
Journal of Clinical and Cellular Immunology
Open Access
ISSN: 2155-9899

ISSN: 2155-9899
Short Commentary - (2017) Volume 8, Issue 4
Keywords: Immunoglobulin; Multiple sclerosis (MS); kFLC Index
Intrathecal oligoclonal immunoglobulin synthesis is commonly observed In inflammatory disorders of the central nervous system (CNS) of either infectious or autoimmune origin [1,2].
Multiple sclerosis (MS), where intrathecal synthesis is present, is one of the most common neurological diseases of the young adults in CNS, and it often causes deficits since its early stage. Clinically isolated syndrome (CIS) is a central nervous system demyelinating event isolated in time and it is compatible with the possible future development of multiple sclerosis (MS). Early risk stratification for conversion to MS helps with treatment decisions [3]. Currently it is possible to identify the presence of antibodies by the detection of oligoclonal immunoglobulin bands (OCBs) in cerebrospinal fluid (CSF) [4,5]. It is necessary to differentiate the origin of immunoglobulin (Ig) in the CSF before intrathecal immunoglobulin synthesis can be diagnosed [6]. Immunoglobulin light chains that are circulating in serum in a free state are called Free Light Chains (FLCs). These can be both kappa (kFLCs) and lambda type (λFLCs). We examined 80 CSF/serum pairs from patients of the neurological clinic who underwent analysis of OCBs during their diagnostic workup. We analysed the correlation between OCBs test and the FLCs nephelometric assay [1] and we assessed the diagnostic accuracy of a nephelometric assay for k free light chain determination in cerebrospinal fluid and serum. The correlation between the two methods was very good, but the method to determine OCBs is time-consuming, not quantitative, and also relatively insensitive and operator depending. [1,2,7-9]. On the contrary, the nephelometric determination of FLCs in serum and CSF is a quantitative method and it might be a sensitive alternative to the above-mentioned approach.
In some cases we found positivity to intrathecal immunoglobulin synthesis with the nephelometric method, that was absent with immunofissation [1,9]. These results highlight the greater sensitivity and specificity of nephelometric assay method in the detection of intrathecal immunoglobulin synthesis [1,9-11]. The development and evaluation of new technologies to define local vs. systemic B-cell responses in patients with Multiple Sclerosis or Clinically Isolated Syndrome versus patients with other inflammatory neurological diseases should shed new light on the role of CSF OB [12]. The 80 patients studied were divided into three groups depending on the neurological diagnosis: non-inflammatory disorders (Group 1), inflammatory disorders excluding MS (Group 2) and patients with definitive MS (Group 3). The same patients were analyzed for the presence of immunoglobulins, FLCs and albumin on both serum and CSF to highlight possible differences between three groups.
During the study of the kFLCs (kappa Free Light Chains) concentration, we find that kFLC Index calculated as 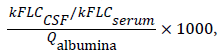 provides a specific tool to follow intrathecal immunoglobulin synthesis and it seemed to be more accurate especially in patients with impaired CSF-serum barrier [1]. Furthermore kFLC Index, with the best sensitivity and specificity in MS patients, could replace the OCBs test and help the neurologists to monitor the patient’s treatment.
provides a specific tool to follow intrathecal immunoglobulin synthesis and it seemed to be more accurate especially in patients with impaired CSF-serum barrier [1]. Furthermore kFLC Index, with the best sensitivity and specificity in MS patients, could replace the OCBs test and help the neurologists to monitor the patient’s treatment.
Subsequently [9], we have increased the number of patients in order to confirm our previous results. We analysed 176 patients and the results obtained confirmed the importance of the kFLC Index as an aid for the diagnosis of MS [9].
In the first study two patients had a CIS diagnosis (Group 2) but a kFLC Index higher than the cutoff (Figure 1A). Over time, these patients were again hospitalized and diagnosed with MS (Figure 1B, Group 3), highlighting kFLC Index's importance. One of these patients was followed in our hospital and he was the subject of a case report [13].
Figure 1: Scatter plot of three patient’s groups depending on neurological diagnosis, Group 1: non-inflammatory disorders; Group 2: inflammatory disorders excluding Multiple Sclerosis; Group 3: patients with definitive MS. (A) Scatter plot of all patients in the study of Duranti et al. 2013. (B) Scatter plot of all patients in the study Pieri et al. 2017. The arrow describe that two patients change their diagnosis during this time from clinically isolated syndrome to Multiple sclerosis, so they shift from Group 2 to Group 3. Our data indicates that the FLCs assay could replace the OCBs test and confirms the great specificity and sensitivity of the kFLC Index as a valid aid in the MS diagnosis. kFLC Index determination provides a tool for following changes in the synthesis of intrathecal immunoglobulins. Moreover its use in clinical routine, can assist the McDonald criteria facilitating a faster MS diagnosis and hence a more early therapeutic treatment. The kFLC Index is an early MS marker, and in some cases it may have a prognostic and predictive role in the diagnosis of MS.
Three patients within the 176 had a kFLC Index below the cutoff (Figure 1B) [9]; by studying these patients, we observed that they were undergoing therapy while all other patients were at their first diagnosis. These data may indicate a possible monitoring role of the kFLC Index during the patient’s therapy.
In conclusions, it would be desirable for neurologists to insert the kFLC Index determination in clinical routine to give a valid aid for the diagnosis and monitoring the patient's treatment.