Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2021)Volume 12, Issue 2
A 62-years-old man who underwent cataract surgery coupled with intraocular lens implantation with the Yamane 2-haptic intrascleral fixation technique (ISF IOL) due to a history of blunt ocular trauma, was referred to our department due to pain and vision loss, 8 weeks after his operation. The patient presented visual acuity of light perception of the right eye, conjunctival hyperemia, hypopyon, vitritis, and 2 exposed PMMA flanges throughout the conjunctiva.
Endophthalmitis was diagnosed, followed by urgent treatment with vitreous and anterior chamber puncture and intravitreal injections of antibiotics and steroids. The cultures revealed Staphylococcus epidermidis infection which was resolved in a few weeks; with notable improvement in final visual acuity.
The SF IOL with 2 monoflex PMMA flanges has gained popularity in the last ten years; a rare complication is the extrusion of the rim that can cause endophthalmitis as in this case. Studies evaluating the short- and long-term complications of this technique are warranted.
Endophthalmitis; Cataract surgery; Intrascleral fixation technique; Staphylococcus epidermidis; Intraocular lens
Scharioth et al. described a technique to fix the haptics of a 3-piece lens within a scleral tunnel without the need for sutures [1]; Yamane et al. described the intra-SF IOL (ISF IOL) technique with haptic flange [2,3] and in 2019, Canabrava et al. presented a new sutureless 4-flange ISF IOL technique using a 5-0 polypropylene suture and a 1-piece poly (methyl methacrylate) IOL with eyelets in the haptics [2,4]. One of the complications that may arise for these techniques is infectious endophthalmitis, a condition in which the internal structures of the eye are infected by microorganisms such as bacteria [5,6].
A 62-year-old man was referred to our hospital due to pain, redness, and reduced visual acuity in his right eye over the 7 days prior to the consultation. The patient did not had a personal history of pathologies; initial best corrected visual acuity (BCVA) 20/100 in the right eye due to blunt ocular trauma with lens subluxation, for which a lensectomy plus posterior vitrectomy was performed followed by implantation of 2-haptic ISF IOL without suture “Yamane technique” (Figure 1) and 20/20 in the left eye. 8 weeks after the operation, he presented symptoms of eye pain and reduced vision, for which he was treated (in a private practice) with prednisolone acetate 1% eye drops, suspension; during the follow-up visit 24 hours later, endophthalmitis was diagnosed. In the examination in our department, (BCVA) was perception with light and 20/20 in his right and left eyes, respectively. The intraocular pressure (IOP) was 12 mmHg and 17 mmHg in the right and left eyes, respectively. Biomicroscopic examination of the right eye revealed: severe conjunctival hyperemia, one conjunctival-covered PMMA flange on the nasal side and one transconjunctival exposed PMMA flange on the temporal side, severe corneal edema with Descemet folds 4+, presence of cells at the anterior chamber with 3.0 mm hypopyon and white membrane covering the pupil (Figure 2). The posterior segment wasn’t visible; Ultrasound revealed a homogeneous hyperechoic infiltrate in the anterior vitreous, choroidal thickening, mild T sign. No retinal detachments or choroids were observed (Figure 2).
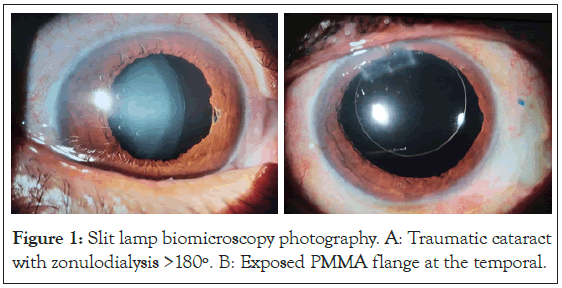
Figure 1: Slit lamp biomicroscopy photography. A: Traumatic cataract with zonulodialysis >180º. B: Exposed PMMA flange at the temporal.
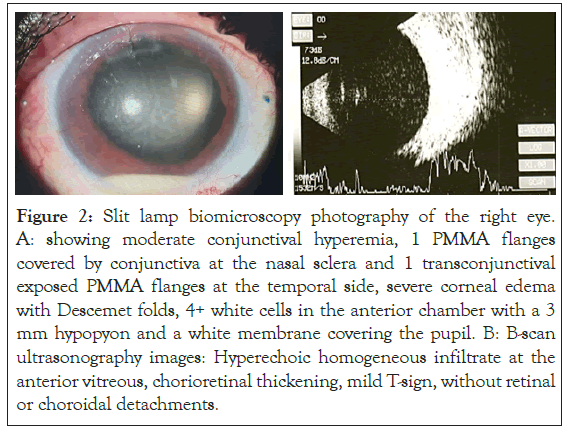
Figure 2: Slit lamp biomicroscopy photography of the right eye. A: showing moderate conjunctival hyperemia, 1 PMMA flanges covered by conjunctiva at the nasal sclera and 1 transconjunctival exposed PMMA flanges at the temporal side, severe corneal edema with Descemet folds, 4+ white cells in the anterior chamber with a 3 mm hypopyon and a white membrane covering the pupil. B: B-scan ultrasonography images: Hyperechoic homogeneous infiltrate at the anterior vitreous, chorioretinal thickening, mild T-sign, without retinal or choroidal detachments.
Once the diagnosis was confirmed, the patient was subjected to an anterior chamber and vitreous biopsy, followed by intravitreal injections of vancomycin (1 mg/0.1 mL), ceftazidime (2.25 mg/0.1 mL) and dexamethasone (400 μg/0.1 ml). The anterior chamber and vitreous samples were sent for Gram staining, culture and antibiotic sensitivity tests; blood cultures were also taken. Although the professional suggestion was for IOL explantation and pars plana vitrectomy, the patient refused any surgical intervention. An intravenous bolus of 1 gram of ceftriaxone was administered per day along with the following regimen of topical medications: dexamethasone 0.1% six times a day, gatifloxacin 0.3% eight times a day and cyclopentolate 1% three times a day. Two days after the procedure, the pain diminished significantly and the inflammation signs began to subside; nevertheless, the intravitreal injection with vancomycin (1 mg/0.1 mL), ceftazidime (2.25 mg/0.1 mL) and dexamethasone (400 μg/0.1 mL) was repeated; with a negative outcome as shown by the vitreous puncture and anterior chamber results. On the fifth day after the initial intravitreal injections, anterior chamber microbiological cultures revealed Staphylococcus epidermidis sensitive to ceftazidime; blood cultures were negative. The patient was discharged with topical drops of gatifloxacin 0.3% and dexamethasone 0.1% six times a day.
During the follow-up visit, 37 days after the last intervention, visual acuity was 20/50 in the right eye due to an epiretinal membrane; without signs of infection, leaving a paralytic mydriasis and an iris pigment adhered to the IOL (Figure 3). At the 2-month follow-up, the eye remained stable and the temporal edges of the IOL still extruded.
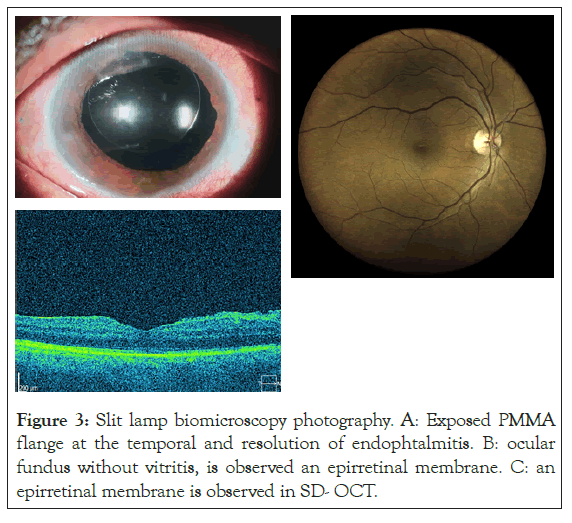
Figure 3: Slit lamp biomicroscopy photography. A: Exposed PMMA flange at the temporal and resolution of endophtalmitis. B: ocular fundus without vitritis, is observed an epirretinal membrane. C: an epirretinal membrane is observed in SD- OCT.
Lalwani et al. reported that the incidence of postoperative endophthalmitis show a decreasing trend, with a frequency of 0.68% to 0.05% after clear corneal cataract extraction surgery in a population with a mean age of 76 years in a period from nine years, due to innovations of the surgical techniques and technological improvements [5].
According to Doft et al. the incidence of postoperative endophthalmitis was 0.072% after cataract extraction with or without IOL implantation, 0.30% after secondary IOL implantation and 0.051% after of PPV [6]. It has also been reported that the incidence of endophthalmitis increases after secondary IOL implantation, probably due to associated risk factors like diabetes mellitus type 1 or 2 [7]; transscleral fixation of the posterior chamber IOL with suture, which provides a pathway from the haptic (internally) to the scleral surface (externally) constituting a gateway for microorganisms, polypropylene haptics of the intraocular lens, preoperative palpebral anomalies, re-entry through an anterior wound and postoperative wound defects [8].
Of all causes the exogenous endophthalmitis, according to published studies have shown that endophthalmitis caused by coagulase-negative staphylococci is associated with the best visual prognosis [9]. The good visual result in our patient may be due, at least in part, to the clinical association with endophthalmitis caused by a low virulence organism.
Worth to mention, for this case, is that the source of the infection was the lens haptic exposure that allowed Staphylococcus epidermidis to penetrate the eye. Exposure of the IOL flang, should be cauterized or covered with the conjunctival flap to prevent any possible infection [9].
The patient’s initial visual acuity was limited to light perception. The Endophthalmitis Vitrectomy Study (EVS) has shown that vitrectomy was beneficial for eyes that presented light perception vision, however, the patient refused any surgical intervention, therefore the treatment was several injections were performed of intravitreal antibiotics [8,10].
In the current case, a good visual outcome with a best-corrected visual acuity of 20/50 at 8 weeks due to the development of an epiretinal membrane. Clinicians must be aware of the high importance of burying the flanges into a short scleral tunnel and the potential risk for endophthalmitis with exposed PMMA flanges.
No relevant potential conflict of interest was reported for this article.
The patient was fully informed about the examinations and provided her written consent. Written consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor.
Citation: Cayatopa FS, Mendez ALG, Ortiz RB, Cueva SAS (2021) Late Endophthalmitis Associated with Haptic Exposure After an Intrascleral Fixation Yamane Technique. J Clin Exp Ophthalmol. 12:874.
Received: 10-Mar-2021 Accepted: 25-Mar-2021 Published: 05-Apr-2021
Copyright: © 2021 Cayatopa FS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.