Review Article - (2022)Volume 8, Issue 4
Lessons Learned from the SARS-CoV-2 Pandemic: Preparing for the Next Outbreak of Respiratory and Enteric Viral Infections
M. Khalid Ijaz1*, Raymond W. Nims2, Joseph R. Rubino1, Julie McKinney1 and Charles P. GerbaAbstract
Evidence has been accumulating to suggest that the numbers of cases/detections of respiratory viruses (especially influenza virus, respiratory syncytial virus, parainfluenza virus, and human metapneumovirus) and enteroviruses (especially norovirus and enterovirus) have dropped drastically during periods of relatively strict adherence to Non- Pharmaceutical Interventions (NPIs) for mitigating the risk of acquiring SARS-CoV-2. In other words, while the public has been protecting themselves from acquiring SARS-CoV-2 through use of NPIs, such as social distancing, mask wearing, avoiding crowded spaces, and paying greater attention to surface and hand hygiene, they may also have been protecting themselves from acquiring other respiratory viruses and enteric pathogens, including viral infections. What evidence do we have of this? What may happen when the NPIs are relaxed in the post-pandemic setting? In this viewpoint, we discuss these topics and other learnings from the ongoing SARS-CoV-2/COVID-19 pandemic, as well as our recommendations for NPIs for preparing for the inevitable post-pandemic future.
Keywords
COVID-19; SARS-CoV-2; Non-pharmaceutical interventions; Enteroviral infections; Respiratory infections; Post-pandemic viral outbreaks
Introduction
The pandemic of severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2) and its associated disease (COVID-19) has caused considerable morbidity and mortality worldwide, with cases numbering ~507 million and deaths numbering just over 6 million globally, as of the date of writing of this article [1]. In addition, the pandemic has had severe economic consequences globally [2]. As the SARS-CoV-2 pandemic extended into its second year in 2021, the public-at-large and local governments had at various times and to varying extent, observed voluntary and imposed Non-Pharmaceutical Interventions (NPIs) including mask wearing, social distancing, stay-at-home/lockdowns, bans on indoor and outdoor social gatherings, travel restrictions, and increased frequency/stringency of surface and hand hygiene. Air sanitization practices, including use of room air purifiers and use of High Efficiency Particulate Air (HEPA) filters, used in conjunction with the other best practices recommended by the U.S. Centers for Disease Prevention and Control (CDC) and other regional public health agencies, also likely contributed to mitigation of transmission risk during this pandemic [3,4]. In various locations around the globe, relaxation of these NPIs to varying degrees has been occurring, and the resumption of high-risk activities such as participation in social events taking place in crowded venues (e.g., concert halls, bars, sports venues, etc.) has occurred during 2021 and into 2022. In some cases, relaxation of NPIs has been associated with rebounds in SARS-CoV-2 caseloads, and in detection rates for other respiratory and enteric viruses, as will be discussed below.
Should this have been expected? In fact, such rebounds have been associated with past pandemics. For instance, the third season of the 1918 “Spanish” influenza pandemic represented a similar situation. In the United States, as Infection Prevention And Control (IPAC) measures yielded to public fatigue, case numbers and death rates rebounded. As documented by McHugh [5]. “The 1918 flu lasted far beyond 1918. Two years after it began, just as officials were declaring victory and cities were easing restrictions, a fourth wave hit parts of the country, bringing punishing caseloads that pushed some hospitals to the brink of collapse and left many more Americans dead. By the winter of 1919-1920, Americans were weary of the limitations on daily life. Nearly all of the public health restrictions -such as mask-wearing, social distancing and the closure of schools and churches-had been lifted. A hasty return to public gatherings led to an increase in case numbers. Politicians either blamed people’s carelessness for the reemergence of the virus or downplayed the seriousness of it.” [5,6-8].
To what extent are we now repeating history? Have the various NPIs implemented during the SARS-CoV-2 pandemic really led to a decrease in caseloads and morbidity for SARS-CoV-2 during 2020 and early 2021? Following relaxation of interventions, have caseloads for SARS-CoV-2 increased? Have caseloads and detection rates for other communicable respiratory and enteric viruses diminished during the observance of NPIs for SARS-CoV-2? What is to be expected for these other respiratory or enteric viruses once NPIs for SARS-CoV-2 are more uniformly relaxed going into 2022? In this mini-review, we have attempted to answer these questions and to use these learnings to put into perspective the most appropriate roles of NPIs at home, community, and health care settings in the post-pandemic future.
A quite extensive body of literature addressing the impact, on SARSCoV- 2/COVID-19 transmission, of implementation of NPIs has appeared during the SARS-CoV-2 pandemic. In this mini-review, we have included in Table 1 just a sampling of this literature. Although a full review on this topic is beyond the scope of the present mini-review, we have attempted in Table 2. to more comprehensively review the literature on the impact of NPIs implemented in response to SARS-CoV-2 on the detection of other seasonal respiratory and enteric viruses, and the resurgence of detections of these viruses following relaxation of the pandemic-driven NPIs. Finally, in Table 3, we provide our recommendations for the role of NPIs in the postpandemic future in responding to emerging and re-emerging respiratory and enteric viruses.
| Intervention | Impact on SARS-CoV-2 transmission measures | Reference |
|---|---|---|
| Impact of observation of non-pharmaceutical interventions | ||
| Travel restrictions, school closures, social distancing, closure of non-essential businesses in Ontario, Canada | Modeling of SARS-CoV-2 reproduction number Rc indicated Rc was 2.84 to 3.25 between Feb. 26 to Mar. 21 - 29, 2020. Improving case detection rates and reducing contacts was estimated to lead to Rc less than the threshold 1 value in Apr. 2020. Key factors in reducing Rc were found to be reducing contact rate, transmission probability, detection/diagnosis rate, and quarantine rate. Transmission probability is impacted by personal hygiene (handwashing and avoiding face touching) and mask wearing. | [9] |
| Ban on large gatherings, shelter-in-place, public school closures, restaurant or entertainment business closures in USA | Impacts of interventions on growth rates for SARS-CoV-2 cases were evaluated. After 21 days of implementation, the most significant reductions in growth rate were due to shelter-in-place orders (-8.6%) and restaurant or entertainment business closures (-5.2%). School closures and bans on large gatherings did not result in significant impacts of case growth rates. | [10] |
| School closures, non-essential business closures, ban on public events/gatherings, encouraged or imposed work at home in Texas, USA | School closures alone resulted in minimal reductions in cumulative or peak SARS-CoV-2 caseloads, hospitalizations, and deaths from Mar. to Aug. 2020. On the other hand, school closures plus 75% to 90% reduction in non-household contacts resulted in striking reductions in both cumulative and peak caseloads, hospitalizations, and deaths, compared to no measures. | [11] |
| School closures, voluntary stay-at-home, state ordered shelter-in-place in Georgia, USA | Compared to no interventions, or to school closure only, voluntary stay at home and state ordered shelter-in-place resulted in 25-36% fewer infections from Mar. 2020 to Oct. 2020. Extending the length of the intervention period reduced the new infection counts and delayed the peak infection rates, as well as the cumulative numbers of cases and deaths | [12] |
| Travel ban, state border closures, working from home, limits on indoor and outdoor social gatherings, increased use of hand hygiene, face mask wearing, in Australia | COVID-19 detections declined sharply following implementation of the most stringent government restrictions by the end of Mar. 2020. | [13] |
| School closures, workplace closures, public events bans, stay at home orders, within country travel bans; date pooled from 131 countries | A decreasing trend in the time-varying reproduction number (R) ratio (R for current phase of restrictions/R for previous phase of restrictions) following NPI implementation. Statistically significant decreases were noted only for bans on public events. | [14] |
| Personal protective measures (mask wearing, hand washing, physical distancing, in Thailand | Consistent mask wearing, handwashing, and social distancing were independently associated with lower risk for SARS-CoV-2 infection. | [15] |
| Social distancing in Oregon, USA | Modeling based on mobile phone location demonstrated that social distancing is extremely effective in reducing both the cumulative impact (in terms of fraction infected) and the peak intensity of the epidemic. | [16] |
| Personal protective measures (mask wearing, hand washing, physical distancing, in Macao, China | Statistically significant COVID-19 infection risk reductions in those wearing face masks when outside of the home, and in those who wash hands following high risk activities (food handling, following use of toilet, sneezing and coughing, handling pets), and before touching mouth and nose). | [17] |
| School closures, gatherings bans, business closures, stay-at-home orders, wearing of face masks, and travel restrictions in the USA | Stay-at-home orders resulted in the greatest decreases (51% reduction) in reproduction number (Rt), followed by mask wearing (29%), bans on large (7%) and small (19%) social gatherings, and non-essential business closures (16%). | [18] |
| Mask use, disinfection, and social distancing in Beijing, China | Face mask use by the primary case and family contacts before the primary case developed symptoms was 79% effective in reducing transmission. Daily use of chlorine- or ethanol-based disinfectant in households was 77% effective. Wearing a mask after symptom onset of the primary case was not significantly protective. | [19] |
| Impact of relaxation of non-pharmaceutical interventions | ||
| Relaxation of school closures, workplace closures, public events bans, stay at home orders, within country travel bans; data from 131 countries | An increasing trend over time in the R ratio was observed following relaxation of NPI. Statistically significant increases were noted only for school reopening and lifting bans on public events. | [14] |
| Physical, but not travel, restrictions were relaxed from May to June 2020 in Australia | A peak in COVID-19 notifications occurred in July 2020 following relaxation of certain NPI. | [13] |
| Relaxation of stay-at-home orders in USA | COVID-19 prevalence was 12.4 cases per 100,000 population during implementation of stay-at-home orders, vs. 234.6 cases per 100,000 population following relaxation of stay-at-home orders. | [28] |
Table 1: Impact of SARS-CoV-2 case numbers/deaths following observation and relaxation of non-pharmaceutical interventions.
| Intervention | Impact on respiratory/enteric viral transmission measures | Reference |
|---|---|---|
| Impact of observation of non-pharmaceutical interventions | ||
| Social distancing, lockdown in Finland | Statistically significant decrease in rate of daily pediatric ER visits, shortened influenza and RSV seasons, relative to previous four seasons | [38] |
| Travel ban, state border closures, working from home, limits on indoor and outdoor social gatherings, increased use of hand hygiene, face mask wearing, in Australia | Influenza notifications numbered 7,029 from Mar. to Sep. 2020, compared to an average of 149,832 for the same period in 2015-2019. During Mar. to Sep. 2020, detections of RSV and influenza virus remained extremely low. Rhinovirus detections also declined in Apr. 2020, following implementation of the most stringent restrictions | [13] |
| Isolation of confirmed/suspected COVID-19 cases, strict community restrictions, travel bans, school and entertainment venue closures, bans on mass gatherings, compulsory use of face masks, in China | Following implementation of NPIs, the positivity rate for influenza virus detections was reduced by 79%, compared with the two previous epidemiological years (1 Oct. to 30 Sept.). The influenza virus positivity rate approached zero within 7 weeks of NPI implementation. Influenza incidence and reproduction number (Rt) also declined significantly during these periods. | [39] |
| Community lockdown in Wuhan, China and Government declaration of a state of emergency in USA | NPIs intended to mitigate SARS-CoV-2 transmission reduced influenza positivity rates in Southern China, Northern China, and the USA during the 2019-2020 influenza seasons by 79%, 79%, and 67%, respectively, compared with modeling based on the rates from previous influenza seasons. | [40] |
| Social distancing: foreign travel ban, gathering bans, public closures, stay at home orders in USA | Decreased detection rates for influenza virus A, hERV, MPV, and PIV in Mar. and Apr. 2020, compared to historical rates for the previous five years | [41] |
| Social distancing, including school closures, travel restrictions, non-essential business closures, and ban of social gatherings in Alaska, USA | Hospital admissions for acute respiratory illnesses and specifically for RSV in children decreased to zero by the second week of Apr. 2020 and remained there through the third week in May. During the previous ten seasons, ~23% of admissions occurred between Mar. 28 and 15 May, vs. only 3.6% of admissions during this period in the 2019-2020 season. | [42] |
| International and state border closures, stay-at-home restrictions in Western Australia | 98.0% and 99.4% reductions in RSV and influenza virus detections in children through winter 2020 in Western Australia, compared with typical seasons (2012-2019). Decreased detection despite school reopening while observing social distancing and increased hygiene | [43] |
| International and state border closures, stay-at-home restrictions, limiting social gatherings, increased hand hygiene in Queensland, Australia | Striking reduction in detection of influenza virus, MPV, PIV, RSV in 2020 vs. 2019. Reduction of Ad and rhinovirus was only observed during national lockdown period. | [44] |
| School closures, ban on public gatherings, non-essential business closures in Alberta, Canada | Respiratory virus surveillance data from Mar. to Jul. 2020 indicated significant reductions in test positivity rates for influenza virus A/B, RSV, MPV, hERV, and PIV, compared to similar time periods in 2017- 2019. | [45] |
| Social distancing, travel restrictions, face mask mandates, lockdowns, school closures, and increased hand hygiene in Canada | Significantly decreased detection of influenza virus A/B, RSV, PIV, and MPV in 2020-2021, compared to the pre-pandemic period (2014-2019). Lesser, but still statistically significant decreases in detection of Ad, CoV, and hERV were also observed. | [46] |
| NPI Levels 1 (face masks, personal hygiene, social distancing) through 3 (added business, school, event closures) in South Korea | The more stringent the NPI, the higher the reduction in respiratory virus rates, per the national respiratory virus surveillance dataset, compared to 2015-2019. The most striking reductions were for RSV, PIV, influenza virus, CoV, and MPV. Less impacted were Ad and hERV. | [47] |
| Movement restrictions, social distancing, face coverings, increased hand hygiene in UK | 62.2% and 98.8% reduction in positive tests for pediatric viruses (RSV, PIV, influenza virus, enterovirus, Ad) at two large hospitals from Apr. 2020 to Mar. 2021, compared to pre-pandemic period (Apr. 2019 to Mar. 2020) | [48] |
| National lockdown, social distancing, school and daycare closures, use of masks in UK | Detection of RSV, influenza virus, MPV, PIV, and CoV were suppressed in the period of Mar. to Oct. 2020, compared to similar periods in 2016 to 2019. | [49] |
| National lockdown, social distancing, school and daycare closures, use of masks in UK | Decreases in hospital admissions for influenza virus (94%), bronchiolitis (RSV, 82%) from Mar. 2020 to Mar. 2021 compared to Mar. 2017 through Feb. 2020. | [50] |
| Contact ban, mask mandate, school and venue closures in Germany | Decrease in all respiratory viruses per national surveillance system, coinciding with temporary interventions. Influenza virus infections were at historically low levels throughout the 2020-2021 season. | [51] |
| Pre-lockdown, lockdown, universal mask mandate in Singapore | Pre-lockdown measures resulted in decreased cases of influenza and respiratory viruses other than hERV and Ad, for which case numbers were reduced following lockdown, relative to 2019 numbers. | [52] |
| Social distancing, personal hygiene, and universal face mask use in South Korea | Statistically significant reductions in hospitalizations for pneumonia and influenza were observed from Feb. to Jul. 2020, versus 2016-2019. | [53] |
| Social distancing, mask wearing, hand hygiene in Brazil | Among patients hospitalized with respiratory symptoms but negative for SARS-CoV-2, only 1.8% had influenza virus A, none had influenza virus B, 8.6% had Ad, 26% had rhinovirus 1/2, 14% had rhinovirus 2/2, and none had enterovirus 68. In 2019, 17.8% of such patients were positive for influenza virus A. | [54] |
| Social distancing, school and daycare closures, non-essential commerce closures, emphasized hygiene measures and mask wearing in Brazil | 75% to 81% reduction in hospitalizations for acute bronchiolitis (primarily caused by RSV) in children in Mar. through Jun. 2020, compared to similar time periods in 2016-2019. | [55] |
| Ban of social gatherings, mask mandates, work at home, school closures in Shanghai, China | Significant reduction in incidence of RSV, PIV 1/3, Ad, influenza virus A/B, and MPV in children during 2020, compared to 2019. | [56] |
| National lockdown in Italy | Within a month of the national lockdown in Italy, isolations of RSV, hERV, PIV-1,2,3,4, MPV, influenza virus, CoV, and Ad were atypically low, compared to the pre-pandemic period of Jan. to Mar. 2020 and to the comparable time period in 2019. | [36] |
| Voluntary mask wearing, school closure, social distancing, increased hand hygiene, temperature checks, bans on gatherings/events, travel restrictions in Hong Kong | Hospitalizations for children decreased by 85% to 99% in 2019, compared to 2017-2019. This included rates for influenza virus A/B, RSV, Ad, PIV 1-4, MPV, and hERV | [57] |
| Social distancing, school closures, furlough scheme, entertainment and restaurant closures; partial lockdown in England | Compared to the 5-year average (2015-2019), laboratory-confirmed norovirus caseloads for norovirus were similar through week 6, then begin decreasing in the pre-lockdown and early lockdown periods beginning weeks 10-14 and remained very low through week 31. | [37] |
| Impact of relaxation of non-pharmaceutical interventions | ||
| Reopening of schools, opening of non-essential retail and outdoor hospitality, resumption of indoor socialization and hospitality in UK | Increases in rhinovirus detection, detection of PIV and CoV. | [58] |
| Reopening of schools and day-care centers in Germany | Resurgence in rhinovirus detection to pre-pandemic levels, especially in children. | [51] |
| Reopening of businesses and schools but continued mask wearing and social distancing in Singapore | Resurgence in hERV in September, 13 weeks after reopening | [52] |
| Relaxation in social distancing, other local restrictions, normal school activities, and relaxation of state border restrictions in Western Australia | Resurgence in RSV detections in children in Western Australia, exceeding the median seasonal peaks from 2012 to 2019, following relaxation of restrictions in the fall of 2020. | [59] |
| Relaxation in social distancing, other local restrictions, normal school activities, and relaxation of state border restrictions in Queensland, Australia | Resurgence of RSV following termination of lockdowns in Queensland in Dec. 2020. Rhinovirus resurgence to levels higher than observed in 2017-2019 occurred following reopening of schools in late May 2020. | [44] |
| School reopening and relaxation of restrictions of health measures for adults in France | Delayed RSV season in fall of 2020, with increased case detection in children coinciding not with school reopening (maintaining mask wearing) but with relaxation of restrictions for adults (easing of travel restrictions, non-essential business opening, etc.) | [60] |
| Easing of restrictive measures (including mask wearing and social distancing) in Italy | During the period from Apr. 2021, when restrictive measures were eased, to Nov. 2021, two peaks of respiratory infections occurred, the first starting in Jun 2021 (atypical for respiratory infections) and the second, much greater peak starting toward the end of Sep. 2021. The infections included RSV, hERV, PIV-1,2,3,4, MPV, influenza virus, CoV, and Ad. | [36] |
| Reopening of schools, daycare, and relaxation of lockdown rules in UK | Resurgence in Ad, rhinovirus, RSV, PIV and CoV upon easing of restrictions, especially after May 2021. | [49] |
| School reopening in Shanghai, China | Resurgence in RSV and PIV 1/3 following school reopening in June of 2020 | [56] |
Note*: RSV: Respiratory Syncytial virus; PIV: Parainfluenza Virus; Ad: Adenovirus; MPV: Human Metapneumovirus; CoV: Non-SARS-COV-2 Coronavirus; hERV: Human Enterovirus/Rhinovirus
Table 2: Impact on respiratory/enteric virus detection following observation and relaxation of non-pharmaceutical interventions.
| High-risk activities | Personal protective equipment | HVAC/air purification | Hand and surface hygiene |
|---|---|---|---|
| Hospital/healthcare center waiting room | Face mask | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth |
| Retirement home for seniors | Face mask | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth |
| Attending concert/sports venue | Face mask | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth |
| Air or bus travel | Face mask | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth |
| Crowded bar | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth | |
| Daycare center | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, disinfection of toys | |
| Hospitality business | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth | |
| School | HEPA filter recirculated air or 100% fresh air | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth | |
| Workplace | Room air purifiers | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth | |
| Retail businesses | Room air purifiers | Increased hand / surface targeted hygiene, avoid touching face, nose, mouth | |
| At home | Room air purifiers | Practice good hand and surface hygiene |
Table 3: Recommendations for observation of NPIs by healthy people in the post-pandemic future.
Literature Review
Impacts of SARS-CoV-2 pandemic NPIs on viral transmission measures
Impact of NPI on COVID-19 caseloads and deaths during the SARSCOV- 2 pandemic: A number of primary literature reports [9-19], have described assessments of the impacts of voluntary or government-imposed NPIs on COVID-19 caseloads (numbers of positive detection results for SARS-CoV-2, etc.), hospitalizations, and deaths, and indices of SARSCoV- 2 transmissibility (e.g., reproduction number, R, i.e., the disease transmission probability per contact). The types of NPIs considered have varied among these reports, but in general, have included increased use of personal protective equipment (masks), increased hand hygiene, and social distancing measures, such as school and business/entertainment closures, intra- and inter-country travel restrictions, bans on indoor or outdoor social gatherings, and stay-at-home (shelter-in-place) mandates. In some cases, the impacts of individual NPIs have been teased out, while in other reports, the impacts of groups of NPIs or the totality of the NPIs implemented (i.e., NPI packages) have been assessed [9-28] (Table 1).
Where the impacts of individual NPIs have been assessed, some interesting and perhaps discrepant results have been obtained. For instance, Courtemanche, et al. reported that the most significant reductions in SARS-CoV-2 caseloads were attributed to shelter-in-place (stay-at-home) orders and entertainment/restaurant closures, while bans on large social gatherings and school closures did not result in significant impacts [10]. On the other hand, Wang, et al. found that school closures alone had minimal impacts on caseloads, hospitalizations, or deaths, while school closures in combination with 75% to 95% reduction in out-of-home contacts resulted in striking reductions in caseloads, hospitalizations, or deaths [11]. The analyses of Keskinocak, et al. showed that voluntary stay-at-home and state-ordered shelter-in-place resulted in 25-36% fewer infections, compared with no interventions or school closures alone [12]. Li, et al. reported that significant decreases in reproduction number (R0) were obtained only through bans on public events [14]. Liu, et al. found that stay-at-home orders resulted in the greatest decreases in reproduction number, followed by mask wearing, bans on large and small social gatherings, and non-essential business closures [18]. The lowest impacts were attributed to interstate travel restrictions and school closures. Wang, et al. reported that daily use of chlorine or ethanol-based disinfectants in households was 77% effective at reducing SARS-CoV-2 transmission (although the concentrations of disinfectants used by participants were not reported) [19].
In addition to these primary literature reports on the impact on SARSCoV- 2 transmission of implementation of NPIs during the SARS-CoV-2 pandemic, numerous systematic reviews on this topic have appeared. Examples of these include [20-24]. The Talic, et al. review assessed the individual contributions of various personal protective NPIs (hand washing, mask wearing, household disinfection) and social isolation NPIs (physical distancing, stay-at-home, case quarantine, school closures, business closures, lockdowns, and travel restrictions and border closures) to SARS-CoV-2/COVID-19 incidence, mortality, or transmission [20]. The authors identified statistically significant reductions in incidence of SARS-CoV-2/COVID-19 through implementation of mask wearing and physical distancing. Hand washing interventions resulted in reductions in SARS-CoV-2/COVID-19 incidence, though statistical significance was not obtained. Conclusions on the effectiveness of the other NPIs evaluated (school closures, business closures, travel restrictions, etc.) were more guarded, and were not based on random effects analysis [20].
Regmi and Lwin. addressed a variety of topics related to implementation of NPIs, two of which addressed the effectiveness of NPIs for reducing the reproduction number (R0). One theme covered the positive impacts of social distancing measures (avoiding crowds, border restrictions, isolation in hospital, appropriate use of personal protective equipment, school closures,and working from home) [21]. Of these, travel restrictions, case quarantine, and school closures were called out as being particularly important. The second theme addressed effective public health interventions (including increased hand hygiene, avoiding crowds and social events, and use of face masks and eye protection) [21]. Quantitative conclusions on effectiveness for reducing R0 were not reported, although qualitative conclusions were made such as “NPI were effective only if integrated with enhanced personal hygiene, environmental sanitization and adequate and appropriate use of PPE (masks, hand washing and coughing etiquette)” [20,21].
The Ayouni, et al. review described 18 studies on NPI effectiveness and the major outcomes of the studies [22]. Again, quantitative conclusions on individual NPIs effectiveness were not reached, but the qualitative conclusion was “The identified studies showed that travel restrictions, borders measures, quarantine of travellers arriving from affected countries, city lockdown, restrictions of mass gathering, isolation and quarantine of confirmed cases and close contacts, social distancing measures, compulsory mask wearing, contact tracing and testing, school closures and personal protective equipment use among health workers were effective in mitigating the spread of COVID-19 with varying degrees” [22].
Modelling studies have been conducted to ascertain the effectiveness of NPIs for reducing SARS-CoV-2 reproduction number (Rt) [23,24]. Flaxman, et al. acknowledged that dissecting out the effectiveness of individual interventions was difficult [23]. The impact of lockdowns was identified as contributing to an 81% reduction in Rt [23]. Sharma, et al. concluded that the greatest impacts on Rt were achieved by business closures (35% reduction) and bans on social gatherings (26% reduction), with lesser impacts achieved through night curfews (13% reduction) and school closures (7% reduction) [24]. In addition, modelling studies have attempted to predict the trajectory of pandemic outcomes (peak number of diagnoses (caseloads), deaths, attack rate, time to peak number of diagnoses) with and without implementation of NPIs, such as maskwearing, hand washing, self-imposed social distancing, governmentimposed social distancing, contact tracing, and/or case isolation [25-27].
Another way to look at the impact of NPIs on the progress of the SARSCoV- 2 pandemic is to observe resurgence in transmission measures following relaxation of the voluntary or government-imposed NPIs. A sampling of the primary literature on this topic is provided in Table 1 [13,14,28]. A depiction of the reduction in COVID-19 caseloads following implementation of very stringent NPIs and resurgence in COVID-19 caseloads following a decrease in stringency of the NPIs is depicted in Figure 1, taken from Sullivan, et al. [13] (Figure 1).
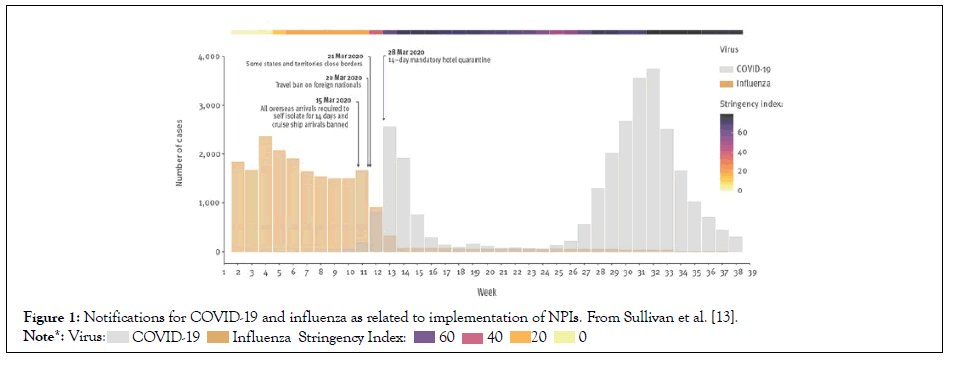
Figure 1: Notifications for COVID-19 and influenza as related to implementation of NPIs. From Sullivan et al. [13].
The preceding discussion provides an indication of the types of data that have been reported on the effectiveness of NPIs on measures of SARS CoV-2 spread and COVID-19 caseloads. As is apparent from Table 1, a variety of NPI have been assessed for effectiveness, through a number of different measures of disease spread (including caseloads, positive viral detection, reproduction number, and mortality). The higher stringency NPI packages, which have included stay-at-home orders, bans on small and large social gatherings, travel restrictions, and personal protective measures, such as mask wearing and increased hand hygiene, appear to have realized the greatest impacts on reduction of viral transmission. We find it surprising that school closures on their own were not found, in every study, to result in more profound reductions in transmission risk for SARS-CoV-2. The disparities in conclusions reached in these studies may have resulted, in part, from the different indices of SARS-CoV-2 transmission used in the studies (especially the use of reproduction number vs. caseloads).
Quantifying the effectiveness of individual NPI used as components of an overall NPI package is clearly difficult to accomplish, and the safest approach to use during this and future pandemics would, therefore, appear to be a combination of the various social distancing and personal hygiene measures described (i.e., an NPI package or “Swiss cheese” approach) [29].
Impact of SARS-CoV-2 NPI on detection of other respiratory and enteric viruses
A more comprehensive search of the literature on the impact of NPIs implemented during the SARS-CoV-2 pandemic on detection of other respiratory and enteric infections was conducted for this review. As the 2019-2020 cold and influenza season in the Northern Hemisphere progressed into 2021, reports began to appear on the rather drastic decreases in caseloads and positive testing outcomes for respiratory syncytial virus (RSV) and influenza virus following implementation of NPIs for the SARS-CoV-2 pandemic [30,31]. An example of the impact on influenza cases during the 2019-2020 influenza seasons is shown in Figures 1 and 2, taken from reference [13]. During normal years, both of these respiratory infections have been associated with significant mortality in children and adults [30].
Additional reports begin to be appear later in 2021, that discussed the decreases in incidence of RSV and influenza virus, as well as other respiratory viruses, especially human metapneumovirus (MPV), parainfluenza virus types 1-4 (PIV), human coronaviruses (CoV), and adenovirus (Ad) [32-35]. Certain of these viewpoint articles also speculated on the possibility of occurrence of additional off-season peaks in respiratory virus detections/cases. The cold and influenza seasons in the Northern Hemisphere (typically October through May, with peaks in December through February) have been unusual. For instance, data from Italy demonstrated very low respiratory virus detections in 2020 and an atypical peak occurring in July 2021 [36] (Figure 2). Decreased detection of enteric viruses has also been reported during pandemic NPI observation periods in 2020 [37] (Figure 3). The common findings from both hemispheres have been that the normal cold and influenza seasons have been relatively non-existent. Many of the other respiratory/enteric infections have also been observed at decreased numbers, in comparison with previous years.
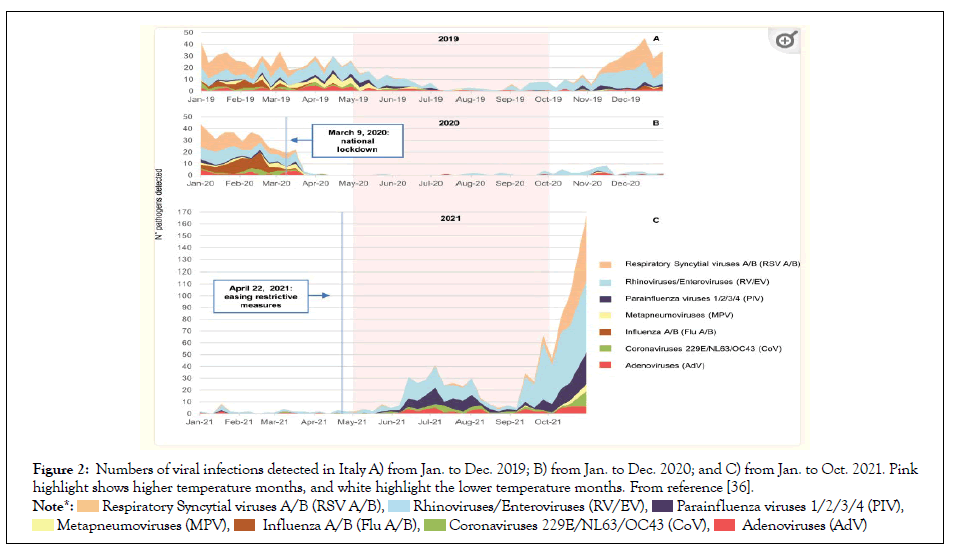
Figure 2: Numbers of viral infections detected in Italy A) from Jan. to Dec. 2019; B) from Jan. to Dec. 2020; and C) from Jan. to Oct. 2021. Pink highlight shows higher temperature months, and white highlight the lower temperature months. From reference [36].
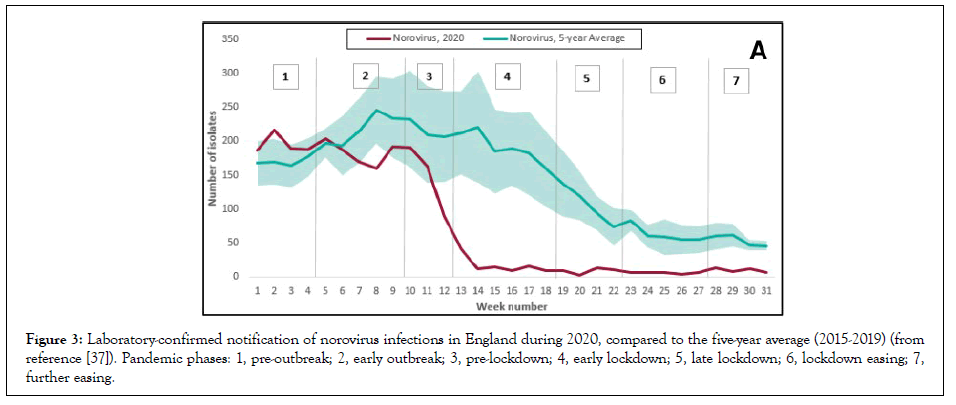
Figure 3: Laboratory-confirmed notification of norovirus infections in England during 2020, compared to the five-year average (2015-2019) (from reference [37]). Pandemic phases: 1, pre-outbreak; 2, early outbreak; 3, pre-lockdown; 4, early lockdown; 5, late lockdown; 6, lockdown easing; 7, further easing.
The results of the primary literature identified on the impact of pandemic NPIs on respiratory and enteric viral infections have been summarized in [13,36-60] (Table 2). As will be noticed, these reports describe reductions in positivity rate, case loads, and reproduction number for respiratory or enteric viral infections. Detection rates for these respiratory/enteric viruses were drastically reduced during the periods of most stringent NPI observation, regardless of geographical region. These papers discuss detection/ transmissibility data for influenza virus [13,36,38-41,43-57], RSV (bronchiolitis) [13,36,38,42-52,54-57], other respiratory viruses [13,36,41,44-49,51-54,56,57], or enteroviruses [36,37,41,45-48,52,54,57]. The primary point of discrepancy among these studies involves the trends for rhinovirus and adenovirus. For instance, some reports describe decreases in detection of these viruses [36,37,41,45,48,57]. Other reports suggested that rhinovirus or adenovirus detections were reduced to lesser extents or were observed only when the most stringent NPIs were implemented [44,46,47,52,54,58,60] [Table 2].
The literature on the impact of pandemic NPIs on influenza viral infections has been reviewed by Rizvi, et al. [61]. These authors analysed 28 studies to attempt to quantify the impact of individual NPIs on measures of incidence, transmissibility, or mortality. The NPIs evaluated included bans on mass gatherings, school closures, travel restrictions, workplace policies (work from home), border restrictions, stay-at-home restrictions, case isolation. It was concluded that NPI packages were more effective than individual NPIs. Outbreak severity and timeliness of implementation of interventions was discussed. The authors stated that “The more widespread the infectious disease and/or the longer the delay in implementation of a measure, the more limited the effectiveness of the intervention” [61].
The various non-SARS-CoV-2 respiratory and enteric viral infections considered in Table 2, are thought to be transmitted from person-to-person via direct transmission through respiratory droplets/aerosols and indirectly via fomites and possibly fecal-oral transmission. As such, it should not be surprising that NPIs intended to mitigate risk for acquiring SARS-CoV-2 also have mitigated risk of acquiring these other viral infections during the ongoing SARS-CoV-2/COVID-19 pandemic.
Another approach for evaluating the effectiveness of pandemic NPIs for reducing transmission measures for non-SARS-CoV-2 respiratory and enteric viral infections is to examine the detection trends following relaxation of the pandemic NPIs (Table 2). This topic has been addressed in a number of publications [36,44,49,51,52,56,58-60]. These papers have examined the consequences of partial relaxation of NPIs, most typically, easing of travel restrictions and reopening of schools and entertainment (i.e., non-essential business) venues. Resurgence in RSV cases and delays in peak caseloads compared with normal RSV seasons have been observed [44,49,56,59,60]. Rhinoviral and enteric virus detections also have been reported to increase following easing of NPIs [36,44,49,51,52,58]. A few papers discussed increases in other respiratory viral infections, such as PIV,CoV, MPV, Ad and influenza virus, following easing of NPIs [36,49,56,58]. In some cases, resurgence of detections of RSV or rhinoviruss, have exceeded peak levels in years preceding the SARS-CoV-2 pandemic [59,44].
Li, et al. examined the factors underlying the resurgence of RSV following relaxation of pandemic NPIs in eighteen countries [62]. The authors concluded that the full re-opening of schools represented the predominant risk factor, with climate (lower temperatures) and duration of time since the last outbreak (higher susceptible population) also being important drivers. Baker, et al. used modelling to attempt to predict the impacts of different durations of NPI observation on the timing and severity of RSV and influenza outbreaks that might occur following cessation of NPI [63]. They suggest that longer periods of NPI observation may lead to the build-up of greater populations of susceptible individuals and, therefore, atypically earlier start to the RSV seasons and greater peak caseloads.
In view of the very light caseloads of the non-SARS-CoV-2 respiratory and enteric viral infections observed globally during the extended SARS-CoV-2 pandemic, concern has been expressed about severe resurgence of these viral infections (especially RSV and influenza) during the upcoming cold and influenza seasons. There may be more people that are vulnerable to such infections, due to waning of immunity [36,63-66]. Not only children are at risk, as the elderly may also be vulnerable [30,64-66,35,63]. As a result of this concern, arguments have been made for retaining at least certain of the pandemic NPIs through the upcoming cold and influenza seasons to help mitigate this risk. In the next section of this mini-review, we provide recommendations on the measures that might appropriately be taken in the post-pandemic future. Of course, the emergence of new SARS-CoV-2 variants on a relatively continuous basis, with some being more transmissible and causing more severe COVID-19 disease than others, makes predictions of when we truly will be in a post-pandemic state challenging. At the time of writing of this mini-review, attention was being paid globally to the Omicron BA.1, BA.2, BA.3 variants and variant recombinants, such as the Delta-Omicron recombinant [67,68].
Learnings from the SARS-CoV-2 pandemic inform recommendations for observation of NPIs in the postpandemic future
What should constitute the NPI package to be utilized in the future to mitigate risk of outbreaks of respiratory/enteric viruses, whether during typical winter seasons, or during off-season peaks? In Asian countries, people historically have been much more likely to observe routine facemask wearing in the setting of community or personal infection. Globally, including within the United States and Europe, the SARS-CoV-2 pandemic has made mask wearing more acceptable, albeit perhaps grudgingly. What about other NPIs? We make the case here for a more targeted approach for apparently healthy people that includes use of selected NPIs during highrisk activities and in the setting of increased community infection. The latter may now be indicated in locations where surveillance techniques for estimating community infection level, such as sewage monitoring for viral RNA, have been implemented [69,70].
Our recommendations Table 3, take into account the degree of transmission risk imparted by different social situations, as well as the realities of compliance expectations (it is unlikely that healthy patrons will wear face masks at the neighbourhood bar, unless forced to by government mandate). In addition, the voluntary NPIs listed below could be complied with to the degree that risk of infection transmission in the community exists.
In lieu of having customers and patrons utilize personal protection, businesses and entertainment venues might invest in Heating, Ventilation, and Air Conditioning (HVAC) or air purifying technologies which are available. These include 100% exhausting/high air change systems, or alternatively, air purifying technologies for air that is intended to be recirculated. Air sanitization practices, including use of portable room air purifiers and use of HEPA filters, are recommended by the U.S. Centers for Disease Prevention and Control (CDC) and other regional public health agencies, including the Chinese CDC, European CDC, and the World Health Organization [3,4,71-73]. Other air purifying technologies include UVC irradiation of air intended to be recirculated. The simplest technology, of course, is to provide 100% fresh air with adequate air changes per hour to prevent stagnant, contaminated air from accumulating within an indoor space.
Individuals with clinical signs of respiratory illness should observe the more stringent measures followed during the SARS-CoV-2 pandemic, in order to limit transmission of their infections to others. In other words, these individuals should wear masks and should engage in cough etiquette when in public. They should avoid crowded locations, avoid air and bus travel, and to the extent possible should work from home and self-quarantine. If this is done, the risk to the healthy population will be lessened and the recommendations mentioned in Table 3 above will be more effective at limiting transmission of an emerging respiratory or enteric virus.
Discussion
Non-pharmaceutical interventions for mitigating risk of transmitting SARS-CoV-2 were implemented to varying degrees and for varying durations globally during the pandemic. The breadth and stringency of these NPIs were unprecedented and, other than the response to SARSCoV in China and limited other global regions, which emerged in 2003, have not been implemented to this degree since the 1918 influenza pandemic. As a result of the severity of the SARS-CoV-2 pandemic, from both public health and regional economy points of view, research during the 2020-2021 timeframe has to a great extent focused on topics related to the SARS-CoV-2/COVID-19 pandemic. The massive proliferation of literature on various topics relating to the pandemic, and the rather novel use of preprints for the rapid dissemination of information, has resulted in studies with some limitations. In fact, the majority of the studies reviewed in this mini-review acknowledged limitations, some of which are discussed below. The evidence summarized in this mini-review indicates that the NPIs were effective in reducing transmission of both the SARSCoV- 2 virus and other infectious respiratory and enteric viruses. In most studies reviewed, it was acknowledged by the authors that it was difficult to determine quantitatively the effectiveness of individual NPIs. This is due to the fact that most regional health authorities mandated NPI packages (i.e., a broad range of social distancing and hygiene approaches implemented concurrently). In some cases, NPIs were implemented or were relaxed in staged approaches (that is, implemented in increasing stringency over time and relaxed in decreasing stringency over time), thus allowing for some assessment of individual NPIs or abbreviated NPI packages.
The importance of NPI was emphasized during the SARS-CoV-2 pandemic, in part due to the possibility of reinfection of individuals with the virus after initial infection. At the beginning, it was not clear to what extent such re-infection might occur. In other words, even if one acquired natural immunity through experiencing a primary SARS-CoV-2 infection, the possibility existed that a subsequent infection of the same virus or variants of this coronavirus might be acquired through relaxation of observance of one or more of the NPI. Further the evolution of the ongoing pandemic has resulted in emergence of a series of variants, subvariants, and recombinants of SARS-CoV-2, some of which have been declared variants of concern due to increased transmissibility, exhibition of immune escape, virulence, or all of the above. Search of the relevant literature indicates that, in fact, the frequency of reinfection, whether with the same virus or with a variant, has been very low, with measured attack rate being less than 1% in previously infected people vs. 4.3% in previously uninfected people in one study and 0.65% in previously infected people vs. 3.27% in previously uninfected people in another study [74,75]. Since it is not yet clear which individuals will respond to either naturally acquired SARS-CoV-2 infections, or vaccines directed against the SARS-CoV-2 spike (or other) proteins, with a robust and lasting immune response, the observation of NPI in vaccinated people as well as in people following natural infections remains of high importance.
Perhaps the most surprising outcome of this mini-review was the discrepant assessments of the effectiveness of school closures for reducing the transmission of SARS-CoV-2 and other respiratory and enteric viruses. This point was brought up in certain of the reviewed papers. For instance, Edwards, et al. noted that reductions in RSV caseloads persisted even when schools reopened in Australia [34]. This was considered remarkable, since school-aged children are major vectors for transmitting RSV and influenza virus to younger children at home [76,77]. El-Heneidy, et al. noted that rhinoviral detection rates increased when schools reopened in Australia, speculating that this was due to children being the key reservoirs for rhinoviral spread [44]. The findings from certain of the reviewed studies that school closures represented a less important factor for reducing transmission of these viruses were surprising to us as well, and as mentioned previously, may relate in part to the different transmission endpoints used in the studies (i.e., caseloads or positive virus detection outcomes vs. reproduction number, etc.). One might also speculate that children are more liable to respond to SARS-CoV-2 infection with asymptomatic or mildly symptomatic cases and, therefore, to shed less virus, although this remains a controversial topic. Rostad, et al. analyzing a dataset published by Chung, et al. concluded that children were less frequently symptomatic than adults, and when symptomatic had fewer symptoms and a shorter duration of symptoms [78,79]. Rostad, et al. concluded that “Taken together, these findings suggest that children may be less likely to transmit SARS-CoV-2 because of reduced frequency and severity of symptoms, which are associated with reduced viral load.” This conclusion differs from that of Jones, et al. who concluded that “PAMS [Presymptomatic, Asymptomatic, and Mildly Symptomatic] subjects had, at the first positive test, viral loads and estimated infectiousness only slightly less than hospitalized patients [80]. Similarly, children were found to have mean viral loads only slightly lower (0.5 log10 units or less) than those of adults and ~78% of the adult peak cell culture isolation probability.”
In certain of the studies reviewed in Table 2, it was reported that rhinovirus and adenovirus detection rates were reduced during the SARS-CoV-2 pandemic to lower extents, and/or only during the most stringent NPIs, compared with other respiratory viruses. The best discussion of possible reasons for this has been offered by El-Heneidy, et al. [44]. The reasons discussed included greater likelihood of seeking viral testing in individuals exhibiting symptoms of respiratory infections, reopening of schools during periods of easing of restrictions, the possibility of rhinovirus (a respiratory virus) being spread also by the oral-faecal route, and the fact that rhinovirus and adenovirus are non-enveloped viruses that exhibit lower susceptibility to non-formulated alcohol- and detergent-based hand hygiene agents [81,82]. Finally, these authors cited a paper suggesting that rhinovirus in droplets (>5 μm in size) or aerosols (≤ 5 μm in size) is less efficiently filtered by the commonly used surgical face masks than coronavirus [83]. The latter finding would not be expected to apply to N95 masks, as testing of an example of the latter by Zhou, et al. indicated that these should be equally capable of filtering the enveloped influenza virus and the non-enveloped rhinovirus [84].
While the studies reviewed in our paper addressing the efficacy of masks as an NPI for reducing risk of acquiring a viral infection have not differentiated between surgical and N95 masks, the differences between N95 masks and the surgical masks and fabric masks more typically utilized during the SARS-CoV-2 pandemic deserve some additional discussion. Surgical masks and fabric masks are typically multi-layered, albeit relatively loose fitting and are intended primarily to serve as a barrier to passage of large droplets or sprays. These serve primarily to protect other individuals in the vicinity of an infected person from viral particles that might be emitted during coughing, sneezing, or speaking of the infected person. For this reason, surgical masks are used in healthcare settings to protect the surgical field [85]. Since such a mask does not serve as an effective barrier for preventing exposure to virus-containing aerosols, small droplets, etc., it becomes apparent that these masks are primarily useful for preventing transmission of an infection from the mask wearer to others, rather than for protecting an uninfected mask wearer. An N95 mask, on the other hand, is one which has been certified by the National Institute for Occupational Safety (NIOSH) to seal to a wearer’s face (requiring a procedure for fitting the mask to the individual) in order to achieve the intended effectiveness of filtering 95% of particles with a mass median diameter of 0.3 micrometers (300 nm) [85]. While coronaviruses are on the order of 60-140 nm in particle size, the aerosols and droplets containing the viruses are expected to be larger in aerosolized body secretions emitted from infected person (<500 nm for respiratory aerosols) [86,87]. Thus, the N95 mask would be expected to protect both an uninfected wearer as well as individuals in the vicinity of an infected wearer, provided that the N95 mask has properly been fitted to the wearer. However, from a practical standpoint, cost and the requirement for fit testing preclude more widespread use of N95 masks during pandemics.
The impact of the NPIs implemented during the SARS-CoV-2/COVID-19 pandemic on the risk of acquisition of enteric pathogens was not limited only to viruses such as human enteroviruses, adenoviruses, or noroviruses, although that is the primary topic of this paper. In fact, detection rates for additional enteric pathogen-associated illnesses, including those attributed to enteropathogenic bacteria (eg., Campylobacter spp, Shiga toxin producing Escherichia coli, Listeria spp, non-typhoidal Salmonella spp, typhoidal Salmonella, Shigella spp), and enteric protozoan parasites (eg., Cryptosporidium spp. and Giardia sp.) were also reduced [37,88,89].
Conclusion
Notwithstanding the limitations of the studies reviewed herein, it is clear that reductions in detection rates for a variety of respiratory and enteric viruses occurred concurrently with implementation of NPIs intended to mitigate risk of transmission of SARS-CoV-2 during the SARS-CoV-2/ COVID-19 pandemic. These results demonstrate the general utility of the NPI packages and individual NPIs (including mask wearing, avoiding large social gatherings, other forms of social distancing, case quarantine, travel restrictions, and targeted surface hygiene, hand and air sanitization, etc.) for mitigating spread of respiratory viruses. These NPIs especially pertain to individuals with obvious clinical symptoms, in order to prevent transmission to healthy people. Moving into the post-pandemic future, we should be vigilant, pre-emptively taking advantage of the learnings described above as we experience further variants of SARS-CoV-2, including its Omicron BA.1 through 5 variants and variant recombinants, such as the Delta-Omicron “deltacron” recombinant as well as other emerging or re-emerging respiratory or enteric viruses.
Author Contributions
Conceptualization, M.K.I. and J.M.; data curation, R.W.N.; writing original draft preparation, R.W.N. and M.K.I.; writing-review and editing, J.R.R., J.M., and C.P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Home-Johns Hopkins Coronavirus Resource Center.
- GLOBAL OUTLOOK. Global Economic Prospects.2022.
- Air Cleaners, HVAC Filters, and Coronavirus (COVID-19).
- Cleaning and Disinfecting Your Home. 2022.
- McHugh J. The 1918 Flu Pandemic Had a Devastating Third Year.
- Morens DM, Taubenberger JK, Harvey HA, Memoli MJ. The 1918 influenza pandemic: lessons for 2009 and the future. Critic Care Med. 2010;38(4):e10.
- Short KR, Kedzierska K, Van de Sandt CE. Back to the future: lessons learned from the 1918 influenza pandemic. Front Cell Infect Microbiol. 2018:343.
- Beach B, Clay K, Saavedra M. The 1918 influenza pandemic and its lessons for COVID-19. J Econ Lit. 2022;60(1):41-84.
- Wu J, Tang B, Bragazzi NL, Nah K, McCarthy Z. Quantifying the role of social distancing, personal protection and case detection in mitigating COVID-19 outbreak in Ontario, Canada. J Math Ind. 2020;10(1):1-2.
- Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures in the United States Reduced the COVID-19 Growth Rate. Health Affairs. 2020;39(7):1237-46.
- Wang X, Pasco RF, Du Z, Petty M, Fox SJ, Galvani AP, et al. Impact of social distancing measures on coronavirus disease healthcare demand, central Texas, USA. Emerg Infect Dis. 2020;26(10):2361.
- Keskinocak P, Oruc BE, Baxter A, Asplund J, Serban N. The impact of social distancing on COVID19 spread: State of Georgia case study. PloS One. 2020;15(10):e0239798.
- Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Eurosurveil. 2020;25(47):2001847.
- Li Y, Campbell H, Kulkarni D, Harpur A, Nundy M, Wang X, et al. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries. Lancet Infect Dis. 2021;21(2):193-202.
- Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-control study of use of personal protective measures and risk for SARS-CoV 2 infection, Thailand. Emerg Infect Dis. 2020;26(11):2607.
- Hartnett GS, Parker E, Gulden TR, Vardavas R, Kravitz D. Modelling the impact of social distancing and targeted vaccination on the spread of COVID-19 through a real city-scale contact network. J Comp Net. 2021;9(6):cnab042.
- Lio CF, Cheong HH, Lei CI, Lo IL, Yao L, Lam C, et al. Effectiveness of personal protective health behaviour against COVID-19. BMC Pub Heal. 2021;21(1):1-10.
- Liu X, Xu X, Li G, Xu X, Sun Y, Wang F, et al. Differential impact of non-pharmaceutical public health interventions on COVID-19 epidemics in the United States. BMC Pub Health. 2021;21(1):1-7.
- Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5):e002794.
- Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, et al. Effectiveness of public health measures in reducing the incidence of Covid-19, SARS-CoV-2 transmission, and Covid-19 mortality: systematic review and meta-analysis. Bmj. 2021:375.
- Regmi K, Lwin CM. Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): a systematic review. Int J Envi Res Pub Health. 2021;18(8):4274.
- Ayouni I, Maatoug J, Dhouib W, Zammit N, Fredj SB, Ghammam R, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Pub Health. 2021;21(1):1-4.
- Flaxman S, Mishra S, Gandy A, Unwin HJ, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257-261.
- Sharma M, Mindermann S, Rogers-Smith C, Leech G, Snodin B, Ahuja J, et al. Understanding the effectiveness of government interventions against the resurgence of COVID-19 in Europe. Nature Comm. 2021;12(1):1-3.
- Zhang Y, Jiang B, Yuan J, Tao Y. The impact of social distancing and epicenter lockdown on the COVID-19 epidemic in mainland China: A data-driven SEIQR model study. MedRxiv. 2020.
- Ge Y, Chen Z, Handel A, Martinez L, Xiao Q, Li C, et al. The impact of social distancing, contact tracing, and case isolation interventions to suppress the COVID-19 epidemic: A modeling study. Epidem. 2021;36:100483.
- Teslya A, Pham TM, Godijk NG, Kretzschmar ME, Bootsma MC, Rozhnova G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020;17(7):e1003166.
- Hatef E, Kitchen C, Chang HY, Kharrazi H, Tang W, Weiner JP. Early relaxation of community mitigation policies and risk of COVID-19 resurgence in the United States. Prev Med. 2021;145:106435.
- McKimm-Breschkin JL, Hay AJ, Cao B, Cox RJ, Dunning J, Moen AC, et al. COVID-19, Influenza and RSV: Surveillance-informed prevention and treatment–Meeting report from an isirv-WHO virtual conference. Antiviral Res. 2021:105227.
- Jones N. How COVID-19 is changing the cold and flu season. Nature. 2020;588(7838):388-90.
- Jenkins C, Sunjaya A. Social distancing as a strategy to prevent respiratory virus infections. Respirol. 2021;26(2):143-144.
- Hansen CL, Chaves SS, Demont C, Viboud C. Mortality Associated With Influenza and Respiratory Syncytial Virus in the US, 1999-2018. JAMA. 2022;5(2):e220527.
- Williams TC, Sinha I, Barr IG, Zambon M. Transmission of paediatric respiratory syncytial virus and influenza in the wake of the COVID-19 pandemic. Eurosurveill. 2021;26(29):2100186.
- Edwards KM. The Impact of Social Distancing for Severe Acute Respiratory Syndrome Coronavirus 2 on Respiratory Syncytial Virus and Influenza Burden. Clinic Infect Dis.2021.
- Zheng Z, Pitzer VE, Shapiro ED, Bont LJ, Weinberger DM. Estimation of the Timing and Intensity of Reemergence of Respiratory Syncytial Virus Following the COVID-19 Pandemic in the US. JAMA. 2021;4(12):e2141779.
- Mattana G, Albitar-Nehme S, Cento V, Colagrossi L, Piccioni L, Raponi M, et al. Back to the future (of common respiratory viruses). J Global Antimicrob Res. 2022:S2213-7165.
- Love NK, Elliot AJ, Chalmers RM, Douglas A, Gharbia S, McCormick J, et al. Impact of the COVID-19 pandemic on gastrointestinal infection trends in England, February–July 2020. BMJ. 2022;12(3):e050469.
- Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020;39(12):e423-427.
- Lei H, Xu M, Wang X, Xie Y, Du X, Chen T, et al. Nonpharmaceutical interventions used to control COVID-19 reduced seasonal influenza transmission in China. J Infect Dis. 2020;222(11):1780-1783.
- Feng L, Zhang T, Wang Q, Xie Y, Peng Z, Zheng J, et al. Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nature Commun. 2021;12(1):1-8.
- Nawrocki J, Olin K, Holdrege MC, Hartsell J, Meyers L, Cox C, et al. The effects of social distancing policies on non-SARS-CoV-2 respiratory pathogens. Open Forum Infect Dis. 2021; 8(7):ofab133.
- Nolen LD, Seeman S, Bruden D, Klejka J, Desnoyers C, Tiesinga J, et al. Impact of social distancing and travel restrictions on non–coronavirus disease 2019 (non–COVID-19) respiratory hospital admissions in young children in Rural Alaska. Clin Infect Dis.2021;72(12):2196-2198.
- Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72(12):2199-2202.
- El-Heneidy A, Ware RS, Robson JM, Cherian SG, Lambert SB, Grimwood K. Respiratory virus detection during the COVID-19 pandemic in Queensland, Australia. Aust N Z J Public Health. 2022;46(1):10-15.
- Doroshenko A, Lee N, MacDonald C, Zelyas N, Asadi L, Kanji JN. Decline of influenza and respiratory viruses with COVID-19 public health measures: Alberta, Canada. Mayo Clin Proc. 2021;96(12):3042-3052.
- Groves HE, Piché-Renaud PP, Peci A, Farrar DS, Buckrell S, Bancej C, et al. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. Lancet Reg Health Am. 2021;1:100015.
- Kim MC, Kweon OJ, Lim YK, Choi SH, Chung JW, Lee MK. Impact of social distancing on the spread of common respiratory viruses during the coronavirus disease outbreak. PLoS One. 2021;16(6):e0252963.
- Bramley A, Crocker-Buque T, Breuer J, Mahungu TW. Evidence of the reduction of acute circulating communicable viruses during the SARS-CoV-2 pandemic in London. J Infect. 2021;83(4):496-522.
- Lumley SF, Richens N, Lees E, Cregan J, Kalimeris E, Oakley S, et al. Changes in paediatric respiratory infections at a UK teaching hospital 2016–2021; impact of the SARS-CoV-2 pandemic. J Infect. 2022;84(1):40-47.
- Kadambari S, Goldacre R, Morris E, Goldacre MJ, Pollard AJ. Indirect effects of the Covid-19 pandemic on childhood infection in England: population based observational study. Bmj. 2022;376.
- Oh DY, Buda S, Biere B, Reiche J, Schlosser F, Duwe S, et al. Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January-September 2020: Analysis of national surveillance data. Lancet Reg Health Eur. 2021;6:100112.
- Wan WY, Thoon KC, Loo LH, Chan KS, Oon LL, Ramasamy A, et al. Trends in respiratory virus infections during the COVID-19 pandemic in Singapore, 2020. JAMA. 2021;4(6):e2115973.
- Huh K, Kim YE, Ji W, Kim DW, Lee EJ, Kim JH, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax. 2021;76(9):939-941.
- Eisen AK, Gularte JS, Demoliner M, de Abreu Goes Pereira VM, Heldt FH, Filippi M, et al. Low circulation of Influenza A and coinfection with SARS-CoV-2 among other respiratory viruses during the COVID-19 pandemic in a region of southern Brazil. J Med Virol. 2021;93(7):4392-4398.
- Friedrich F, Ongaratto R, Scotta MC, Veras TN, Stein RT, Lumertz MS, et al. Early impact of social distancing in response to coronavirus disease 2019 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis. 2021;72(12):2071-2075.
- Liu P, Xu M, Cao L, Su L, Lu L, Dong N, et al. Impact of COVID-19 Pandemic on the Prevalence of Respiratory Viruses in Children with Lower Respiratory Tract Infections in China. Virol J. 2021;18(1):1-7.
- Chiu SS, Cowling BJ, Peiris JM, Chan EL, Wong WH, Lee KP. Effects of Nonpharmaceutical COVID-19 Interventions on Pediatric Hospitalizations for Other Respiratory Virus Infections, Hong Kong. Emerg Infect Dis. 2022;28(1):62.
- Tanner AR, Brendish NJ, Poole S, Pregon J, Clark TW. Increase in circulation of non-SARS-CoV-2 respiratory viruses following easing of social distancing is associated with increasing hospital attendance. J Infect. 2021;83(4):496-522.
- Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73(9):e2829-2830.
- Fourgeaud J, Toubiana J, Chappuy H, Delacourt C, Moulin F, Parize P, et al. Impact of public health measures on the post-COVID-19 respiratory syncytial virus epidemics in France. Eur J Clin Microbiol Infect Dis. 2021;40(11):2389-2395.
- Rizvi RF, Craig KJ, Hekmat R, Reyes F, South B, Rosario B, et al. Effectiveness of non-pharmaceutical interventions related to social distancing on respiratory viral infectious disease outcomes: a rapid evidence-based review and meta-analysis. SAGE Open Med. 2021;9:20503121211022973.
- Li Y, Wang X, Cong B, Deng S, Feikin DR, Nair H. Understanding the potential drivers for respiratory syncytial virus rebound during the COVID-19 pandemic. J Infect Dis. 2022.
- Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJ, Grenfell BT. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci USA. 2020;117(48):30547-30553.
- Welsh, J. Colds and Other Common Diseases Might Surge as Kids Return to School.
- Kelly M. Large, Delayed Outbreaks of Endemic Diseases Possible Following COVID-19 Controls.
- Han S, Zhang T, Lyu Y, Lai S, Dai P, Zheng J, et al. The Incoming Influenza Season-China, the United Kingdom, and the United States, 2021–2022. China CDC Weekly. 2021;3(49):1039.
- . The 1918 Flu Pandemic Had a Devastating Third Year
- Mahase E. Covid-19: What do we know about the delta omicron recombinant variant? BMJ. 2022;376.
- Ahmed W, Angel N, Edson J, Bibby K, Bivins A, O'Brien JW, et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ. 2020;728:138764.
- Peccia J,Zulli A, Brackney DE, Grubaugh ND, Kaplan EH, Casanovas-Massana A, et al. Measurement of SARS-CoV-2 RNA in Wastewater Tracks Community Infection Dynamics. Nat Biotechnol 2020; 38(10):1164-1167.
- Chinese Government’s Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (Trial Version 7). 2022.
- Heating, Ventilation and Air-Conditioning Systems in the Context of COVID-19. 2022.
- WHO Considers “airborne Precautions” for Medical Staff after Study Shows Coronavirus Can Survive in Air.2022.
- Kojima N, Klausner JD. Protective immunity after recovery from SARS-CoV-2 infection. The Lancet 2022;22(1):12-14.
- Hansen CH, Michlmayr D, Gubbels SM, Mølbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397(10280):1204-1212.
- Agoti CN, Phan MVT, Munywoki PK, Githinji G, Medley GF, Cane PA et al. Genomic Analysis of Respiratory Syncytial Virus Infections in Households and Utility in Inferring Who Infects the Infant. Sci Rep. 2019;9(1):1-14.
- Kamigaki T, Mimura S, Takahashi Y, Oshitani H. Analysis of influenza transmission in the households of primary and junior high school students during the 2012–13 influenza season in Odate, Japan. BMC Infect Dis. 2015;15(1):1-8.
- Rostad CA, Kamidani S, Anderson EJ. Implications of SARS-CoV-2 viral load in children: getting back to school and normal. JAMA Pediatri. 2021;175(10):e212022.
- Chung E, Chow EJ, Wilcox ND, Burstein R, Brandstetter E, Han PD, et al. Comparison of symptoms and RNA levels in children and adults with SARS-CoV-2 infection in the community setting. JAMA Pediatri. 2021;175(10):e212025.
- Jones TC, Biele G, Mühlemann B, Veith T, Schneider J, Beheim-Schwarzbach J, et al. Estimating Infectiousness Throughout SARS-CoV-2 Infection Course. Sci. 2021;373(6551):180.
- Lau SK, Yip CC, Lung DC, Lee P, Que TL, Lau YL, et al. Detection of Human Rhinovirus C in Fecal Samples of Children with Gastroenteritis. J Clin Virol. 2012;53(4):290-296.
- Bizot E, Bousquet A, Charpié M, Coquelin F, Lefevre S, Le Lorier J, et al. Rhinovirus: A Narrative Review on Its Genetic Characteristics, Pediatric Clinical Presentations, and Pathogenesis. Front Pediatri. 2021;9:113.
- Leung NH, Chu DK, Shiu EY, Chan KH, McDevitt JJ, Hau BJ, et al. Respiratory Virus Shedding in Exhaled Breath and Efficacy of Face Masks. Nat Med. 2020;26:676-680.
- Zhou SS, Lukula S, Chiossone C, Nims RW, Suchmann DB, Ijaz MK. Assessment of a Respiratory Face Mask for Capturing Air Pollutants and Pathogens Including Human Influenza and Rhinoviruses. J Thorac Dis. 2018;10(3):2059-2069.
- Birkner J, Arey C. The difference between surgical masks and N95s. 2021.
- Ijaz MK, Sattar SA, Rubino JR, Nims RW, Gerba CP. Combating SARS-CoV-2: leveraging microbicidal experiences with other emerging/re-emerging viruses. Peer J. 2020;8:e9914.
- Zuo Z, Kuehn TH, Verma H, Kumar S, Goyal SM, Appert J, et al. Association of airborne virus infectivity with survivability with its carrier particle size. Aerosol Sci Technol. 2013;47:373-382.
- Teimouri A, Alimi R, Farsi S, Mikaeili F. Intestinal Parasitic Infections among Patients Referred to Hospitals Affiliated to Shiraz University of Medical Sciences, Southern Iran: A Retrospective Study in Pre- and Post-COVID-19 Pandemic. Environ Sci Pollut Res. 2022;1:1-9.
- Tang HJ, Lai CC, Chao CM. Changing Epidemiology of Respiratory Tract Infection during COVID-19 Pandemic. Antibio. 2022;11(3):315.
Author Info
M. Khalid Ijaz1*, Raymond W. Nims2, Joseph R. Rubino1, Julie McKinney1 and Charles P. Gerba2RMC Pharmaceutical Solutions, Longmont, CO, USA
3Department of Environmental Science, University of Arizona, Tucson, Arizona, USA
Citation: Ijaz MK, Nims RW, Rubino JR, McKinney J, Gerba CK (2022) Lessons Learned from the SARS-CoV-2 Pandemic: Preparing for the Next Outbreak of Respiratory and Enteric Viral Infections. Appl Microbiol Open Access. 8: 229.
Received: 17-May-2022, Manuscript No. AMOA-22-17521; Editor assigned: 20-May-2022, Pre QC No. AMOA-22-17521(PQ); Reviewed: 06-Jun-2022, QC No. AMOA-22-17521; Revised: 13-Jun-2022, Manuscript No. AMOA-22-17521(R); Published: 21-Jun-2022 , DOI: 10.35284/2471-9315.22.8.229
Copyright: © 2022 Ijaz MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.