Medical & Surgical Urology
Open Access
ISSN: 2168-9857
ISSN: 2168-9857
Case Report - (2019)Volume 8, Issue 2
Kidney angiomyolipoma is a rare renal benign neoplasm. In exceptional cases, it can extend to inferior vena cava causing thrombosis. We report here a case of a 33 years old patient who presented an angiomyolipoma caval thrombus during pregnancy.
Angiomyolipoma; Inferior vena cava; Thrombosis; Pregnancy
Kidney angiomyolipoma is a rare benign tumor mostly found as sporadic cases. Literature reported cases of angiomyolipoma associated with thrombosis of the Inferior Vena Cava (IVC) are scarce, those diagnosed and treated during pregnancy are even more exceptional. No therapeutic consensus is found; the decision depends on benefit/risk balance for both the mother and the fetus [1,2].
A 33 years old woman, with no history, pregnant at 39 weeks of gestation, was admitted for lumbar pain with hematuria. Clinical examination did not find any abnormality. Abdominal doppler ultrasound accidentally discovered a floating thrombus of inferior vena cava.
The patient was admitted in our Intensive Care Unit (ICU), with vital and biological monitoring. She received loading dose of unfractionated heparin (50 UI per kg), then maintenance dose (20 UI per kg per hour) with partial thromboplastin time monitoring. The patient didn’t present respiratory distress or syncope.
Multidisciplinary discussion between intensivists, gynecologists, radiologists and vascular surgeons, opted for conservative treatment with anticoagulation for 48 hours to reduce the risk of pulmonary embolism. Other options such as inferior vena cava filter or thrombectomy were discussed but discarded due to the high surgical risk. After 48 hours, caesarian delivery was performed with spinal anesthesia. The immediate postoperative evolution was without complications.
Twelve hours after the surgery, low molecular weight heparin was administrated. Computerized Tomography (CT) scan (Figure 1a) and Magnetic Resonance Imaging (MRI) (Figure 1b) showed bilateral renal angiomyolipoma extending to the right renal vena and the inferior vena cava. Joint medical staff between intensivists, urologists vascular surgeons and radiologists decided on thrombectomy with angioembolization of the tumor. The patient remained stable and didn’t present any complication. Three months after the procedure, follow up imaging showed a reduction of tumor size.
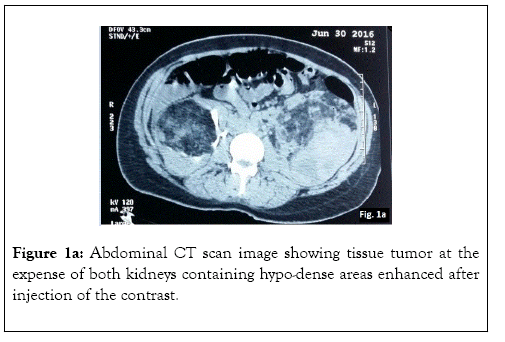
Figure 1a: Abdominal CT scan image showing tissue tumor at the expense of both kidneys containing hypo-dense areas enhanced after injection of the contrast.
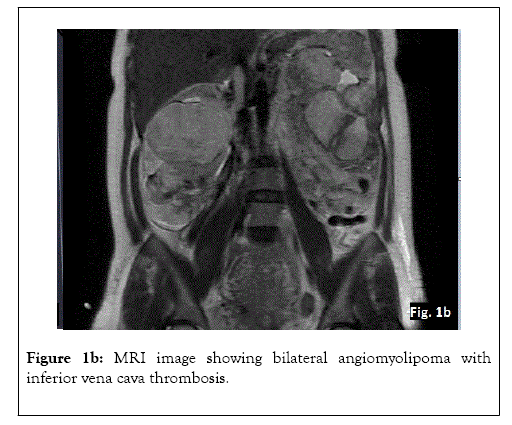
Figure 1b: MRI image showing bilateral angiomyolipoma with inferior vena cava thrombosis.
Angiomyolipoma is a rare renal benign neoplasm which may occur as an isolated phenomenon or as a part of a syndrome which is associated with tuberous sclerosis. The most of the angiomyolipomas are asymptomatic and found incidentally with ultrasound. It is composed of fat cells, smooth muscle cells and blood vessels.
Angiomyolipoma is also the only benign renal tumor that may result in vena cava thrombus. It was first described by Morgan in 1951, [1] and since then, only less than fifty case have been reported with extension to inferior vena cava.
Angiomyolipoma caval thrombus during pregnancy is an exceptional complication of renal angiomyolipoma. It has been shown that pregnancy affects tumor growth as well as the occurrence of hemorrhagic complications by action on progesterone receptors [2]. More than 25% of renal angiomyolipoma carry estrogen and progesterone receptors. Therefore, they are thought to grow during pregnancy or with oral contraceptive use [3]. This hypothesis is supported by a published case of rapid renal angiomyolipoma tumor growth in a woman receiving progesterone contraception [4]. Pregnancy has been identified as a significant risk factor for complications in the case of renal angiomyolipoma. It is therefore essential that women with renal angiomyolipoma who wish to become pregnant be properly informed and undergo close ultrasound monitoring. Furthermore, if there is a surgical indication (tumor size 4 cm or more or previous hemorrhagic complications), renal angiomyolipoma should preferably be surgically removed before the pregnancy [5].
Tumor thrombus during pregnancy is exceptional. However, inferior vena cava thrombectomy during pregnancy outcome is discussed in the few reported cases in the literature. As in the large study by Pillny et al. [6] where among the 53 patients who underwent surgery, the maternal mortality was nil, the authors described 5 fetal deaths, owing to placental abruption. This fetal risk seems to be reasonable compared to the risk of pulmonary embolism.
Current treatment options for renal angiomyolipoma include partial or total nephrectomy (open or laparoscopic), cryoablation, radiofrequency ablation, or arterial embolization [3,7,8] Each patient must be reviewed on a case-by-case basis, but current indications for total nephrectomy are nonfunctioning kidney causing uncontrolled hypertension, local tissue invasion, and high suspicion of malignancy. Our patient not only had significant invasion into the venous system but also had extensive tumor growth encompassing a vast majority of the right kidney.
As regards to the delivery mode for pregnant women with complicated renal angiomyolipoma, there seems to be no consensus within scientific literature. Some authors are afraid that massive tumor bleeding might occur owing to significant intra-abdominal pressure. In the other hand, other authors believe that a complicated renal angiomyolipoma does not constitute, by itself, a contraindication for vaginal delivery. In our case, we gave preference to cesarean delivery given that the complications were potentially serious.
We present a rare case of bilateral renal angiomyolipoma with IVC thrombosis diagnosed and treated during pregnancy. Inferior vena cava thrombosis is often under diagnosed as patients may be asymptomatic. Tumor is the most common cause [7]. The discovery of angiomyolipoma is often fortuitous at imaging. Other circumstances are back pain (41%), palpable mass (11%), hematuria (11%) or its complications [7]. In our case, the initial symptom was lumbar pain with hematuria; which can be secondary to both inferior vena cava thrombosis and the tumor [2,7].
Differential diagnosis of these lesions includes renal cell carcinoma, oncocytoma, and metastatic lesions from primary tumors elsewhere. Radiographic features can usually distinguish these from each other [3,9]. Radiological aspect of angiomyolipoma is characteristic, with enhanced appearance on ultrasound, and hypodense areas in computerized tomography scan (corresponding to the adipose component) and enhancement after contrast injection (corresponding to the vascular component).
Three other cases of angiomyolipoma with inferior vena cava thrombosis during pregnancy were reported [6]. Radical nephrectomy, thrombectomy, or embolization can be proposed. Embolization can also be performed after 12 weeks of gestation with minimal fetal radiation exposure. Management depends on multidisciplinary discussion considering benefit/risk balance, stability of the patient, term of pregnancy, nature, type and location of the thrombus and complication risk of the angiomyolipoma.
In conclusion, renal angiomyolipomas are rare renal neoplasms. They are most of time asymptomatic, but they can grow and become symptomatic during pregnancy. Their extension to inferior vena cava is exceptional. The therapeutic management of this extensive rare tumor thrombus is complex, needing multidisciplinary discussion. The major risk is pulmonary embolism. Further research is needed to assess the safety of any further pregnancy.
Citation: Bkiyar H, Alouani I, Gharibi M, Skikar I, Housni B (2019) Kidney angiomyolipoma with inferior vena cava thrombosis during third trimester of pregnancy. Med Sur Urol 8:218. doi: 10.35248/2168-9857.19.8.218
Received: 04-Mar-2019 Accepted: 25-Mar-2019 Published: 31-Mar-2019 , DOI: 10.35248/2168-9857.19.8.218
Copyright: © 2019 Bkiyar H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.