Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2024)Volume 15, Issue 4
Introduction: Klippel-Trenaunay Syndrome (KTS) is a rare congenital sporadic condition, which is clinically diagnosed by the presence of two of its classical triad features and is commonly seen at birth or early childhood. The triad is composed of cutaneous hemangiomas (port-wine-stains), varicosities, as well as bone and soft tissue hypertrophy, affecting between 2 to 5 in 100,000. Recently, KTS was found to be related to somatic mutations in the Phosphatidylinositol-4-5-biphosphate 3 Kinase Catalytic subunit (PIK3CA) gene, therefore, classified as a PIK3CA-related overgrowth spectrum. These mutations affect the embryological angiogenesis development stage. The KTS features are clinically variable, including systemic and ophthalmological signs and symptoms. Although it can affect nearly any part of the eye, the description of ophthalmological involvement is scarce in the literature.
Case presentation: This study aims to describe a case of KTS in a 30-year-old woman who was found to have retinal and conjunctival telangiectasia, increased excavation and mild retinal vascular tortuosity. The patient best-corrected visual acuity of both eyes was 20/20. The patient presented no signs of retinal or choroidal neovascularization and no evidence of glaucoma. The proper treatment required was only eyeglasses prescription and regular follow-up.
Conclusion: KTS patients must undergo an ophthalmological assessment as some conditions related to this syndrome can be vision-threatening and result in severe visual impairment if not evaluated promptly.
Ocular telangiectasies; Ocular manifestations; Cutaneous hemangiomas; Hypertrophy; Ophthalmology
Klippel-Trenaunay Syndrome (KTS) is a rare congenital sporadic condition clinically diagnosed by the presence of at least two of its classical triad features. The triad is composed of the following: cutaneous hemangiomas (port-wine-stains), varicosities (venous abnormalities), as well as bone and soft tissue hypertrophy. KTS was first described by Maurice Klippel and Paul Trenaunay, two French physicians, in 1900 [1-3]. This syndrome has an estimated incidence rate between 2-5:100,000 with no sex, race or geographical area preference. However, some studies report more cases in males rather than females. It is commonly seen at birth or early childhood. Other synonyms are angioosteohypertrophy syndrome, hemangiectatic hypertrophy and Capillary-Lymphatic-Venous Malformation (CLVM).
Besides the classical triad cited above, literature has indicated multi-systemic involvement as it has been reported to be associated with seizures, developmental delay, hemimegalencephaly, digital abnormalities such as syndactyly, macrodactyly, polydactyly and infrequently, ophthalmic alterations. Therefore, its variable characteristics suggest it is part of a group of disorders instead of an isolated diagnostic entity. Such speculation was confirmed by recent genetic studies, which enabled it to be classified as a PIK3CA-Related Overgrowth Spectrum (PROS). Somatic mutations in the Phosphatidylinositol-4-5-biphosphate 3 Kinase Catalytic subunit (PIK3CA) gene induces activation of Phosphatidylinositol-3-Kinase (PI3K)/protein kinase and cell overgrowth by mammalian Target of Rapamycin 1 (mTOR1) pathway impairment. These mutations affect the embryological angiogenesis development stage [4-6].
In regards to KTS ophthalmologic features, they are variable and scarce in the literature. Conjunctival telangiectasia, retinal varicosities, glaucoma, optic nerve abnormalities, strabismus, orbit varix, cataracts, oculosympathetic palsy, Marcus-Gunn pupil, heterochromia iridum, iris coloboma, choroidal angioma, persistent fetal vasculature and choroidal melanoma are possible findings [7,8].
We report a clinical case of a female patient with Klippel-Trenaunay Syndrome (KTS), presenting with conjunctival and retinal telangiectasia and mild retinal vascular tortuosity.
A 30-year-old woman came for an elective ophthalmologic evaluation. The patient was born following uncomplicated vaginal delivery, with hypertrophy of the lower limbs and a discrete asymmetry, with a bigger left leg and foot. Moreover, patients mother noted the presence of cutaneous flat body hemangiomas since birth.
At the age of 6 years, patient noted lower limb varicose veins, with progressive worsening, which she believes increased after her first menstruation. That was the same time, patient developed vulvovaginal varicosities. At the age of 18 years old, patient sought an evaluation with the vascular team due to lower limbs edema, pain and varicose veins.
The patient denied any known past disease or medication use. The patient clinical and laboratory examination did not demonstrate any evidence of other conditions such as arterial hypertension or anemia. Besides an aunt with mild varicosities, patient reported no other relevant family history. The patient had two children and during her second caesarean section, uterine varices were noted.
The patient’s physical evaluation revealed facial and body asymmetry with increased volume on the left side, irregularly distributed flat hemangiomas (port-wine-stains) on limbs, chest and abdomen, as well as lower limb severe varicosities and edema, left foot syndactyly and bilateral feet macrodactyly. Accordingly, patient was diagnosed with Klippel-Trenaunay Syndrome (KTS), by the vascular team, as patient exhibits the classical triad. The patient was on regular follow-up with the vascular and the orthopedic teams. The patient’s complementary exams showed no significant changes in cranial and orbital magnetic resonance or abdominal ultrasound (Figure 1).

Figure 1: (a): Lower limbs varicosities and edema; (b): Port-wine-stains in the upper back; (c): Left foot syndactyly and; (d): Bilateral feet macrodactyly.
Regarding the ophthalmologic assessment, she complained of mild blurred vision for distant objects in both eyes (Oculi Unitas (OU)) with no other associated symptoms or previous evaluations. Furthermore, she had no history of ophthalmologic illness and denied previous surgeries, traumas, use of illegal substances or glasses.
The distance visual acuity without correction was 20/60 for the Right Eye (RE) and 20/25 for the Left Eye (LE). Subject static refraction displayed RE -1.25 D (diopter) spherical power and LE -0.75 D (spherical power) -0.50 D (cylindrical power) 40° (axis) with best corrected visual acuity of 20/20 OU (Early Treatment Diabetic Retinopathy Study (ETDRS)). On biomicroscopy exam, we observed bilateral bulbar conjunctival telangiectasia with no other changes. Pupillary reflexes and extraocular movements were normal. Intraocular pressure, measured by Goldmann applanation tonometry, was 10 OU. On gonioscopy, the ciliary body was visible (open-angle) OU, without neovascularization or other irregularities (Figure 2).
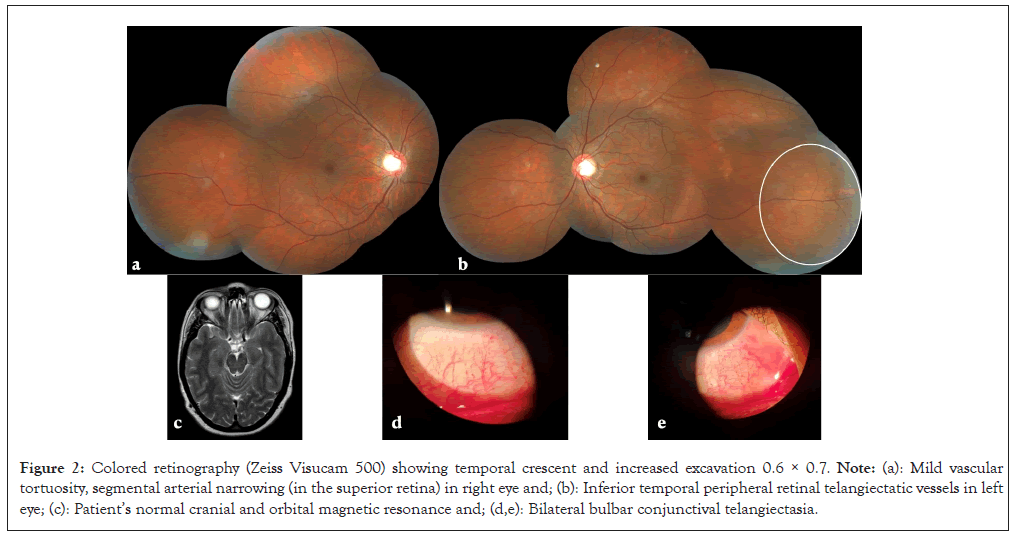
Figure 2: Colored retinography (Zeiss Visucam 500) showing temporal crescent and increased excavation 0.6 × 0.7. Note: (a): Mild vascular tortuosity, segmental arterial narrowing (in the superior retina) in right eye and; (b): Inferior temporal peripheral retinal telangiectatic vessels in left eye; (c): Patient’s normal cranial and orbital magnetic resonance and; (d,e): Bilateral bulbar conjunctival telangiectasia.
Fundoscopy exam of both eyes demonstrated; a temporal crescent and increased excavation 0.6 × 0.7, mild vascular tortuosity, segmental arterial narrowing (in the superior retina) in RE and inferior temporal peripheral retinal telangiectatic vessels in LE. Complementary multimodal examination revealed 570 RE/594 LE corneal pachymetry, no visual field relevant defects (Humphrey HFA II 750, 24-2, SITA-Standard), optic nerve head increased excavation, however, all the other parameters were within the normal limits accordingly to Cirrus Spectral Domain Optical Coherence Tomography (SD-OCT) analysis and normal macular Spectralis SD-OCT. Fundus Fluorescein Angiography (FFA), performed with Zeiss Visucam 500, displayed that all the exam phases were within the normal time limits, with no signs of leakage, either on the disc or peripherally and it highlighted the telangiectatic vessels in LE and mild vascular tortuosity OU (Figure 3).
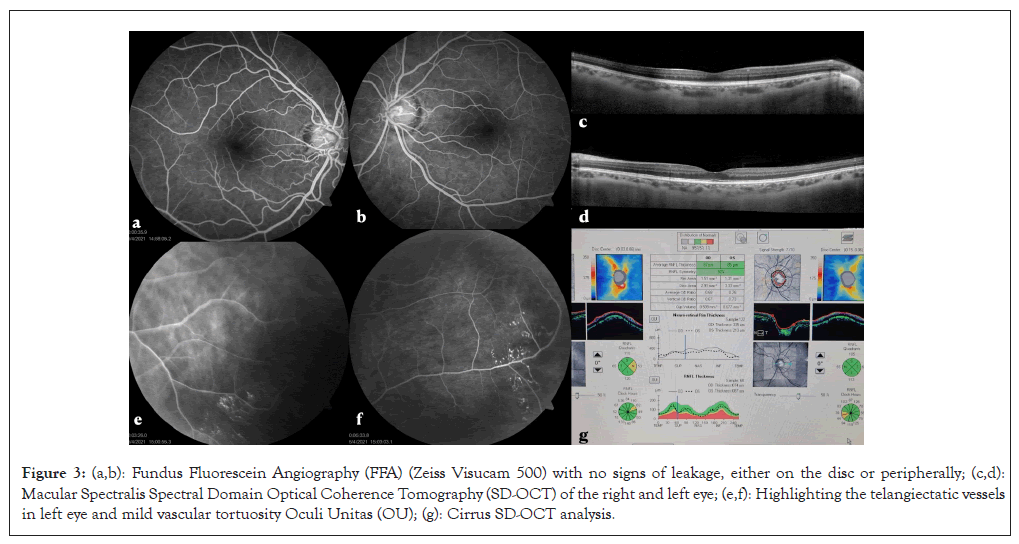
Figure 3: (a,b): Fundus Fluorescein Angiography (FFA) (Zeiss Visucam 500) with no signs of leakage, either on the disc or peripherally; (c,d): Macular Spectralis Spectral Domain Optical Coherence Tomography (SD-OCT) of the right and left eye; (e,f): Highlighting the telangiectatic vessels in left eye and mild vascular tortuosity Oculi Unitas (OU); (g): Cirrus SD-OCT analysis.
As there were no manifestations of retinal or choroidal neovascularization and no retinal capillary non-perfusion areas, the posterior segment findings did not require any specific treatment. Despite the augmented optic nerve excavation, all the complementary assessments did not endorse any evidence of glaucomatous optic neuropathy. Therefore, the only required treatment was an eyeglasses prescription, in accordance with her static refraction and regular follow-up.
Klippel-Trenaunay Syndrome (KTS) is a PIK3CA-Related Overgrowth Spectrum (PROS) syndrome, first described in 1900. KTS has been described by the Hamburg classification as a mixed type of vascular abnormality consisting of lymphatic, capillary and venous deformities [9]. The venous deformities can involve both the superficial and deep venous plexuses and virtually they can occur in any part of the body. Most commonly, they are unilateral, affecting the lower extremities. However, they can alter the upper extremities and/or bilateral limbs. In 1985, Servelle [10], published a series of 768 KTS cases and found that flat angiomata was present in 32% of patients, varicose veins in 36%, edema in 84% and impaired limb elongation in all patients. It is usually a benign condition and having pain and lymphedema are common symptoms. Nevertheless, severe complications may occur and can include deep vein thrombosis, pulmonary embolism, bleeding from gastrointestinal tract vascular malformations and angiosarcoma, among others. Its pathogenesis was recently explained by postzygotic somatic activating mutations in the PIK3CA gene, which occurs in a mosaic pattern. Oncogenic hotspot mutations comprise most cases. The broad phenotypic spectrum from diffuse multisystem to an isolated digit involvement is probably related to the type and timing of mutation development over embryogenesis. There is no cure for KTS and the treatment will vary, basically addressing the patients’ symptoms.
Ocular involvement is as variable as systemic involvement in KTS. There is no epidemiologic data revealing its frequency among KTS patients. The articles published to date reveal a diverse range of possible findings. There is evidence that choroidal hemangiomas, similar to those found in Sturge Weber Syndrome (SWS) and glaucoma are among the most frequent ophthalmic alterations seen in KTS. Notwithstanding, almost any part of the eyeball can be affected and all the following alterations have already been reported in case studies, including conjunctival telangiectasia, retinal varicosities and dilated veins, optic nerve gliomas, optic disc drusen, acquired myelination of the retinal nerve fiber layer, strabismus, orbit varix, cataracts, oculosympathetic palsy, Marcus-Gunn pupil, heterochromia iridum, iris coloboma, persistent fetal vasculature and retinal dysplasia with astrocytic proliferation of the nerve [11].
Olcaysu, et al. [8], reported a case of a 17-year-old boy with KTS that had a unilateral mature cataract and vitreoretinopathy. After the cataract surgery, they could examine the fundus and identified severe vitreoretinopathy and choroidal hemangioma. FFA highlighted in the right eye; leakage from dilated retinal vessels, neovascularization and ischemia. Concerning our patient, despite the mild vascular tortuosity OU and the telangiectatic vessels in LE, there was no leakage, no exudation and no signs of ischemia or neovascularization on fundoscopy or FFA, in contrast to other telangiectatic retinal illnesses such as Coats disease and Eales disease.
Optic Nerve Hypoplasia (ONH) is described by Lambert, et al. [12], as a non-progressive developmental anomaly easily overlooked and frequently associated with endocrine and central nervous system abnormalities. They state that tilted discs can also be hypoplastic and are usually related to bitemporal field depressions crossing the vertical midline. Retinal vascular tortuosity is mentioned as one of the other ocular disorders associated with ONH. Klippel-Trenaunay-Weber syndrome, Duane’s retraction syndrome and Goldenhar-Golin syndrome are cited as some of the illnesses that can be associated with ONH. Although our patient had a temporal crescent, increased excavation and mild vascular tortuosity in OU, we did not find ONH or tilted disc. All those alterations are probably due to developmental defects related to KTS genetic mutations and specific mechanisms that are not yet well understood. The patient augmented excavation does not seem to be related to any type of glaucoma as complementary examination with visual field, Cirrus SD-OCT and corneal pachymetry was undoubtedly normal. The degree of impairment in visual acuity is variable and luckily our patient did not have any visual deficits.
The port-wine stains (nevus flammeus) are a typical feature of the disease. It represents a skin pigmentation anomaly due to the underlying vascular capillary malformation, presenting classically on the facial surface, although it could affect any part of the body. Since it can occur in other conditions with classical ophthalmological involvement, such as Sturge-Weber syndrome, it is relevant for all attendants to become familiar with KTS to guarantee an adequate diagnosis and an optimal follow-up. Our patient had facial, thoracic, abdominal, palmoplantar and vulvar port-wine stains.
Therefore, the patient presented in this case carries many systemic features leading to the diagnosis of KTS and several ocular findings that have already been described in the literature and linked to the syndrome as well. The ocular treatment required will depend on the severity of ocular findings and consequently, the resulting visual impairment. The only required treatment for patient was eyeglasses prescription and regular follow-up as there were no signs of retinal or choroidal neovascularization, no non-perfusion areas and no evidence of glaucoma on complementary examination.
KTS is a very rare systemic syndrome that can include a great range of ocular manifestations. The severity of such alterations is variable and will determine the appropriate treatment. For instance, if retinal neovascularization is identified, then photocoagulation may be required. Also if there is glaucoma development, then management may require eye drops, laser or surgical treatment. The KTS ocular illness early identification and correct treatment will define the patients’ visual acuity and quality of life.
Therefore, ophthalmologists must recognize and understand this condition as it can bring serious visual deterioration. A patient diagnosed with KTS should have an ophthalmologic assessment as soon as possible and regular follow-up depending on the alterations identified. Moreover, KTS, especially its ocular findings, merit further study for a better understanding.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images, including personal and clinical details along with identifying pictures.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Lemos RD, Hamade AMA, Araujo DC, Hall LN, Berezovsky M, Nascimento MA (2024) Klippel-Trenaunay Syndrome Ocular Manifestations: A Case Report. J Clin Exp Ophthalmol. 15:985.
Received: 27-Jun-2024, Manuscript No. JCEO-24-32056; Editor assigned: 01-Jul-2024, Pre QC No. JCEO-24-32056 (PQ); Reviewed: 15-Jul-2024, QC No. JCEO-24-32056; Revised: 22-Jul-2024, Manuscript No. JCEO-24-32056 (R); Published: 29-Jul-2024 , DOI: 10.35248/2155-9570.24.15.985
Copyright: © 2024 Lemos RD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.