Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Review Article - (2019)Volume 8, Issue 4
Introduction: Before the advancement and improvement of techniques of using laparoscopy in total hysterectomy, it was considered as a procedure that carried a high risk of injury to the ureters but now with improvement of the experience, training and novel equipment, there is increase in the use of such procedure with lower incidence of ureteric injury. Recently, in surgical staging of endometrial carcinoma (EC); the laparoscopy role has been considered more beneficial. Many previous reports proved fewer complications, lower morbidity, shorter duration of postoperative hospitalization, and rabid recovery. But, the therapeutic benefits and drawbacks of using laparoscopy are not confirmed yet.
Aim: The aim of current study was to assess the benefits and drawbacks of using laparoscopy in surgical staging of EC and comparing them with open surgical staging (laparotomy).
Materials and Methods: the current study included 50 patients diagnosed with EC were included and were divided in to two groups the first group included 20 patients and was managed by laparoscopic staging, while the second group included 30 patients and was managed by laparotomy. We compared between using laparoscopy in surgical staging of EC with open surgical staging (laparotomy) regarding operative and postoperative outcomes.
Results: laparoscopic method of staging had a significantly longer time of the operation than laparotomy (p=0.04), but it had lesser amount of blood loss intra-operatively (p<0.002). There were fewer number of resected lymph nodes (p=0.004) in the laparoscopic technique in contrast to laparotomy. Patients who underwent laparoscopy has a shorter time of postoperative staying in hospital in comparison to those who underwent laparotomy (p=0.012). More number of patients in the open group than the laparoscopy group underwent para-aortic lymphadenectomy (p<0.001).
Conclusion: we have proved the benefits, disadvantages and the essential role of laparoscopy in treatment and surgical staging of EC. Laparoscopy is proved to be safe and effective technique with lower rates of blood loss and less rates of intra-and post-operative morbidity. Experienced surgeon could perform hysterectomy and lymphadenectomy with perfect cancer excision and staging as equally good to laparotomy.
Laparoscopic; Laparotomy; Surgical staging; Endometrial carcinoma
Endometrial carcinoma (EC) has been ranked as the 4th commonest female cancer worldwide and the commonest cancer that affect postmenopausal women [1]. Surgery is considered the standard treatment for EC according to the International Federation of Obstetrics and Gynecology (FIGO) staging system [2]. The conventional staging surgery procedures include performing peritoneal washings cytology, total abdominal hysterectomy (TAH), bilateral salpingo-oophorectomy (BSO), pelvic and/or para-aortic lymphadenectomy. Before the advancement and improvement of techniques of using laparoscopy in total hysterectomy, it was considered as a procedure that carried a high risk of injury of the ureters but now with improvement of the experience, training and novel equipment there is increase in the use of such procedure with lower incidence of ureteric injury [1] Recently, in surgical staging of EC; the role of laparoscopy has become more important. Many previous reports proved fewer complications, lower morbidity, shorter duration of post-operative hospitalization, and rabid recovery [3-5]. But, the therapeutic benefits and drawbacks of using laparoscopy are not confirmed yet. There is a gap of knowledge between results of previous studies.
The aim of our study was to evaluate the benefits and drawbacks of using laparoscopy in surgical staging of EC and comparing them with open surgical staging (laparotomy).
This is a retrospective cohort study which was designed to compare using laparoscopy in surgical staging of EC with open surgical staging (laparotomy).
Our study was performed in Department of Gynecology and Obstetrics and in Department of General Surgery, Faculty of Medicine, Zagazig University. The approval of local ethical committee of Faculty of Medicine Zagazig University was obtained. A total of 50 patients diagnosed with EC were included for a period from January, 2016 to March 2019. All selected patients were divided in to two groups the first group included 20 patients and was managed by laparoscopic staging, while the second group included 30 patients and was managed by laparotomy. Written informed consents were acquired from all patients for all surgeries.
We reviewed the data recorded for all included EC patients in our study. Inclusion criteria (1) sure histo-pathological diagnosis of EC (2) size of the tumor is less than 2 cm without presence of lymph node enlargement on radiological evaluation by magnetic resonance imaging (3) the tumor is clinically confined to the body of the uterus.
All the included cases were subjected to surgical staging which is consisting of TAH & BSO, pelvic lymphadenectomy and/or paraaortic lymphadenectomy.
The appropriate details of surgical techniques are:
• TAH & BSO, pelvic lymphadenectomy and para-aortic lymphadenectomy was performed using a single-port device in two steps: First, a retroperitoneal para-aortic dissection was conducted, followed by a trans peritoneal pelvic lymphadenectomy and a total hysterectomy. Conventional laparoscopic instruments were used in the selected cases.
• Pelvic lymphadenectomy is the surgical excision of lymph nodes from the obturator fossa, above the level of obturator nerve and those which are found over external iliac vessels.
• Para-aortic lymphadenectomy is the surgical excision of lymph nodes which are found over the inferior vena cava and the abdominal aorta, below inferior mesenteric artery.
Pre-operative data were collected from patients’ files (age and parity), body mass index (BMI), and history of previous abdominal operations. Operative and post-operative data were recorded and analyzed; pain, bleeding, operative time, amount of blood loss, and length of hospital stay, and number of excised lymph nodes. Postoperative histopathological data were detected by examinations of the postoperative excised samples in pathology department, Faculty of Medicine, Zagazig University grade, and surgical stage of cancer (as defined by FIGO, 2009), LV invasion and the depth of invasion of the myometrium,. All data were collected tabulated and statistically analyzed using Microsoft Excel 2010. And the tests used were; Chi-square, Fisher’s exact test, t-test and Mann-Whitney U-test.
In group of patients which are managed by laparoscopy (20 patients), all of them were completed laparoscopically without conversion to laparotomy. And the remaining 30 patients were surgically managed by open laparotomy from the start. Pelvic lymphadenectomy was performed for all the included 50 patients. While, we performed para-aortic lymphadenectomy in one patient from the first group which is managed by laparoscopy and in 3 patients who were surgically managed by laparotomy.
The findings in the two study groups’ are detailed in Table 1.
| Variables | Staging by laparoscopy no (20) | Staging by laparotomy no (30) | P-value |
|---|---|---|---|
| Patient age (y) | 56.3 (29e80) | 55.4 (28e75) | 0.148 |
| Gestation | 2.65 (0e8) | 2.94 (0e8) | 0.207 |
| Parity | 2.09 (0e7) | 2.14 (0e5) | 0.207 |
| Body mass index (kg/m2) | 28.0 (16e38) | 25.4 (13e44) | 0.254 |
| Previous abdominal surgery | 5 (25%) | 6 (20) | 0.974 |
Table 1: Demographic data of patients.
There were no significant differences between the both groups regarding patients’ age, BMI, number of previous surgeries with abdominal incisions, histological grade of EC or FIGO stage.
Table 2 shows the correlations between intraoperative data of both groups. Although laparoscopic method of staging had a significantly longer time of the operation than laparotomy (p=0.04), but it had less intraoperative blood loss (p<0.001). Two patients which are operated by laparotomy had a blood loss more than 500 mL and required blood transfusion. No patients in the laparoscopic group were in need for blood transfusion.
| Variables | Staging by laparoscopy no(20) | Staging by laparotomy no(30) | P-value |
|---|---|---|---|
| Blood loss (mL) intra-operatively | 73(30e300) | 280 (50e1500) | <0.001 |
| Operative time (min) | 160 (81e275) | 130 (80e190) | 0.04 |
| Uterine weight (g) | 186.8 (55e405) | 287.5 (40e1360) | 0.003 |
| No. of pelvic lymph nodes | 15 (2e58) | 20 (4e50) | 0.004 |
| Hospital stays (d) | 6 (3e11) | 11 (5e28) | 0.012 |
| Intra- and postoperative complications | 2(10) | 6 (20) | 0.068 |
| Wound infection | 0 (0) | 2 (2.4) | |
| Vaginitis | 1 (5.7) | 1 (1.2) | |
| Urinary tract infection | 1 (1.4) | 1 (1.2) | |
| Ileus | 0 (0) | 2 (1.2) |
Table 2: Intra-operative parameters and postoperative complications.
There were fewer number of resected lymph nodes (p=0.004) with the laparoscopic technique as in contrast to laparotomy. Patients who underwent laparoscopy had a smaller time of post-operative staying in hospital in comparison to those who underwent laparotomy (p=0.012). There was no significant difference between both groups regarding complication rate between. No injuries to the bowel or vascular complications were reported during the laparoscopic staging method.
Table 3 shows both groups, most patients had Stage 1 and Grade 1 EC with invasion into less than half of the myometrium (Figure 1).
| Variables | Staging by laparoscopy no(20) % | Staging by laparotomy no(30) % | P-value |
|---|---|---|---|
| Grade | |||
| 1 | 15(75) | 18 (75) | 0.166 |
| 2 | 3 (15) | 9 (15) | |
| 3 | 2 (10) | 3 (10) | |
| Stage | |||
| 1 | 18 (90) | 24 (86) | 0.123 |
| 2 | 1 (5) | 3 (7) | |
| 3 | 1 (5) | 3 (7) | |
| Myometrial Invasion | |||
| No | 5 (25) | 6 (20) | 0.923 |
| 1/2 thickness | 13 (65) | 23 (70) | |
| >1/2 thickness | 2 (10) | 3 (10) | |
| LVSI | |||
| No | 15 (75) | 19(60) | 0.947 |
| Yes | 5 (25) | 11 (40) | |
| Lymph Node Metastasis | |||
| No | 18 (90) | 24 (86) | 0.213 |
| Yes | 2 (10) | 6 (14) | |
Table 3: Oncological and histopathological parameters of the included cases by surgical approach.
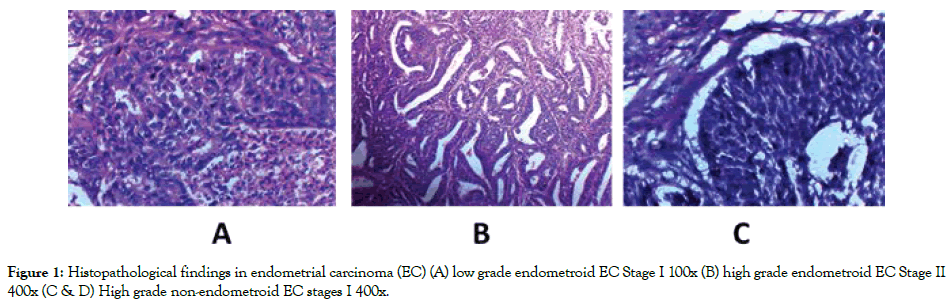
Figure 1. Histopathological findings in endometrial carcinoma (EC) (A) low grade endometroid EC Stage I 100x (B) high grade endometroid EC Stage II 400x (C & D) High grade non-endometroid EC stages I 400x.
More number of patients in the open group than the laparoscopy group underwent para-aortic lymphadenectomy (p<0.001).
Adequate EC staging, which is based on the latest FIGO staging, has an essential role in choosing the adequate type of its management. Recently most surgeons choose the laparoscopic approach for surgical staging of early EC mainly stages I & II where the tumor is confined to the uterus and cervix [1]. Recently most gynecologists encourage performing lymphadenectomy in most diagnosed EC patients and some of them prefer laparotomy which allow a direct tactile approach during the dissection of lymph node.
In our current study we have demonstrated that the laparoscopic surgical management and staging of EC in addition to lymphadenectomy is a feasible, effective and safe method, similarly by Chu et al. [2]. The study of Ghazali et al. [1], showed the values of laparoscopic excision in EC stage I with proved histopathological results and proved that laparoscopy technique is not worsened or decreased the completeness of tumor excision with adequate margins. And they found that full hysterectomy could be performed similar to laparotomy technique. Ghazali et al. [1] study shows that lymphadenectomy could be performed safely and completely during laparoscopy and the number of lymph nodes is similar to laparotomy, which was nearly similar to our results. Moreover Ghazali et al. [1] proved that laparoscopy is a safe approach for patients of alla age groups even with presence of comorbid conditions as obesity, hypertension or diabetes. In the surgical management of any malignancy the most important issue is to keep the patient as healthy as the surgeon can. So any performed procedure must aim at decreasing patients’ morbidity. The most morbid condition of the patient results from excessive intra and/or post-operative bleeding, wound infection, difficult post-operative movement. These morbidities will weaken their body more and couldn’t fight the cancer. Using the laparoscopic approach of management allow rabid healing of the wound which allow rabid beginning of needed further therapies for EC e.g. chemotherapy or radiotherapy which improve patients outcome and survival.
Similarly Api, et al. [6] comparison study, between laparoscopy and laparotomy and finally favoured laparoscopy technique regarding lesser blood loss and shorter time of post-operative hospital stay.
Moreover it was found that was no increased 3 years recurrence rate in the patients who underwent laparoscopic management versus those who underwent laparotomy management, and the 5-year OS rate was the same in both groups [7]. Our results are in line with previous reported results that laparoscopy is a safe and effective method os surgical management and staging of EC. Also we showed that intraoperative blood loss was lower in those patients who underwent laparoscopy versus those who underwent laparotomy. There are no patients have required blood transfusion intra- or post-operative in the laparoscopy groups. But we found that the time of operation was longer in the laparoscopy than for laparotomy, these findings are near findings from previous studies [2,7, and 4]. We found that there is no patient in the laparoscopy group was converted to laparotomy that is comparable with previously reported conversion rates of 0-36.4% [8-11].
Our study encouraged performing laparoscopy especially in obese patients or patients that are at high risk of developing deep vein thrombosis or pulmonary embolism due to smaller size of the incision, less painful technique which allowed rabid post-operative movement. However, there are some morbid patients conditions that lead to extra caution before choosing laparoscopic surgery e.g. patients with chronic lung disease that leads to restricted lung function or patients with morbid obesity and obstructive sleep apnea. So, a medical physician or ear, nose, and throat (ENT) specialist evaluation is required before deciding the type of surgery. The reason for such extra caution that during the laparoscopic approach, the anesthetists might have intra-operative difficulties in adequate patients ventilation due to insufflation of the abdomen, with higher rate of conversion to laparotomy due to difficult laparoscopic techniques, poor visualization and difficulties in instruments manipulation [1].
Performing laparoscopic surgical staging of EC is now performed routinely in many centres and the availability of recent instruments, the skill and experience of surgeons play an essential role in controlling the operative time. Our current study proved the essential role of laparoscopy in management and surgical staging of EC. Laparoscopy is proved to be safe and effective technique with lower rates of blood loss and less rates of intra- and post-operative morbidity. Experienced surgeon could perform hysterectomy and lymphadenectomy with perfect cancer excision and staging as equally good to laparotomy.
Few numbers of the included cases and absence of long term follow-up which is needed to assess the patients’ outcome.
Our study is deficient in long time of patients’ follow-up to evaluate differences in survival and postoperative recurrence in both techniques and the long-term follow-up and survival data may need more patients and larger time of follow-up to allow more accurate evaluation.
Citation: Ramadan MSH, Eltokhy EA, Yehia AM, Mahmoud R, Harb OA (2019) Laparoscopic Versus Conventional Open Method for the Surgical Staging of Endometrial Carcinoma: A Comparative Study. J Women’s Health Care 8.469. doi: 10.35248/2167-0420.19.8.469.
Received: 13-May-2019 Accepted: 30-May-2019 Published: 07-Jun-2019
Copyright: © 2019 Ramadan MSH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.