Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2022)Volume 7, Issue 6
Objective: The Corona Virus Disease 2019 (COVID-19) has tremendously transformed medical care worldwide, and elective surgery has been affected. The aim of the current study was to determine whether complicated appendicitis rates in children were influenced by the lockdown in April 2022 in Puxi region of Shanghai due to COVID-19.
Background: The progression of acute appendicitis from simple to complicated is affected by the presentation timeliness. In the context of city-mandated control, the influences of lockdown in Puxi April on children suffering from acute appendicitis will be investigated in this study.
Methods: The medical records of all children presenting in 2 hospitals with acute appendicitis between April 1 and April 30, 2022 (The first lockdown month in Puxi region) were reviewed and analyzed as the lockdown group. Moreover, the medical records of the latest 2 years of acute appendicitis in the same period were reviewed and analyzed as the control group. In addition, the clinical and laboratory parameters, treatment ways, intraoperative and pathological findings, and postoperative outcomes were analyzed.
Results: A total of 22 children were diagnosed with acute appendicitis in the first month of the lockdown period in 2 hospitals. Compared with a 2-year control cohort of acute appendicitis, we observed a longer mean duration of symptoms (67.2 ± 77.6 vs. 31.9 ±3 4.7 h, P=0.01) and higher rate (72.73% vs. 43.75%, P=0.038) in children with complicated appendicitis and a long operation time (92.5 ± 35.46 vs. 71.25 ± 34.44 min, P=0.03), as well as a higher CRP (61.82 ± 49.75 vs. 23.43 ± 28.19 mg/dL, P<0.001) and serum bilirubin (19.07 ± 11.07 vs. 10.74 ± 4.37 umol/L, P<0.0001). The mean length of stay was longer in the lockdown group than that in the control group (10.77 ± 5.37 vs.7.70 ± 3.74 d, P=0.0072). The admission WBC and neutrophil percentage had no significant differences, the mean number of hospital or clinic visits had no differences, and the interval between diagnosis and operation has no statistical differences (5.28 ± 2.94 vs. 3.73 ± 3.11 h, P=0.076). However, the overall conservative treatment cases, postoperative morbidity and mortality did not change.
Conclusion: The lockdown affected the symptoms’ duration time of pediatric acute appendicitis. The children in the lockdown period demonstrated higher complicated appendicitis compared with the historical controls, as well as longer mean length of hospital stay.
Appendicitis pediatric; Complicated appendicitis; Corona virus disease; Lockdown
Substantial changes in medical care have occurred worldwide owing to the Corona Virus Disease 2019 (COVID-19) [1-3]. Many studies have reported that medical emergencies had been decreased by the pandemic [4,5]. It is believed that the fear of traveling outside during the pandemic and the fear of contracting the virus in the hospital setting have led to delay in seeking medical care, thus resulting in more complicated presentations of common pediatric pathologies [6]. Acute appendicitis is regarded as one of the most common emergency cases in general surgery in children and the progression is time-sensitive. Delayed diagnosis often lead to more severe diseases, including perforation, intra-abdominal abscess formation and acute peritonitis [7]. Clinical, environmental, and socioeconomic determinants influence the progression of appendicitis in children from simple inflammation to complicated perforation [8]. Since the pandemic has posed additional challenges to emergency surgical care, conservative treatments for acute appendicitis have been established in therapeutic algorithms [9]. It is believed that open appendectomy is a wise option in case of aerosol formation during laparoscopy [10].
It is reported that limited access to pediatrician’s offices may deter families from obtaining timely assessment in the course of appendicitis [11]. Due to the country’s most extensive outbreak of COVID-19 during the spring of 2022, Shanghai was overwhelmed. In response to a dynamic zero-COVID strategy to respond to SARS-CoV-2 variants, the local government had to close schools, factories, and business, and issued the stay-at-home order in April in Pu Xi, Shanghai. Fewer people went out for their normal lives and went to hospitals [12].
The aim of the current study was to determine whether complicated appendicitis cases in children were influenced by the lockdown in April 2022 in Puxi.
We reviewed the records of all children younger than 16 years old with acute appendicitis in Shanghai Children’s Hospital, and Shanghai Jiahui International Hospital, in Puxi region during 2 discrete time periods: a lockdown period between April 1, 2022 and April 30, 2022 as the lockdown group; and a period from April 1, 2020, to April 30, 2021 as the control group. The volume of Emergent Room (ER) visits or general pediatric surgical ER visits in the 2 hospitals were collected too. The study approval was granted through institutional review board agreements of both hospitals.
All patients in the two hospitals with the diagnosis of acute appendicitis were included. However, the patients who received the diagnosis of acute appendicitis as inpatients before the first day of the studies or patients with COVID-19 were excluded. Chronic appendicitis or simultaneous appendectomy during abdominal operations was excluded for other diseases. In addition, the patients who were older than the age of 17 were excluded.
The charts were identified from electronic medical record system of the 2 hospitals via the code “K35” (acute appendicitis) according to the International Statistical Classification of Diseases (ICD-10). The medical records, including progress notes, lab values, and imaging, were reviewed. Radiographic evidence of acute appendicitis was defined by appendiceal dilatation (>6 mm diameter), wall thickening (>3 mm), or peri-appendiceal inflammation. All cases were categorized into uncomplicated or complicated grades based on radiographical or intraoperative and histopathological findings. The patients with complicated appendicitis were delineated from those with non-complicated appendicitis based on the identification of gangrenous or perforated appendix, or with a peri-appendicular abscess. The data analysis included demographics, presentation variables, and number of hospital visits, preoperative assessments, treatment type, intraoperative findings, appendeceal pathology, and inpatient length of stay. The primary outcome was to observe the rates of complicated appendicitis, which was determined by Radiographic report, attending surgeon documentation, or pathologic report.
All data were collected and transferred to a database. They were imported to IBM SPSS Statistics, Version 25 (IBMCorp. Released 2017. Armonk, NY), for statistical analysis. According to the data distribution, the statistical tests were applied using the t test for continuous variables and the chi-squared test or Fisher exact testing for categorical variables. Continuous variables are presented as mean (S.D.) and categorical variables as number with percentages. P values<0.05 were regarded to be statistically significant.
During the first month of lockdown, the number of general pediatric surgical ER visit in Shanghai Children’s Hospital decreased by 38.4% and the number of ER visit in Shanghai Jiahui International Hospital decreased by 29.2%, with 33.4% of decrease on average, compared with the cohort period of the last 2 years. However, the volume of surgery in Shanghai Jiahui Hospital increased by 79.6% (413 vs. 230) during the period of lockdown, compared with the control period (Table 1).
| Hospital | Control period (Mean of 2 years) | Lockdown period | Decrease percentage% |
|---|---|---|---|
| Shanghai Children’s* | 500 | 308 | 38.4 |
| Jia Hui** | 612 | 433 | 29.2 |
| In all | 1112 | 741 | 33.4 |
Note: *Pediatric general surgical ER visits
**ER visits
Table 1: Number of ER visits or pediatric general surgical ER visits in 2 hospitals in the two periods.
We identified 22 acute appendicitis, excluding 1 chronic appendicitis and 1 acute appendicitis with SARS-CoV-2 PCR positive in the lockdown group, as well as 48 cases, excluding 1 chronic appendicitis in the control group (Table 2).
| Variable | Control period (N=48) | Lockdown period (N=22) | P value |
|---|---|---|---|
| Age, y | 8.91 ± 2.86 | 8.08 ± 3.72 | 0.31 |
| Sex, m:f | 27:21 | 8:14 | 0.12 |
| Symptom duration, h | 31.9 (2-192) | 67.2 (7-264) | 0.01 |
| No. of late presentation cases (>48 h) | 11 (22.92%) | 9 (42.86%) | 0.1479 |
| No. of hospitals visited | 1.46 ± 0.58 | 1.23 ± 0.43 | 0.13 |
| Admission WBC 109/L | 15.95 ± 5.1 | 17.03 ± 4.25 | 0.39 |
| Neutrophil % | 80.94 ± 8.18 | 82.58 ± 8.25 | 0.44 |
| CRP, mg/L | 23.43 ± 28.19 | 61.82 ± 49.75 | <0.001 |
| Serum bilirubin, umol/L | 10.74 ± 4.37 | 19.07 ± 11.07 | <0.0001 |
| Complicated appendicitis | 21 (43.75%) | 16 (72.73%) | 0.038 |
| Intervals between diagnosis and operation (h) | 3.73 ± 3.11 | 5.82 ± 2.94 | 0.076 |
| Appendectomy performed | 44 (91.67%) | 18 (81.82%) | 0.24 |
| Operation time | 71.25 ± 34.44 | 92.50 ± 35.46 | 0.03 |
| Length of stay, d | 7.70 ± 3.74 | 10.77 ± 5.37 | 0.0072 |
| Postoperative complications | 6 (13.04%) | 3 (13.64%) | 0.946 |
Table 2: Comparison of appendicitis in children during the lockdown period versus the control period.
A descriptive analysis of the variables of interest was performed in both groups, and the results are shown in Table 2. The mean duration of symptoms before treatment in the lockdown group was nearly 2 times longer than that in the control group (67.2 ± 77.6 vs. 31.9 ± 34.7 h, P=0.01). However, the number of delayed presentation (>48 h) had no statistical significances between the two groups, (42.86% vs. 22.92%, P=0.1479). The reasons for late presentation in the lockdown group included parental ignorance, traffic inconvenience, and the fear of contracting the virus. One main reason for delayed presentation in the control group was misdiagnosis (5 cases were misdiagnosed as gastroenteritis and 3 were misdiagnosed as adenomesenteritis), and another reason was parental ignorance that was observed in 3 cases. There were no statistical differences in parental ignorance between the two groups (Figure 1).
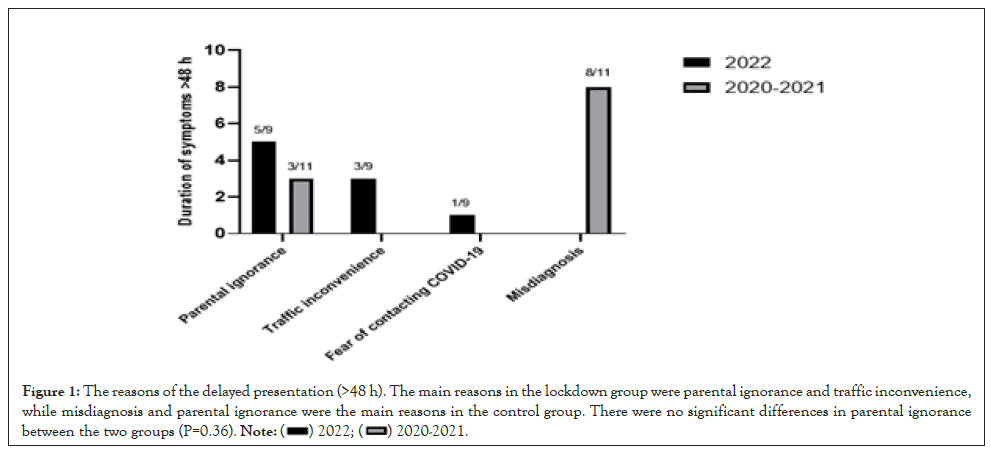
Figure 1: The reasons of the delayed presentation (>48 h). The main reasons in the lockdown group were parental ignorance and traffic inconvenience, while misdiagnosis and parental ignorance were the main reasons in the control group. There were no significant differences in parental ignorance between the two groups (P=0.36).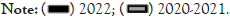
The frequency of medical visits in the lockdown group was lower than that in the control group, without statistical differences (1.23 ± 0.43 vs. 1.44 ± 0.58, P=0.1007). Every patient accepted at least once image examination, either ultrasound or CT scan (Figure 2).
Figure 2: CT scan shows that a 9 years old boy got an acute perforated appendicitis with fecalith. The black arrow indicates the fecalith in the lumen of the appendex. The white arrow indicates that the appendix wall is thick and broken with abscess formation.
The blood test of WBC and neutrophil percentage at admission had no statistical significances in the two groups. However, the serum level of C-reactive protein (CRP) at admission in the lockdown group was greatly higher, compared with the control group, (61.82 ± 49.75 vs. 23.43 ± 28.19, P<0.001). Meanwhile, the serum bilirubin level was significantly higher in the lockdown group, compared with the control group (19.07 ± 11.07 vs. 10.74 ± 4.37 umol/L, P<0.0001). The percentage of complicated appendicitis rose to 72.73% in the lockdown group, but 43.75% in the control group (P=0.037). Eleven (68.75%) complicated appendicitis were diagnosed in the first half of stay-at-home period in the lockdown group. Most patients accepted surgery without differences, with 18 (81.82%) in the lockdown group and 44 (91.67%) in the control group. Totally, 8 cases, with 4 cases in each group, were treated with conservative antibiotics. Six patients had complicated appendicitis with abscess formation and 2 patients in the control group had non-complicated appendicitis whose parents chose the conservative treatment. The interval between diagnosis and operation was 5.28 ± 2.94 hours in the lockdown group and 3.73 ± 3.11 hours in the control group, without statistical differences (P=0.076). The operation time in the lockdown group was longer than that in the control group, (92.50 ± 35.46 vs. 71.25 ± 34.44, P=0.03). The operation time was significantly longer in the lockdown group when the patients who accepted single-incision laparoscopic appendectomy were excluded, (96.53 ± 37.24 vs. 71.25 ± 34.44, P=0.01). The mean length of stay was 10.77 ± 5.37 d in the lockdown group and 7.70±3.74 d in the control group, with statistical significances (P=0.0072). There were no differences in the risks of complications and mortality in the two groups.
Every patent in the lockdown group obtained a SARS-CoV-2 PCR test, and only 1 had a positive result and it was excluded for the different treatment strategy (Figure 3).
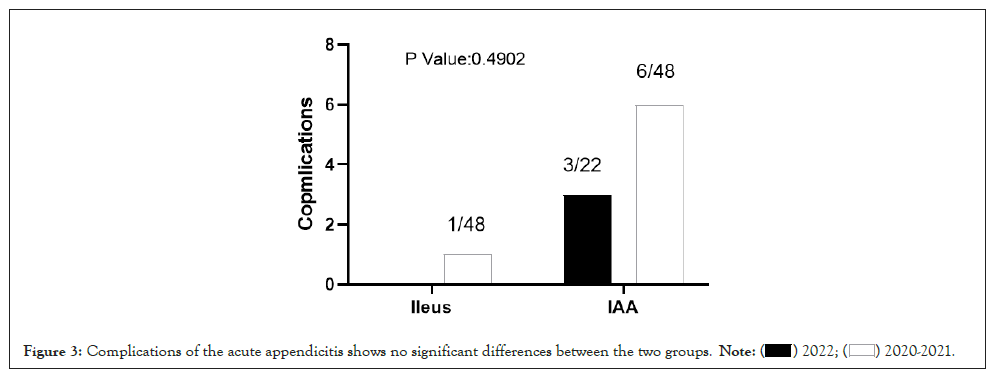
Figure 3: Complications of the acute appendicitis shows no significant differences between the two groups.
A wave of SARS-CoV-2 infection rapidly appeared in the last two months in Shanghai, China. Nearly 0.6 million cases, including 537,726 asymptomatic carriers, have been identified as of April 30, 2022 [13]. Shanghai has issued the stay-at-home order in Puxi region in order to restrict the pandemic from April 1, 2022. The local citizens suffered from daily inconveniences during lockdown [12]. Many hospitals had to close medical service temporarily, due to the hospitalized COVID-19 positive patients. COVID-19 has greatly changed medical care worldwide too. It has reported that the ER visits reduced nearly 50%-60%, especially in younger children below the age of 10 years [6]. Overall, fewer patients would like to visit ER during lockdown for traffic inconvenience and the fear of contamination. Our study indicated that the COVID-19 has affected ER visits. We confirmed that the mean ER visits reduced by 33.4% in 2 hospitals during the period of lockdown in April, which was more obvious in Children’s hospital (nearly 40%). The ER visits were less decreased in Jiahui hospital (about 30%). Interestingly, the surgery volume got a prominent increase in Jiahui hospital, mainly because the hospital was well managed during the period of lockdown.
It is hypothesized that the pathophysiology of acute appendicitis starts with some kind of obstructions, including lymphoid hyperplasia, infection or fecalith, and advances with the increase of intraluminal pressure and ultimate perforation, because the wall had insufficient blood supply and necrosis [14]. Accordingly, the longer the patients’ duration of symptoms is, the higher the likelihood of perforation is. Early diagnosis of acute appendicitis and consequent appropriate treatment in children is important, as it may prevent complications such as appendix perforation, abscess formation and other postoperative complications. In the pediatric population, complicated appendicitis accounts for the minority of cases (approximately 35%) [15]. In this study, we found that the duration time in the lockdown group was 2 times longer than the control group. Subsequently, the complicated appendicitis was more, occupying over 70% of the cases in the lockdown group, which is much higher compare with the control group. These findings are similar with the literature reports [16-18]. Furthermore, the inflammation marker CRP and serum bilirubin were significantly higher in the lockdown group, while the WBC and neutrophil percentage of blood tests had no significance between the two groups. The reasons of late visit demonstrated that the main reason was parental ignorance, misdiagnosis or traffic inconvenience that was very similar to the reason in developing countries [19-21].
However, there was no misdiagnosis in the lockdown group: One reason may be that tertiary hospital was the prioritized option for traffic inconvenience during the lockdown period. We also investigated the number of hospital visits to identify whether more hospitals visits led to the delay to the study hospitals. Actually, the results had no differences, which mean that hospitals referring are not the reason of delayed presentation during the lockdown period in this study. Oppositely, the number of hospital visits during the lockdown period is mildly fewer than that in the control group. The reasons may be that the symptoms of long duration were much more typical and easier to diagnose or inconvenient alternative hospitals during the quarantine. In the lockdown group, only 1 case that was afraid of contracting COVID-19 in hospitals for late visit was identified. It is much lower than the literature reports, because maybe the sample size was very small or the citizens knew that omicron BA.2 is less virulent [6,22,23]. One late visit patient was neglected by his parents, because he had a fever and was mistaken as COVID-19 infection by the family.
Antibiotics alone can successfully treat children and adult patients with uncomplicated appendicitis [24-27]. Non-Operative Management (NOM) for acute appendicitis has been recommended to treat adult acute appendicitis, with satisfactory outcomes during the pandemic [9,10]. However, the changes need further evaluation [28]. We didn’t find any strong recommendation of NOM for acute appendicitis in children with COVID-19 test negative. There were no differences on NOM between the two groups in the study. The reason of NOM for 4 cases in the lockdown group and 2 cases in the control group was complicated appendicitis with abscess formation, because they missed the timing of surgery, another 2 NOM in the control group were their parents’ determination. Appendectomy is the most common abdominal emergent surgery among pediatric population. Laparoscopy appendectomy has replaced open appendectomy as the preferred surgical technique [29,30]. However, traditional open appendectomy is recommended in case of the aerosol formation in the laparoscopy during the pandemic [31,32]. In this study, only one patient was COVID-19 positive and accepted open appendectomy and the patient was excluded from the lockdown group. Over 80% patients accepted appendectomy in the lockdown group. Fifteen patients were treated with traditional laparoscopic appendectomy and 3 were treated with single-incision laparoscopic appendectomy in the lockdown group. The mean operative time was 20 minutes longer in the lockdown group owing to more complicated appendicitis. Initially, we thought that it might be related to the different procedures, since single-incision needs more time. However, we found that, when the single-incision cases, which were only in the lockdown group, were excluded, the operation time was 25 minutes longer than that in the control group. Single incision procedure decreased operation time, because maybe the single-incision was only performed for uncomplicated appendicitis. There was no conversion to open surgery or unrespectable appendix during the operation in the two groups.
The current literature reported that the overall incidence of post- appendectomy complications in children is from 5% to 30%, around 10% in average [33]. Knaapen reported that the incidence is nearly 25% that is higher in complicated appendicitis (about 38%), especially in tertiary hospitals [34]. Both the hospitals in our study are tertiary ones, the incidence of post-operative complications in this study is about 13.6% in the lockdown group, which is not statically different from the control group. The complications in our study are not so high: One reason is that we didn’t collect the data of mild complications such as antibiotic related complications, and another reason is that our length of stay was significantly longer than the literature reported, so the post-operative complication of readmission was lower. No readmission was identified till now in our study. However, the complications in our study are a little higher, compared with the literature reports (around 10%). These findings stood in line with previous findings, which suggested that late diagnosis is related to higher incidence of complications [35].
There are several shortcomings in the article and the authors could identify. The limitations of our study include those inherent to a retrospective review. Another limitation is that the follow-up time for patients treated in the lockdown group is obviously shorter than that in the control group. The postoperative complications in the control group have been collected over 1 or 2 years. The limited sample size and limited time from the two hospitals affected the ability to obtain the accurate estimates on the rate of perforation in the whole city during the whole lockdown period.
We identified that the lockdown significantly impacted ER visits and led to an overall increase in delayed presentation and complicated appendicitis. The patients with complicated appendicitis had an increased length of stay and longer operative time. How to decrease the pre-hospital time may decrease the incidence of complicated appendicitis.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Li H, Xv W, Huang X, Li Q, Wu Y (2022) Long Duration and Increase in Pediatric Complicated Appendicitis during the Period of Lockdown in April 2022 in Shanghai. Clin Pediatr. 7:225.
Received: 01-Nov-2022, Manuscript No. CPOA-22-18980; Editor assigned: 03-Nov-2022, Pre QC No. CPOA-22-18980 (PQ); Reviewed: 17-Nov-2022, QC No. CPOA-22-18980; Revised: 23-Nov-2022, Manuscript No. CPOA-22-18980 (R); Published: 30-Nov-2022 , DOI: 10.35248/2572-0775.22.7.225
Copyright: © 2022 Li H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.