Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research - (2024)Volume 13, Issue 8
Background: Caesarean section (CS) is a commonly performed surgical procedure in obstetrics that has significantly improved maternal and fetal outcomes worldwide in the 20th century. However, in the 21st century, the frequency of Caesarean section operations has surpassed the World Health Organization (WHO) recommendations due to unnecessary and inappropriate indications. There is a notable lack of data on this issue in Somaliland, particularly in the Burao district where no previous studies on Caesarean section have been conducted. This study aims to fill these research gaps by examining the level of maternal knowledge, attitudes, perceptions, and associated factors regarding Caesarean section among pregnant and postpartum women in Burao district.
Objective: To assess the knowledge, attitude, and perception towards caesarean section and its associated factors among pregnant and postpartum women attending maternal health units in Burao District, Somaliland.
Methods: A cross-sectional study design was employed to interview pregnant and postpartum women attending four maternal health centers in Burao district. Participants completed a questionnaire covering socio-demographic characteristics, obstetric histories, and knowledge, attitudes, and perceptions towards Caesarean section . Data were analyzed using Stata software and presented as frequencies and percentages.
Results: The study, involving 162 respondents, highlighted demographic and educational variations that influence delivery preferences and methods among women in the Burao District, Somaliland. Of the respondents, 39.51% were aged 22-28, and 23.46% were aged 15-21. A significant proportion (33.33%) of the women was illiterate, whereas 33.96% of their husbands had basic education. University enrolment rates were low, with only 8.64% of mothers and 23.27% of husbands having higher education. Regarding delivery preferences, 74.19% of women preferred vaginal delivery for their first birth, while 25.81% opted for a caesarean section. For their most recent birth, 70.00% delivered vaginally, whereas 30.00% delivered via caesarean section.The study also reveals significant associations between various factors and the attitudes, knowledge, and perceptions regarding caesarean sections among mothers. The mode of first and last delivery was significantly linked to mothers' knowledge about caesarean sections, indicating that personal experience with different delivery methods influences awareness. Respondents' attitudes towards caesarean sections were significantly associated with their monthly income and the method of their most recent delivery, highlighting the role of socio-economic factors and recent experiences in shaping attitudes. Additionally, mothers' education levels significantly impacted their perceptions of caesarean sections, with higher education levels correlating with more informed and favorable views.
Conclusions: The study reveals that pregnant and post-partum women have good overall knowledge, positive attitudes, and positive perceptions towards Caesarean section , with rates of 64.81%, 51.85%, and 55.56%, respectively. However, the rates of Caesarean section for the first and last delivery modes were 25.81% and 30.0%, respectively, with elective Caesarean section at 5.45%.These findings emphasize the importance of addressing personal experience, socio-economic factors, and education in maternal health initiatives related to caesarean sections.
Recommendations: Maternal health programs should prioritize tailored education and awareness campaigns about caesarean sections, particularly for mothers with varied delivery experiences. Addressing socio-economic disparities and enhancing educational initiatives are crucial to ensure all mothers receive accurate information and support. These measures will promote informed decision-making and positive attitudes towards caesarean sections.
Knowledge, Attitude, Perception, Caesarean Section, Associated Factors, Pregnant Women, Postpartum Women, Maternal Health, Burao District, Somaliland.
In the twenty-first century, childbirth typically occurs through either vaginal delivery or caesarean delivery (CS). When vaginal delivery is not feasible, caesarean delivery serves as an alternative, involving an incision in the uterine wall to ensure the safety of both mother and child [1]. Caesarean section is one of the most common surgical procedures in obstetrics and has significantly improved obstetric care globally, reducing maternal and fetal mortality [2].
Caesarean sections can be elective, planned before labor, or emergency operations based on medical necessity during labor. The primary indication for elective Caesarean section includes a narrow pelvis, where the pelvic outlet is less than 29.5 cm wide, or an interspinal measure of less than 8 cm [3]. However, Caesarean section without medical necessity is associated with higher perinatal complications compared to vaginal birth (VB), affecting both short- and long-term maternal and neonatal outcomes. Despite this, Caesarean section rates have increased globally without clear evidence of reduced morbidity and mortality when Caesarean section is not medically justified [2].
Medical experts consider Caesarean section generally safe, albeit with higher complication risks than vaginal delivery [4]. Decisions regarding Caesarean section often hinge on the best interests and safety of the mother and child [5]. The World Health Organization (WHO) recommends a Caesarean section rate of 10%-15%, noting that higher rates may not correlate with improved health outcomes [6]. In Sub-Saharan Africa, including Somalia, negative perceptions and limited access to Caesarean section contribute to higher perinatal and neonatal mortality [7].
Maternal mortality remains a global concern, with Sub-Saharan Africa, including Somalia, accounting for nearly 70% of maternal deaths in 2020. Somalia's maternal mortality rate (MMR) dropped from 732/100,000 live births in 2015 to 692/100,000 in 2020, yet remains high compared to neighbouring countries [8]. The national Caesarean section rates vary, with developed countries like the UK and USA reporting rates of 23.8% and 32.8% respectively, while Somalia reports significantly lower rates [9].
Studies indicate varying levels of maternal knowledge about Caesarean section. In Manipur, India, 92.7% of pregnant women had inadequate knowledge regarding Caesarean section [10]. In Nigeria, 82.3% had heard about Caesarean section, but many were unaware of specific details [11]. Conversely, in Saudi Arabia, 94.2% of women knew that Caesarean section could save a newborns life [12].These findings highlight the need for enhanced maternal education on Caesarean section.
Attitudes towards Caesarean section vary widely. In Sweden, Somali women preferred Caesarean section due to concerns related to female genital mutilation [13]. In Nigeria, 66% of pregnant women would not accept Caesarean section if indicated [14]. Studies in Jordan found that most women preferred vaginal delivery, with attitudes influenced by past experiences and cultural beliefs [15].
Multiple factors influence maternal acceptance of Caesarean section. Repeat Caesarean section, dystocia, breech presentation, and fetal distress are common indications [6]. Studies indicate that financial incentives, fear of labor pain, and concerns about healthcare quality also drive higher Caesarean section rates [16]. Socio-economic status, education level, and maternal age significantly impact Caesarean section acceptance [17].
Despite limited data, studies indicate Somaliland women face higher risks of Caesarean section due to circumcision-related concerns and the influence of healthcare providers. This study seeks to assess factors affecting maternal knowledge and attitudes towards Caesarean section in Burao district, enhancing community understanding and acceptance when necessary.
General Objective
The purpose of the study is to assess knowledge, attitude and perception towards Caesarean Section and Its Associated Factors among Pregnant and Postpartum women Attending Maternal Health Units in Burao District, Somaliland, in August 2023.
Specific Objectives
• To identify Knowledge towards Caesarean Section and Its Associated Factors Among Pregnant and Postpartum women Attending Maternal Health Units in Burao District, Somaliland, in August 2023.
• To assess the attitude towards elective caesarean section Among Pregnant and Postpartum women Attending Maternal Health Units in Burao District, Somaliland, in August 2023.
• To find out the factors that are associated with maternal knowledge and attitude towards caesarean section Among Pregnant and Postpartum women Attending Maternal Health Units in Burao District, Somaliland, in August 2023.
Study area and Period
This study was conducted at obstetric health units in Burao District, Somaliland, from May 15 to June 30, 2023. Burao, founded in the late 18th century, is the second largest city in Somaliland (UN-HABITAT, 2009). The district is served by two public secondary hospitals, ten private secondary hospitals, and five primary maternal and child health (MCH) centers providing obstetric services. We purposefully selected four of the most populated health centers: Burao General Hospital, Central MCH, Daaru-Hanan, and Sheikh Khalifa Hospital.
Study design
An institutional cross-sectional survey was conducted to assess women's knowledge, attitudes, perceptions, and associated factors regarding caesarean sections among pregnant and postpartum women attending selected obstetric health units in Burao District.
Study Participants
Study participants were pregnant and postpartum women who attend at obstetric health units during the data collection period. In terms of eligibility requirements, the sample was taking from pregnant women and postpartum who were available during data collection, were not in labour, were fully conscious, and were mentally competent.
Study population
The overall population of this study was composed of all pregnant and postpartum women who attended the selected obstetric health centers in Burao District during data collection.
Sample size determination
During data collection, 162 women composed of pregnant and postpartum women, who visited the study area were interviewed. Since the size of target population was less than 10,000, we employed a reduction formula to enroll the study participants. Although our target sample size was 384; we decided to take 162 samples due to financial and time constraints. The final sample size was drawn proportionately from each health center, and the participants were selected by using convenient sampling method. We assumed that the preferred health centers were sufficient to represent the community in Burao city and its surroundings. The formula below was used to determine the sample size (Fisher et al., 1991; cited in Kothari, 2004). Thus, the sample size was being calculated as following:
n=the desired sample size.
z=the standard normal deviation, which corresponds to the 95% confidence level (1.96).
p=the proportion of the target population estimated to have the particular characteristic being studied. In this study, p will be the proportion of pregnant women who will attend Burao General Hospital, which will be estimated at 50%. Hence, P will be 0.5. Since we did not have any related studies carried out in the country as well as in neighboring countries, we assume that the proportion of pregnant mothers' knowledge, attitude and perception is all about 50 percent.
q=1-0.5 p
d=degree of accuracy desired, usually set at 0.05
1.962 x 0.5 x 0.5=3.8416*0.5*0.5=0.9604/0.0025=384. Hence, the sample size will be 384.
Sampling Procedures
A convenience sampling method was used to recruit study participants, including those available during data collection. Additionally, purposive sampling was employed to select the study area, which included four major maternity health centers: Burao General Hospital, Central MCH, Sheikh Khalifa Hospital, and Daaru-Hanaan Hospital. These centers, comprising three public institutions and one private hospital, are among the most frequented in the district and serve a diverse range of clients. This selection allowed for a comprehensive assessment of opinions from individuals with varied backgrounds.
Study Variables
Dependent variables
• Knowledge
• Attitude
• Perception
Independent variable
• Socio-demographic Factors
• Obstetric history of mothers
Inclusion and Exclusion criteria
Inclusion Criteria
All pregnant and postpartum women who attending at Obstetric health centers who were not in labour, were fully conscious, mentally competent, and available during data collection were enrolled in the study.
Exclusion criteria
All pregnant and postpartum women attending at antenatal care who are unconscious, in labour, or mentally incapacitated at the time of data collection.
Data collection Methods and procedures
The researchers distributed a questionnaire, translated into Somali, to collect primary data on the levels of knowledge, attitudes, and perceptions regarding caesarean sections among pregnant women. To ensure data accuracy and completeness, each questionnaire was meticulously reviewed daily by the researchers to confirm that it was fully completed.
Data collection tools/instruments
The data-gathering instrument for this study was a standardized questionnaire comprising three sections. The first part included two sections: Section One collected socio-demographic data, while Section Two gathered information on obstetric history. The second part contained six binary questions (yes/no) assessing knowledge about caesarean sections, with a maximum score of 6 and a minimum of 0 (one point per correct answer). The third part included 16 questions on attitudes and 9 questions on perceptions of caesarean sections, rated on a Likert scale from 1 (Strongly Disagree) to 5 (Strongly Agree), with a maximum score of 60 and a minimum of 12. This questionnaire was selected for its simplicity in administration, enabling the collection of extensive data from a broad sample efficiently and cost-effectively.
Analysis and presentation of results
The collected data were entered into Epi-Data 3.1 for initial handling and then imported into Stata software package version 20 for further analysis. Data cleaning, coding, and analysis were performed using Stata. To evaluate the knowledge, attitudes, and perceptions (KAP) of pregnant and postpartum women regarding caesarean sections, both bivariate and multivariable logistic regression models were employed. The KAP outcomes were analyzed with socio-demographic variables to determine associations. The degree of association between the dependent (KAP) and independent (socio-demographic) variables was represented using crude odds ratios (COR) and adjusted odds ratios (AOR), with 95% confidence intervals (CI). Statistical significance was defined as a p-value of 0.05 or less. Summary statistics were computed, and the results were presented through tables and graphs.
Ethical considerations
Before participating, all individuals were asked to provide informed consent, with a clear explanation that participation was optional and that the collected information would be used solely for research purposes and kept anonymous. Throughout the study, respondents were treated with transparency and integrity regarding the study objectives, procedures, potential outcomes, and any associated demands or discomforts. Approval was obtained from the University of Burao's Research Ethics Committee. Participant information was handled confidentially, and no monetary incentives were offered to avoid bias in responses. Participation was entirely voluntary, with no coercion or undue influence exerted to encourage involvement.
Socio-demographic characteristics among pregnant women in Burao Health centers, n=162
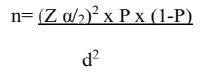
In a study of 162 respondents, the majority were women aged 22-28 (39.51%), followed by those aged 15-21 (23.46%). Education levels varied, with 33.33% of the women being illiterate while 33.96% of their husbands had basic schooling; however, 8.64% of the women and 23.27% of their husbands had attained university education. A significant portion of the women (82.72%) were housewives, whereas 17.28% were employed. Family sizes tended to be large, with 42.21% having 5-7 members and 24.03% having 7 or more. In terms of income, 27.81% of families earned $350 or more per month, while 22.52% earned between $50-150 per month. Nearly all participants (97.53%) were married, and a majority (83.33%) were urban residents, with the remaining 16.67% living in rural areas Table 1, Figure 1.
| Variable | Frequency | Percentage |
|---|---|---|
| Age | ||
| 15-21 | 38 | 23.46 |
| 22-28 | 64 | 39.51 |
| >28 | 60 | 37.04 |
| Marital Status | ||
| Divorced | 4 | 2.47 |
| Married | 158 | 97.53 |
| Mother education level | ||
| Illiterate | 54 | 33.33 |
| Primary school | 52 | 32.1 |
| Secondary | 42 | 25.93 |
| University | 14 | 8.64 |
| Husband education level | ||
| Illiterate | 42 | 26.42 |
| Primary school | 54 | 33.96 |
| Secondary | 26 | 16.35 |
| University | 37 | 23.27 |
| Occupation Status | ||
| Unemployed (household) | 134 | 82.72 |
| Employee | 28 | 17.28 |
| Family members | ||
| 02-Apr | 52 | 33.77 |
| 05-Jul | 65 | 42.21 |
| >7 | 37 | 24.03 |
| Monthly income | ||
| 50-150 | 34 | 22.52 |
| 151-250 | 37 | 23.5 |
| 251-350 | 38 | 25.17 |
| >350 | 42 | 27.81 |
| Place of residency | ||
| Urban | 135 | 83.33 |
| Rural | 27 | 16.67 |
Table 1: Socio-demographic characteristics among pregnant women in Burao Health centers, 2023 n=162
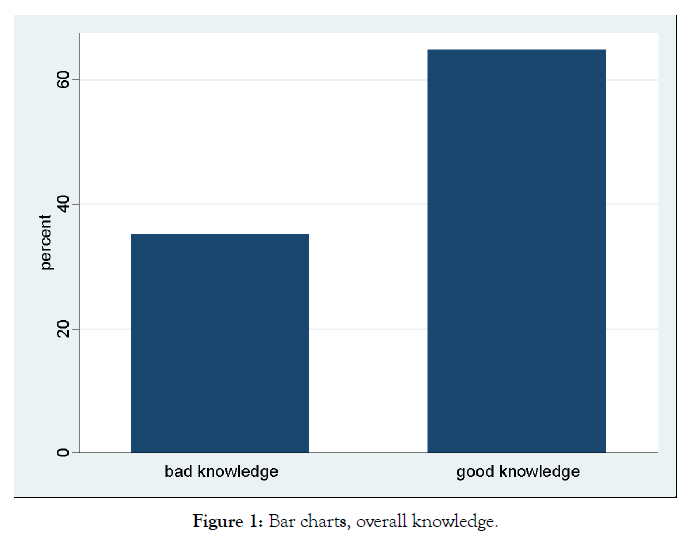
Figure 1. Surgical training questionnaire
Obstetric history of mothers among pregnant women in Burao Health centers, n=162
In the study of 162 women, obstetric history revealed that most women (40.25%) married between the ages of 19 and 23, closely followed by those who married between 14 and 18 years old (39.62%). The majority of participants experienced two to three instances of gravidity (45.68%) and parity (45.06%). Regarding abortion, 28.40% of women had one abortion, and 6.79% had two or more. Concerning delivery methods, 74.19% of women had a vaginal delivery for their first birth, while 25.81% underwent a caesarean section (CS). For their most recent delivery, 70.00% delivered vaginally, whereas 30.00% delivered via CS Table 2.
| Variable | Frequency | Percentage |
|---|---|---|
| Age of your first marriage | ||
| 14-18 | 63 | 39.62 |
| 19-23 | 64 | 40.25 |
| >23 | 32 | 20.13 |
| Gravidity | ||
| Once | 31 | 19.14 |
| Two-three times | 74 | 45.68 |
| Four times and more | 57 | 35.19 |
| Parity | ||
| Zero | 14 | 8.64 |
| Once | 24 | 14.81 |
| Two-three times | 73 | 45.06 |
| Four times and more | 51 | 31.48 |
| Abortion | ||
| Zero | 105 | 64.81 |
| Once | 46 | 28.4 |
| More than once | 11 | 6.79 |
| Age of your first delivery | ||
| 15-19 | 54 | 37.76 |
| 20-24 | 57 | 39.86 |
| >24 | 32 | 22.38 |
| Method of your first delivery | ||
| Vaginal delivery | 115 | 74.19 |
| Cesarean delivery | 40 | 25.81 |
| Method of last delivery | ||
| Vaginal delivery | 98 | 70 |
| Cesarean delivery | 42 | 30 |
Table 2: Obstetric history of mothers among pregnant women in Burao Health centers, n=162
Knowledge of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
In the study of 162 women, 64% demonstrated good knowledge about caesarean sections (CS), while 35% had poor knowledge. All participants had heard of CS, and 66.05% had undergone the procedure. When asked about past surgeries, 33.95% reported having been operated on, with 54.55% having had CS once and 45.45% undergoing the procedure twice or more. Among those who had CS, 94.55% were for medical reasons, and 5.45% were elective. Consent for surgery was primarily given by husbands (80%) and relatives (20%). A significant majority (77.78%) believed that a woman could have a vaginal birth following a CS. Additionally, 72.84% thought that blood transfusions might be necessary before or after CS. Universally, all respondents believed that CS could save the lives of newborns, and nearly all (98.77%) agreed it could save the lives of mothers Table 3.
| Variable | Frequency | Percentage |
|---|---|---|
| Have you ever heard about CS? | ||
| Yes | 162 | 100 |
| No | 0 | 0 |
| If yes, have you ever been operated on? | ||
| Yes | 55 | 33.95 |
| No | 107 | 66.05 |
| How many times have you been operated on? | ||
| Once | 30 | 54.55 |
| Twice and more | 25 | 45.45 |
| What were the reasons for your operation? | ||
| Medical indication | 52 | 94.55 |
| Non-medical indication | 3 | 5.45 |
| If it is non-medical indication, what enforced you to undergo CS? | ||
| My own choice | 3 | 100 |
| Were you asked to sign an informed consent before a CS? | ||
| Yes | 55 | 100 |
| If yes, who signed the consent form? | ||
| Your husband | 44 | 80 |
| Other relatives | 11 | 20 |
| Can women achieve vaginal delivery after CS? | ||
| Yes | 126 | 77.78 |
| No | 36 | 22.22 |
| Does blood transfusion become essential for CS after and before the procedure? | ||
| Yes | 118 | 72.84 |
| No | 44 | 27.16 |
| Dose Cesarean section saves the life of newborn? | ||
| Yes | 162 | 100 |
| Does CS safe the life of mothers? | ||
| Yes | 160 | 98.77 |
| No | 2 | 1.23 |
| Women’s Overall knowledge towards CS | ||
| Bad knowledge | 57 | 35.19 |
| Good knowledge | 105 | 64.81 |
Table 3: Knowledge of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
Attitude of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
In the study examining women's attitudes toward caesarean sections (CS), 51% had a positive attitude, while 48% had a negative attitude. A significant portion of participants (46.30%) strongly agreed they would be prepared to undergo CS if medically indicated, whereas 4.32% strongly disagreed. Nearly half of the women (45.06%) strongly disagreed with the notion that CS is a woman's right to choose without medical indication. The majority (59.88%) strongly agreed that CS should only be allowed when vaginal delivery is impossible, while 8.02% strongly disagreed. Additionally, 12.35% of women agreed that physicians influence their decision to undergo CS, with 4.94% strongly Figure 2, Table 4.
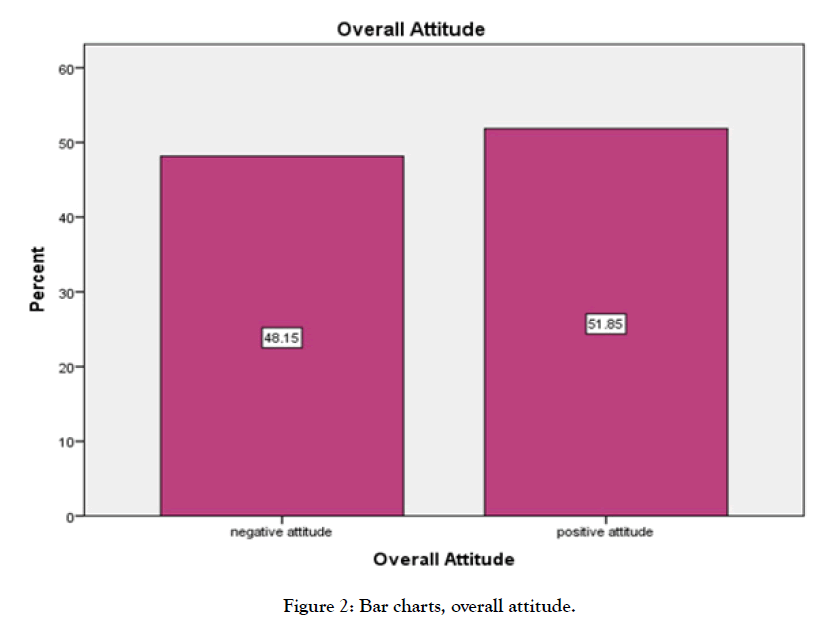
Figure 2. Surgical training questionnaire.
| Variable | Frequency | Percentage |
|---|---|---|
| Willing to undergo CS if indicated | ||
| Strongly disagree | 7 | 4.32 |
| Disagree | 9 | 5.56 |
| Undecided | 13 | 8.02 |
| Agree | 58 | 35.8 |
| Strongly agree | 75 | 46.3 |
| It is a woman’s right to choose a caesarean section for herself, even if there are no medical reasons to have it | ||
| Strongly disagree | 75 | 45.06 |
| Disagree | 35 | 21.6 |
| Undecided | 14 | 8.64 |
| Agree | 31 | 19.14 |
| Strongly agree | 9 | 5.56 |
| CS delivery is only allowed when vaginal delivery is impossible | ||
| Strongly disagree | 13 | 8.02 |
| Disagree | 7 | 4.32 |
| Undecided | 7 | 4.32 |
| Agree | 38 | 23.46 |
| Strongly agree | 97 | 59.88 |
| Cesarean is more comfortable than vaginal delivery | ||
| Strongly disagree | 75 | 46.3 |
| Disagree | 34 | 20.99 |
| Undecided | 21 | 12.96 |
| Agree | 23 | 14.2 |
| Strongly agree | 9 | 5.56 |
| Pain after CS makes mothers unable to nurse their babies | ||
| Strongly disagree | 19 | 11.73 |
| Disagree | 25 | 15.43 |
| Undecided | 29 | 17.9 |
| Agree | 64 | 39.51 |
| Strongly agree | 25 | 15.43 |
| People with higher social status mostly choose caesarean delivery over vaginal delivery | ||
| Strongly disagree | 54 | 33.33 |
| Disagree | 28 | 17.28 |
| Undecided | 27 | 16.67 |
| Agree | 41 | 25.31 |
| Strongly agree | 12 | 7.41 |
| Physicians encourage women that caesarean is an easy and comfortable birth method | ||
| Strongly disagree | 61 | 37.65 |
| Disagree | 49 | 30.25 |
| Undecided | 24 | 14.81 |
| Agree | 20 | 12.35 |
| Strongly agree | 8 | 4.94 |
| Physicians do not explain about vaginal delivery and do not encourage women to perform vaginal delivery | ||
| Strongly disagree | 49 | 30.25 |
| Disagree | 38 | 23.46 |
| Undecided | 30 | 18.52 |
| Agree | 31 | 19.14 |
| Strongly agree | 14 | 8.64 |
| I am scared of getting fistula and deformed genitalia after vaginal delivery | ||
| Strongly disagree | 44 | 27.16 |
| Disagree | 44 | 27.16 |
| Undecided | 15 | 9.26 |
| Agree | 43 | 26.54 |
| Strongly agree | 26 | 9.88 |
| I am terrified vaginal delivery because of FGM | ||
| Strongly disagree | 22 | 13.58 |
| Disagree | 19 | 11.73 |
| Undecided | 19 | 11.73 |
| Agree | 35 | 21.6 |
| Strongly agree | 67 | 41.36 |
| I am afraid that my baby will have problems during vaginal delivery | ||
| Strongly disagree | 60 | 37.04 |
| Disagree | 53 | 32.72 |
| Undecided | 9 | 5.56 |
| Agree | 25 | 15.43 |
| Strongly agree | 15 | 9.26 |
| I do not trust the information and skills of midwives in performing vaginal delivery | ||
| Strongly disagree | 69 | 42.59 |
| Disagree | 44 | 27.16 |
| Undecided | 14 | 8.64 |
| Agree | 20 | 12.35 |
| Strongly agree | 15 | 9.26 |
| Babies born by caesarean delivery are more intelligent | ||
| Strongly disagree | 97 | 59.99 |
| Disagree | 34 | 20.99 |
| Undecided | 18 | 4.94 |
| Agree | 8 | 4.94 |
| Strongly agree | 5 | 3.09 |
| I am terrified of labour pain | ||
| Strongly disagree | 20 | 12.35 |
| Disagree | 27 | 16.67 |
| Undecided | 28 | 17.28 |
| Agree | 61 | 37.65 |
| Strongly agree | 16 | 16.05 |
| Seeing the baby immediately after vaginal delivery is a pleasure for the mother | ||
| Strongly disagree | 6 | 3.7 |
| Disagree | 6 | 3.7 |
| Undecided | 7 | 4.32 |
| Agree | 48 | 29.63 |
| Strongly agree | 95 | 58.64 |
| Women who deliver their babies by caesarean section miss an important life experience | ||
| Strongly disagree | 30 | 18.52 |
| Disagree | 31 | 19.14 |
| Undecided | 26 | 16.05 |
| Agree | 45 | 27.78 |
| Strongly agree | 30 | 18.52 |
| Women’s Overall attitude towards CS | ||
| Negative attitude | 78 | 48.15 |
| Positive attitude | 84 | 51.85 |
Table 4: Attitude of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
Perception of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
In the study regarding women's perceptions of caesarean sections (CS), 55.56% had a good perception, while 44.44% had a bad perception. When asked if their husbands preferred CS for greater sexual satisfaction, a majority (53.09%) strongly disagreed, while 3.70% strongly agreed. Additionally, when asked if they were concerned about decreased sexual satisfaction after vaginal delivery, the majority (56.79%) strongly disagreed, and only 1.85% strongly agreed Figure 3, Table 5.
Figure 3. Surgical training questionnaire.
| Variable | Frequency | Percentage |
|---|---|---|
| It Is a Taboo in My Culture to Have Cs | ||
| Strongly disagree | 100 | 61.73 |
| Disagree | 34 | 20.99 |
| Undecided | 13 | 8.02 |
| Agree | 12 | 7.41 |
| Strongly agree | 3 | 1.85 |
| My Husband Is Not Capable to Pay for Surgery | ||
| Strongly disagree | 67 | 41.36 |
| Disagree | 53 | 32.72 |
| Undecided | ||
| Agree | 28 | 17.28 |
| Strongly agree | 13 | 8.02 |
| The God will not allow me to deliver through Cs | 1 | 0.62 |
| Strongly disagree | 107 | 66.05 |
| Disagree | 39 | 24.07 |
| Undecided | 8 | 4.94 |
| Agree | 5 | 3.,09 |
| Strongly agree | 3 | 1.85 |
| If I Have CS Done the Mark Will Be on Me Forever | ||
| Strongly disagree | 18 | 11.11 |
| Disagree | 17 | 10.49 |
| Undecided | 33 | 20.37 |
| Agree | 56 | 34.57 |
| Strongly agree | 38 | 23.46 |
| I will not perform my daily activities if I deliver through Cs | ||
| Strongly disagree | 28 | 17.28 |
| Disagree | 30 | 18.52 |
| Undecided | 40 | 24.69 |
| Agree | 43 | 26.54 |
| Strongly agree | 21 | 12.96 |
| I am afraid of caesarean section complications | ||
| Strongly disagree | 21 | 13.04 |
| Disagree | 23 | 14.29 |
| Undecided | 16 | 9.94 |
| Agree | 61 | 37.89 |
| Strongly agree | 40 | 24.84 |
| My husband prefers caesarean section due to more sexual satisfaction | ||
| Strongly disagree | 86 | 53.09 |
| Disagree | 32 | 19.75 |
| Undecided | 30 | 18.52 |
| Agree | 8 | 4.94 |
| Strongly agree | 6 | 3.7 |
| I am worried of decreased sexual satisfaction following vaginal delivery | ||
| Strongly disagree | 92 | 56.79 |
| Disagree | 37 | 22.84 |
| Undecided | 26 | 16.05 |
| Agree | 4 | 2.47 |
| Strongly agree | 3 | 1.85 |
| Women’s Overall perception towards CS | ||
| Negative perception | 72 | 44.44 |
| Positive perception | 90 | 55.56 |
Table 5: Perception of mothers towards CS among pregnant women in Burao health centers, 2023 n=162
Association between independents and knowledge for bivariate and multiple logistic regression analysis
Initial crude analysis indicated significant associations between variables such as family size, monthly income, method of first delivery and method of last delivery with respondents' knowledge about caesarean sections. However, after conducting multivariate (adjusted) analysis, these associations were no longer significant, leading to the conclusion that there is no substantial relationship between these variables and maternal knowledge. In contrast, both multivariate and bivariate analyses revealed that the mode of first and last delivery was significantly associated with knowledge. Specifically, participants who had undergone first and last caesarean delivery were found to have 4.5 and 6.32 times greater knowledge compared to those who had a vaginal delivery respectively Table 6.
| Knowledge status | Odds ratio 95% CI | |||
|---|---|---|---|---|
| Covariates | Poor knowledge | Good knowledge | Crude | Adjusted |
| Family members | ||||
| 02-Apr | 25(44.64) | 27(27.55) | Ref | Ref |
| 05-Jul | 16(28.57) | 49(50.00) | 2.84(1.3-6.2)* | 2.12(0.74.6.02) |
| >7 | 15(26.79) | 22(22.45) | 1.36(0.58-3.2) | |
| Monthly income | ||||
| 50-150 | 15(27.78) | 19(19.59) | Ref | |
| 151-250 | 11(20.37) | 26(26.80) | 1.9(0.7-4.10) | 1.9(0.57-6.30) |
| 251-350 | 7(12.96) | 31(31.96) | 3.45(1.2-10.1)* | 2.99(0.83-10.7) |
| >350 | 21(38.89) | 21(21.65) | 0.8(0.3-1.10)* | 0.71(0.22-2.9) |
| Method of your first delivery | ||||
| Vaginal delivery | 48(92.31) | 67(65.05) | Ref | Ref |
| Caesarean delivery | 4(7.69) | 103(100.00) | 6.4(2.2-19.3)* | 4.5(3.8-9.3)* |
| Method of last delivery | ||||
| Vaginal delivery | 45(95.74) | 53(56.99) | Ref | Ref |
| Caesarean delivery | 2(4.26) | 40(43.01) | 16.9(3.9-74.1)* | 6.32(1.23-32.4)* |
Table 6: Association between independents and knowledge for bivariate and multiple logistic regression analysis, n=162
The association between independents and attitude for bivariate and multiple logistic regression analysis
Crude and multiple analyses reveal significant associations between monthly income and the method of last delivery with respondents' attitudes toward cesarean sections. Initially, one income categories—$151-$250 and $251-$350—showed significant associations with attitude in the crude analysis. However, after adjusting for multiple variables, only the $251-$350 income category retained its significance, while the $151-$250 category did not. Additionally, participants who had undergone a cesarean delivery exhibited 2.4 times more positive attitudes compared to those who had a vaginal delivery. Similarly, individuals in the $251-$350 income category displayed 3.36 times more positive attitudes than those in the $50-$150 income category, indicating that both higher income levels and cesarean delivery experience contribute to more favorable attitudes towards cesarean sections Table 7.
| Attitude status | Odds ratio 95% CI | |||
|---|---|---|---|---|
| Independents | Negative Attitude | Positive Attitude | Crude | Adjusted |
| Monthly income | ||||
| 50-150 | 20(27.78) | 14(17.72) | Ref | Ref |
| 151-250 | 14(19.44) | 23(29.11) | 2.35(1.90-6.09) | 1.10(0.70-564) |
| 251-350 | 11(15.28) | 27(34.81) | 3.50(1.31-9.33)* | 3.36(1.13-9.95)* |
| >350 | 27(37.50) | 15(18.99) | 0.7(0.31-2.01) | 0.73(0.25-20.6) |
| Method of last delivery | ||||
| Vaginal delivery | 51(79.69) | 47(61.84) | Ref | Ref |
| Caesarean delivery | 13(20.31) | 29(38.16) | 2.42(1.13-5.20)* | 2.4(2.81-7.4)* |
Table 7: This shows association between independents and attitude for bivariate and multiple logistic regression analysis
The association between independents and perception for bivariate and multiple logistic regression analysis
After both crude and multiple analyses, only the level of education-specifically, having a university education-remained significantly associated with perception toward caesarean sections. Participants with a university education were found to have 99.76% less likelihood of holding a negative bad perception compared to those who were illiterate. This indicates that higher educational attainment is strongly linked to good perception towards caesarean sections, underscoring the impact of education on shaping perceptions in this context Table 8.
| Perception status | Odds ratio 95% CI | |||
|---|---|---|---|---|
| Covariates | Bad perception | Good perception | Crude Odds ratio | Adjusted Odds ratio |
| Mother education level | ||||
| Illiterate | 20(27.78) | 34(37.78) | Ref | Ref |
| Primary school | 24(33.33) | 28(31.11) | 0.69(0.315-1.49) | 0.70(0.29-1.73) |
| Secondary | 17(23.61) | 25(27.78) | 0.87(0.32-1.10) | 1.02(0.38-2.73) |
| University | 11(15.28) | 3(3.33) | 0.16(0.03-0.64)* | 0.0024(0.053-0.91)* |
| Occupation Status | ||||
| Household | 54(75.00) | 80(88.89) | Ref | Ref |
| Employee | 18(25.00) | 10(11.11) | 0.380(0.16-0.87)* | 0.54(0.21-1.40) |
| Monthly income | ||||
| 50-150 | 14((20.29) | 20(24.39) | Ref | Ref |
| 151-250 | 14(20.29) | 23(28.05) | 1.15(0.44-2.99) | 1.22(0.44-3.10) |
| 251-350 | 18(26.09) | 20(24.39) | 0.78(0.30-0.99)* | 1.04(0.35-3.10) |
| >350 | 23(33.33) | 19(23.17) | 0.58(0.233-1.44) | 0.82(0.28-2.34 |
Table 8: The association between independents and perception for bivariate and multiple logistic regression analysis
The present study aimed to evaluate the knowledge, attitudes, and perceptions of women regarding caesarean section (CS and its associated factors among pregnant and postpartum women attending maternal health units in burao district, somaliland. Our findings indicate a high level of awareness and varied attitudes towards caesarean section among the participants.
The majority of women in our study (64.81%) demonstrated good knowledge about caesarean sections. This contrasts with findings from a study conducted in Berbera, where 38% of pregnant women had never heard of caesarean section [18]. Our results align with another study in Nigeria [19], which reported that 82.3% of women were aware of caesarean section. Notably, our study found that all participants (100%) were aware that caesarean section can save neonatal lives, which is consistent with findings from Zayed study in Saudi Arabia [20], where 94.2% of mothers recognized the life-saving potential of caesarean section. Furthermore, a substantial proportion of our participants (77.78%) were aware that vaginal delivery is possible after a caesarean section, which is similar to the 94.4% awareness reported in Nigeria [14]. Additionally, 72.84% of participants understood the need for blood before and after the operation, echoing the 86.4% awareness reported by [11].
Regarding attitudes, our study found that 51% of women held a positive attitude towards caesarean section, while 48% had a negative attitude. The majority of women (46.30%) expressed a willingness to undergo a caesarean section if medically indicated, whereas only 4.32% strongly disagreed with this. Interestingly, 75% of women strongly disagreed with the notion that caesarean section is a woman's right and can be chosen at any time without medical indication. Most participants (59.88%) agreed that caesarean section should only be performed when vaginal delivery is not possible, while 8.02% disagreed. These findings are consistent with a qualitative study from Sweden, which highlighted concerns among Somali women about caesarean section, including fears related to female genital mutilation and perceived stigma from healthcare professionals [21].
In terms of perceptions, our study revealed that 55.56% of women had a good perception of caesarean section, while 44.44% held a bad perception. This contrasts with Waniala's study [22], where women favouring vaginal delivery perceived caesarean section as dangerous, whereas those favouring caesarean section perceived it as safer than vaginal delivery. This discrepancy highlights the diverse views on caesarean section and underscores the need for tailored educational interventions to address specific concerns and misconceptions.
This study indicates that pregnant and postpartum women generally possess good knowledge (64.81%), a positive attitude (51.85%), and a favorable perception (55.56%) towards caesarean delivery. Despite this positive outlook, the observed rates of caesarean sections are notably high, with 25.81% of first deliveries and 30.0% of recent deliveries conducted via caesarean section. Additionally, elective caesarean sections account for 5.45% of all cases. This disproportionately high rate of caesarean deliveries may be influenced by factors related to healthcare professionals' practices and decision-making processes. These findings suggest that while women are well-informed and generally positive about caesarean sections, the high incidence of such procedures indicates a need to examine the clinical practices and guidelines followed by healthcare providers.
Based on the research findings, it is recommended that maternal health programs prioritize education and awareness campaigns tailored to different delivery experiences. Efforts should be made to provide comprehensive information about caesarean sections to expectant mothers, especially those with varied personal delivery experiences. Additionally, targeted interventions should address socio-economic disparities, ensuring that all mothers, regardless of income level, have access to accurate information and support regarding delivery options. Furthermore, educational initiatives should be strengthened to enhance mothers' understanding of caesarean sections, as higher education levels were associated with more informed and favorable perceptions. By addressing these factors, maternal health programs can better support informed decision-making and positive attitudes towards cesarean sections.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Hussein KM, Mahamed AA, Mahamed KA (2024). Knowledge, Attitude and Perception towards Caesarean Section and Its Associated Factors Among Pregnant and Postpartum women Attending Maternal Health Units in Burao District, Somaliland. J Women's Health Care. 13(8):740
Received: 25-Jul-2024, Manuscript No. 33184; Editor assigned: 27-Jul-2024, Pre QC No. 33184; Reviewed: 08-Aug-2024, QC No. 33184; Revised: 17-Aug-2024, Manuscript No. 33184; Published: 21-Aug-2024 , DOI: 10.35248/2167- 0420.24.13. 740
Copyright: © 2024 Hussein KM, Mahamed AA, Mahamed KA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited