | 13 mg/dL | Sodium | 137 mEq/L | Uric acid | 4.4 mg/dL |
| Calcium | 7.8 mg/dL | Magnesium | 1.3 mEq/L | CRP | 31 mg/dL |
Table 1: Biochemical profile of the patient at the moment of the first surgery.
During first stage of the surgery, a very important amount of a whitish fluid was obtained from the peri-articular area. Tissue samples were taken for study (Figure 4), and a resection arthroplasty was performed, until a definitive diagnosis was obtained (Figure 5a).
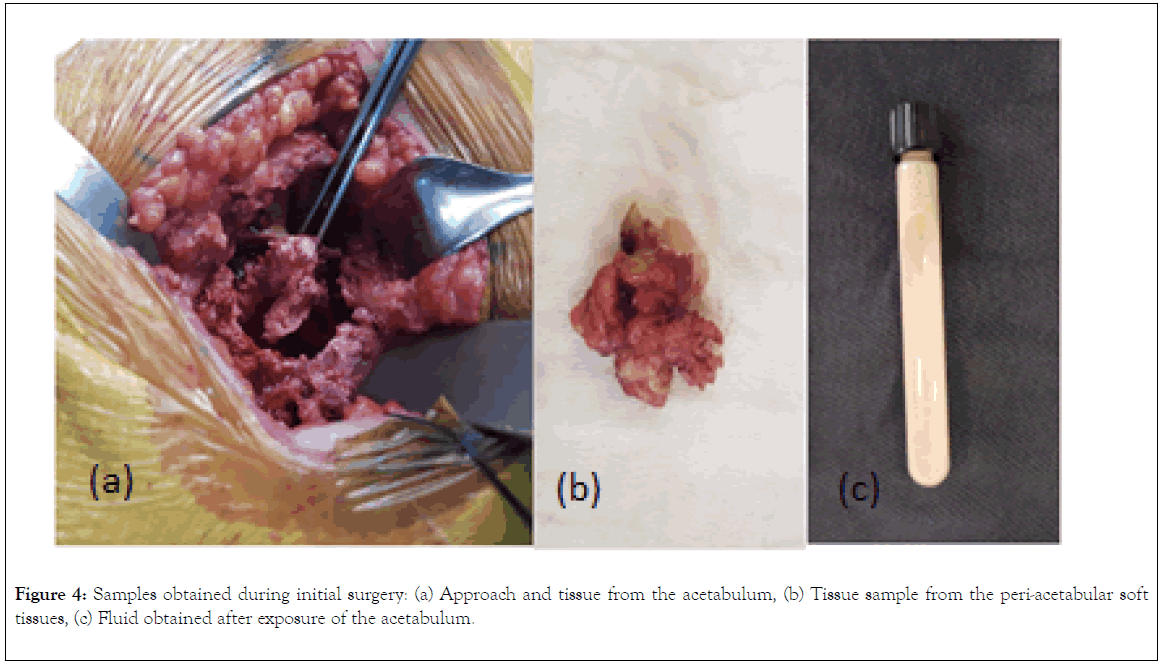
Figure 4. Samples obtained during initial surgery: (a) Approach and tissue from the acetabulum, (b) Tissue sample from the peri-acetabular soft tissues, (c) Fluid obtained after exposure of the acetabulum.
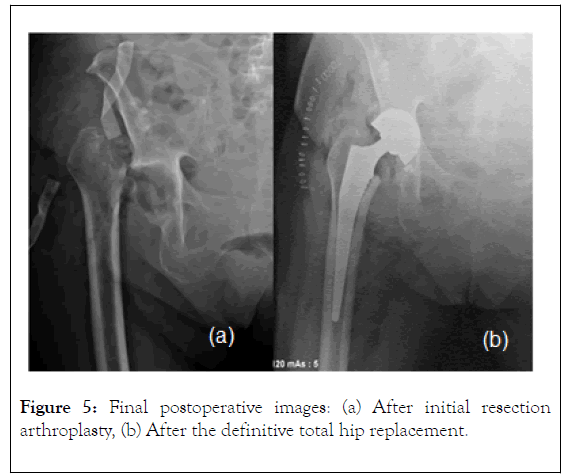
Figure 5. Final postoperative images: (a) After initial resection arthroplasty, (b) After the definitive total hip replacement.
The final reports of the Gram analysis and cultures were negatives and did not identify common germs, anaerobic or fungal organisms in the samples discarding infection; no elevation or change in the acute phase proteins was documented, and phosphate levels were also normal.
Histopathological analysis revealed a clean background with proteinaceous material and occasional histiocytes, associated with increased calcium deposits negative to malignant behavior (Figure 6). Due to the normal phosphate level, the diagnosis was considered consistent with normo-phosphatemic primary tumoral calcinosis.
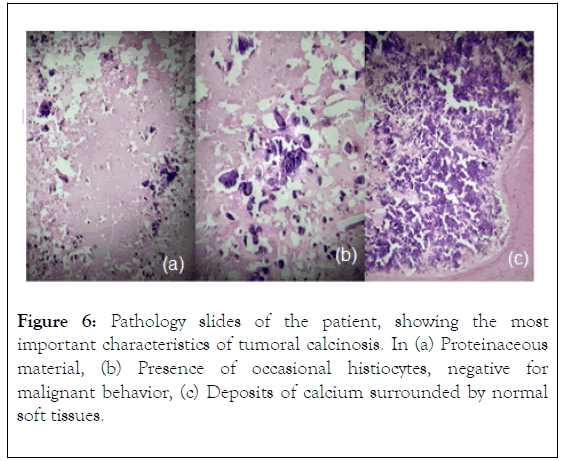
Figure 6. Pathology slides of the patient, showing the most important characteristics of tumoral calcinosis. In (a) Proteinaceous material, (b) Presence of occasional histiocytes, negative for malignant behavior, (c) Deposits of calcium surrounded by normal soft tissues.
With a clear diagnosis, the initial resection arthroplasty was converted to an uncemmented hip replacement (Figure 5b). After the surgical treatment, the patient presented an adequate evolution. She has been followed for two years by now, and at the current time, no infectious or metabolic complications have been recorded.
Tumoral calcinosis is a benign pathology that behaves like a great imitator and in most cases it is associated with hereditary diseases of metabolic phosphate dysfunction [7]. It often leads to the appearance of soft tissue lesions which are described as well demarcated lobular calcifications [8]. Lesions are usually distributed around large joints and can sometimes be associated with mass and pain [9].
The imaging findings of calcifications in soft tissues can be confusing; therefore, the radiologist plays an important role in the diagnosis [10]. When in doubt, the multimodal approach, with culture taking, laboratory monitoring and biopsy may be necessary to establish the correct etiology.
In cases as the one reported, factors such as bone involvement, or age over 50 years old are atypical in the presentation, and therefore, can create some distraction from the diagnosis of tumoral calcinosis, making the identification of the problem and the early treatment more difficult.
The treatment of massive peri-articular calcinosis should be individualized and will depend to a large extent on its underlying cause. The excision of the lesions is a good choice if these masses are limiting the function, involving the joints or generating pain or restriction for daily life activities [7].
Phosphate restriction proved to be of variable success and this is believed to be due to the late presentation in most of the cases. However, surgical excision combined with phosphate deprivation (using aluminum hydroxide in conjunction with synergistic acetazolamide) lowers hyperphosphatemia and has proven to be the most effective therapy [8]. Systemic steroids and radiotherapy have been shown to be also efficient [9].
In dystrophic calcifications, the application of intralesional corticosteroids does not reduce their size or appearance [10]. The use of oral anticoagulants has shown a variable decrease in the more subcutaneous lesions [11]. While shock wave therapy has shown improvement in pain in the randomized trials for calcific tendonitis [12].
Symptomatic treatment for very painful skin lesions with fine needle aspiration and percutaneous fragmentation reported pain relief by 30% [12]. Therapy for metabolic calcification should seek control of the underlying hormonal or metabolic cause [13]. Intravenous sodium thiosulfate (STS) may be an effective option for treating calcifications in patients undergoing hemodialysis. Local STS injections seem efficient in subcutaneous calcified lesions with a 50% reduction in size within 2 years of treatment, but the evidence found is still very weak [14].
The recurrence of these lesions can occur, and therefore it is necessary to clearly establish the etiology of the lesions, to offer a correct treatment. Although metabolic control should be the objective, the option of local treatments, combined therapies or surgical removal are options for painful lesions [13].
Tumoral calcinosis is a rare condition that requires from the treating physician a high suspicion index. In order to diagnose this entity, multimodal radiological imaging and the analysis of the biochemical profile should be performed. After excluding connective tissue diseases, the treatment has to be adjusted to the patient-specific needs and conditions. In cases of confusion, biopsy may contribute to determine the histopathological characteristics and confirm the diagnosis. Due to the nonspecific characteristics of this condition, the radiologists, clinicians and pathologists should be aware in order to avoid incorrect diagnosis.
We declare no conflict of interest for the authors
Citation: Medellin MR, Salinas-Alvarez V, Gomez-Mier LC, Soto-Montoya C (2019) Isolated Tumoral Calcinosis in the Hip Mimicking Periarticular Infection: A Case Report and Literature Review. Rheumatology (Sunnyvale). 9:256. DOI: 10.35248/2161-1149.19.9.256
Received: 05-Dec-2019 Accepted: 20-Dec-2019 Published: 26-Dec-2019 , DOI: 10.35248/2161-1149.19.9.256
Copyright: © 2019 Medellin MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.