Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 5
Aim: To evaluate the safety and efficacy of low-level light therapy+meibomian gland compression in patients with evaporative dry eye due to meibomian gland dysfunction.
Materials and methods: Prospective study that included 39 patients who underwent low-level light therapy with eye light®+meibomian gland compression at Clinica La Luz in Lima, Peru. Performing a total of 4 sessions with a time interval of 15 days per session with 15 mins duration. Evaluating the Ocular Surface Disease Index (OSDI) questionnaire, Non-invasive Keratograph Break-up Time (NIKBUT), non-invasive tear rupture time, non-invasive meniscometry, pre-meibography to see the degree of atrophy, quality and quantity of meibum compression of meibomian glands, classified from 1 to 4, the presence and decrease of telangiectasias.
Results: In NIKBUT, mean (± SD) before 3.93 ± 1.61, one month after the first 2 sessions 13.57 ± 4.31, up to 8 months of follow-up 19.36 ± 3.32. Being statistically significant (P<0.001). In meniscometry, mean (± SD) before 0.19 ± 0.02, one month after the first 2 sessions 0.30 ± 0.05, 0.32 ± 0.04 after 6 months of follow-up, being statistically significant (P<0.001). In OSDI, the mean (± SD ) pre was 38.85 ± 8.02 , at month 13.03 ± 5.77 and 3 months 13.54 ± 2.98 and 6 months the mean (± SD ) pre was 12.64 ± 3.02. Being statistically significant (P<0.001).
Conclusion: Low Level light Therapy (LLLT)+meibomian gland compression is safe and effective, reducing the symptoms and signs of dry eye for up to 8 months of follow-up. Being an alternative option for patients who do not improve with conventional treatment. However, more long-term studies are needed.
Low-level light therapy; Meibomian gland dysfunction; Dry eye disease; Ocular surface
Dry eye is a multifactorial disease of the ocular surface, characterized by a loss of tear film homeostasis and accompanied by ocular symptoms, in which instability and hyperosmolarity of the ocular surface, inflammation and damage of ocular surface and neurosensory abnormalities play important etiologic roles [1].
Most recent consensus of Tear Film and Ocular Surface Society- Dry Eye Workshop II (TFOS-DEWS II), Dry Eye Disease (DED) has a high prevalence in the world population between 5% and 50%, but can reach 75% in adults older than 40 years, and women are affected more frequently. In young adults only 2.7% experience in Electro-Optical System (EOS) [2].
Evaporative dry eye is the triggering factor as a result of meibomian gland dysfunction, generally characterized by obstruction. The meibomian glands fulfill an important function, since they are in charge of secreting and synthesizing a mixture of wax, cholesterol esters, triglycerides and phospholipids that are part of the outer or lipid layer of the tear film, helping the its stability and avoiding its evaporation [3,4].
An introduction in recent years for the management of dry eye treatment has been low level light therapy or photo-biomodulation with the eye light equipment®, Bologna, Italy. Widely used in dermatological and ophthalmological uses that consists of applying light-emitting diodes or broadband sources between 590 nm to 633 nm, but when applied with ophthalmological treatment, the recommendation is 15 min duration with a total fluence of 100 joules/cm2 and an emission power of 100 mW/cm2 of photo-biomodulation, being absorbed by endogenous chromophores in the absorbed tissue, producing a thermal effect on the irradiated tissue, which leads to coagulation and ablation of blood vessels and therefore their reduction, generating a greater intensity of photons therefore a greater penetration under the skin, resulting in the repair of cells or also called cell photo-activation [5,6].
This equipment is used based on the degree of dysfunction of the meibomian glands that the patient presents, also using the Fitzpatrick skin scale, to be able to use the energy levels standardized by the manufacturer of the eye light® equipment, obtaining a safe and effective effect when being non-invasive [7]. The current prospective study was to evaluate the effects of Low Level Light Therapy (LLLT)+meibomian gland compression on symptom improvement. All the variables evaluated based on the Keratograph 5M equipment [8].
Prospective study that was carried out in 39 patients with a total of 78 eyes, in patients diagnosed with evaporative dry eye due to meibomian gland dysfunction. Treated with low level light therapy with eye light®+meibomian gland compression between July 2022 and October 2022, with an 8-month follow-up in the cornea department of Clinica La Luz in Lima, Peru. All patients gave their written approval to the medical ethics committee for the use of information from medical records and treatment, in accordance with the guidelines of the Declaration of Helsinki.
We included patients with evaporative dry eye due to meibomian gland dysfunction, patients who had grade 2 and 3 atrophy or shortening of the glands due to meibogramia, who had already been on conventional refractory treatment, such as corticosteroids, artificial tears, and patients with chronic blepharitis with the presence of mild to severe telangiectasias.
The exclusion criteria were patients who did not agree to give their approval to carry out the work and patients who abandoned the treatment from the 2nd session, pregnant women and children, patients allergic to any laser were performed with an interval of 15 days per session with a duration of 15 min, with a fluence of 100 joules/cm2 and an emission power of 100 mW/cm2 standardized recommendations by the manufacturer and as described by Stonecipher, and with Meibomian Gland Dysfunction (MGD) 3 eyelid stimulation, all with skin type according to the Fitzpatrick scale of I-IV. Evaluating the OSDI questionnaire, pre, 1, 3, 6 and 8 months, non-invasive tear breakup time, NIKBUT, pre, 1, 6 and 8 months and non-invasive meniscometry, pre, 1, 6 and 8 months. Meibography before treatment to evaluate its morphology, all these tests performed with keratograph® 5M , we also evaluated the quality and quantity of the meibum of the meibomian glands before and from the 1st to the 4th session with compression, classified from 1 to 4 (grade 1: normal, clear and easily secreted meibum; grade 2: cloudy meibum at slight pressure; grade 3: cloudy meibum at higher pressure; grade 4: no meibum secretion with 3 attempts), presence of telangiectasias before after treatment at 1, 3, 6 and 8 months of follow-up, clinically classified as mild (1/3 of the eyelids, moderate (only lower eyelids), severe (upper and lower eyelids) and normal (they did not have).
Technique
We proceeded to the dry eye spa area, where we semi-laid the patient on the stretcher, we put on the previously disinfected mask, explaining that he must keep his eyes closed during the treatment, programmed with eyelid stimulation for meibomian gland dysfunction 3, with a duration of 15 min per session, with a fluence of 100 joules/cm2 and an emission power of 100 mW/cm2 as indicated by the manufacturer. After the end of the session, the patient is positioned in the slit lamp, for gland compression with a special Arita forceps, performed by the same ophthalmologist, taking a photograph of the gland compression with the support of his ophthalmology resident. At the end of each session, the patient was explained not to use creams on the face for a week and not to use makeup, the first 5 days of treatment to avoid any type of reaction.
Post LLLT medication
At the end of each session, tear treatment was started with 0.4% sodium hyaluronate drops without preservatives every 4 hours, 0.1% fluorometholone acetate drops every 12 hours until the end of the 4 sessions, and in patients who had cloudy meibum expression at higher pressure, tobramycin 0.3% was added. Dexamethasone 0.1% ointment every 8 hours for 7 days. After the end of the 4 sessions, the ocular lubricant was maintained every 8 hours.
Statistical analysis
Quantitative variables were summarized using the mean, standard deviation, and range (minimum and maximum value) statistics. For the analysis of the change of the quantitative variables as a function of time, the box and whisker diagram was used. Changes over time with respect to the pre-period were evaluated using the Kruskal-Wallis test. The tests that were significant were subjected to the multiple comparisons test using Dunn's test that included p-values adjusted by the Bonferroni method.
Qualitative variables were summarized using absolute and relative frequency tables. For the analysis of the change of the qualitative variables as a function of time, the stacked bar diagram was used. The independence of time with respect to the level of the variable was evaluated using the Chi-square test based on a Monte Carlo simulation.
For all the comparisons, a=0.05 (type I error) was considered as the limit value to indicate the presence of statistically significant differences. All calculations were performed using the statistical program R version 4.3.0 (https://www.r-project.org/).
45 patients underwent the procedure with low-level light therapy+meibomian gland compression, of which only 39 patients (100%) met the inclusion criteria to carry out the analysis. The mean age was (SD=range). Female sex 29(74.4%), male 10(25.6%), skin type according to the Fitzpatrick scale, I (15.4%), II (17.9%), III (20.5%) and IV (46.2%) (Table 1).
| LLLT+compression of meibomian glands | No% |
|---|---|
| No. of patients | 39(100%) |
| Gender | |
| Female | 29(74.4%) |
| Male | 10(25.6%) |
| Age of patients (years) | |
| Mean ± SD | 49.07 ± 14.25 |
| Age range | 22-76 |
| Fitzpatrick skin type | |
| Yo | 6(15.4%) |
| II | 7(17.9%) |
| II | 8(20.5%) |
| IV | 18(46.25%) |
| Diagnosis | |
| Evaporative dry eye by DGM | 39(100%) |
Note: LLLT: Low Level Light Therapy; SD: Standard Deviation
Table 1: Demographic and clinical characteristics of participants.
The mean (± SD) before treatment was 3.93 ± 1.61, one month after the first 2 sessions it improved 13.57 ± 4.31, at 6 months of follow-up after completing the 4 sessions it remained stable 17.96 ± 4.07, as well as up to 8 months of follow-up there was no decrease 19.36 ± 3.32. Being statistically significant (P<0.001) (Figure 1).
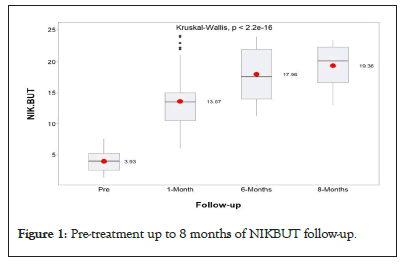
Figure 1: Pre-treatment up to 8 months of NIKBUT follow-up.
Meniscometry
The mean (± SD) before treatment was 0.19 ± 0.02, one month after the first 2 sessions it improved 0.30 ± 0.05, at 6 months of follow-up after completing the 4 sessions it remained unchanged 0.32 ± 0.04, being statistically significant up to this month of follow-up (P<0.001) , and at 8 months a reduction of the meniscus 0.28 ± 0.06 was observed (Figure 2).
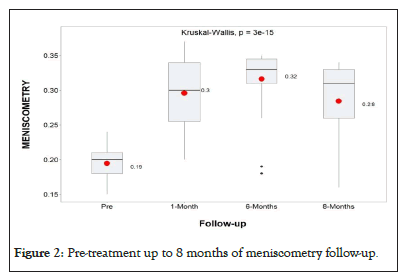
Figure 2: Pre-treatment up to 8 months of meniscometry follow-up.
Ocular Surface Disease Index (OSDI)
The mean (± SD) before treatment was 38.85 ± 8.02, they were between moderate to severe dry eyes, one month after the first 2 sessions there was a slight-moderate improvement of 13.03 ± 5.77, at 3 months of follow-up after having completed. During the 4 sessions 13.54 ± 2.98 remained mild, at 6 months of follow-up they remained without symptoms of dry eyes in normal 12.64 ± 3.02, being statistically significant up to this time and at 8 months of follow-up we observed that the symptoms of dry eyes passed slightly moderate 17.59 ± 10.31 (Figure 3).
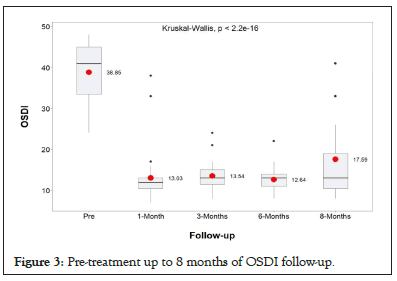
Figure 3: Pre-treatment up to 8 months of OSDI follow-up.
Telangiectasis
The presence of telangiectasias was evaluated, clinically mild (1/3 of the eyelids, moderate (lower eyelids only), severe (upper and lower eyelids) and normal (they did not have) before starting treatment, 43.6% of the patients presented stage severe, 1 month after the first 2 sessions 64.1% telangiectasias were in the mild stage, 3 months after the 4 sessions they remained stable in the mild stage 84.6%, at 6 and 8 months they remained mild in 92.3%, being statistically significant (P<0.001) , only 2.6% remained normal at 6 months (Figure 4).
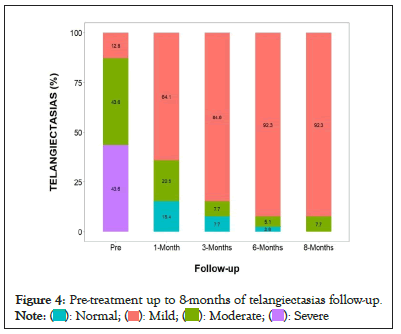
Figure 4: Pre-treatment up to 8-months of telangiectasias follow-up. 
Quality and quantity of expression of meibomian glands
They were classified from 1 to 4 degrees of expression of the meibum. Normal, clear and easily secreted meibum at grade 1, cloudy meibum at slight pressure is grade 2, cloudy meibum at higher pressure is grade 3, no meibum secretion with 3 attempts is grade 4. Before treatment, 69.2% were in (grade 4), in the 1st session 74.4% had improved to (grade 3), in the 2nd session 10.3% were in grade 2 and 59% in (grade 1), they remained that way in the 3rd and 4th session 87.2% and 89.7%, and up to 8 months of follow-up, being statistically significant (P<0.001) (Figures 5 and 6).
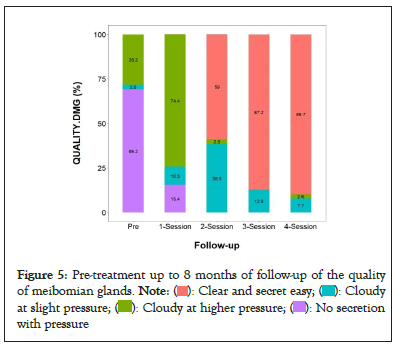
Figure 5: 5: Pre-treatment up to 8 months of follow-up of the quality
of meibomian glands. 
 with pressure.
with pressure.
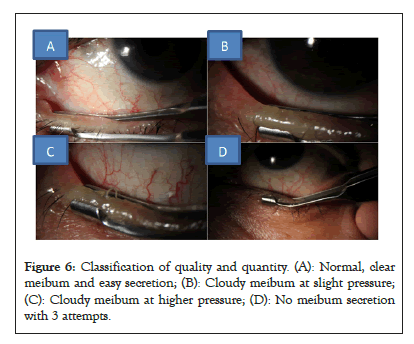
Figure 6: Classification of quality and quantity. (A): Normal, clear meibum and easy secretion; (B): Cloudy meibum at slight pressure; (C): Cloudy meibum at higher pressure; (D): No meibum secretion with 3 attempts.
The application of LLLT associated with the expression of meibomian glands has been seen to be effective for the treatment of evaporative dry eye, providing a long-term improvement of symptoms, restoring the quality of the meibum or increasing the flow of meibum, restoring the stability of the tear film, as well as reducing inflammation, which was evidenced in our work, observing a significant improvement in the evaluation of Meniscometry, NIK-BUT, OSDI questionnaire, telangiectasias evaluated up to 8 months after treatment [9,10].
The use of LLLT in ophthalmology has recently been introduced for the treatment of evaporative dry eye and meibomian gland dysfunction [11,12]. Also known as photo-biomodulation, which involves the application of red or near-infrared radiation using low-power light sources, which stimulates tissue repair, reduces inflammation and relieves pain.
The use of LLLT has proven safe and effective in the treatment of evaporative dry eye due to meibomian gland dysfunction, since no adverse effects were found after the application of the treatment, the same result that was found in recent studies, such as that of Giannaccare, et al. [13] in which Low-Level Light Therapy (LLLT) home devices were used, which were safe in addition to obtaining promising positive results after the application of the treatment, to the evaluation of the average NIKBUT of the first and last session there was an increase from 5.29 to 11.28 and a low OSDI score from 32.00 to 20.71, compared to our results where NIKBUT values were found from 3.93 to 19.36 and OSDI from 38.85 to 17.59, a significant improvement is observed in the production and stability of tear film along with symptoms of ocular discomfort. In comparison, we observed a greater reduction in symptoms and better results from NIKBUT in our work, this due to the fact that the treatment was complemented with the expression of meibomian glands [14].
We can therefore say that this system (NIKBUT) turns out to be useful as an objective, non-invasive diagnostic test and independent examiner that can serve to improve the comparability of the data and standardize the methods of examination of the tear film [15].
In the study by Park, et al. [16] where the efficacy of LLLT was evaluated for the treatment of dry eye and MGD, in the evaluation of the secretion and expressibility of meibomian glands there was a slight improvement without significant differences. In comparison with our study, where a significant difference was obtained in the expressibility of meibum in 89.7%, where an easy and clear secretion was obtained, after treatment, which reinforces the use of LLLT combined with expression of glands.
As mentioned by Finis, et al. [17] in their study the correlation of the meiboscore with the functional parameters of dry eye suggests that in patients with detectable atrophy of the meibomian glands there is also an alteration in the function of the meibomian glands. Something that in our study is corroborated, recapitulating that 100% of our patients presented a meibography pre-dysfunction of meibomian glands grade 3, (classification by meiboscar loss of meibomian gland greater than 2/3) and it can be seen that gradually after of the sessions improves the quality and quantity of the meibum of the meibomian glands since 69.2% were in (grade 4), in the 1st session 74.4% had improved to (grade 3), in the 2nd session the 10.3% were in grade 2 and 59% in (grade 1), 87.2% and 89.7% remained so in the 3rd and 4th session, and up to 8 months of follow-up, being statistically significant (P<0.001).
The eyelid telangiectasias that are observed in patients with dry eye disease due to MGD are abnormal vessels that carry pro-inflammatory factors that damage the ocular surface and contribute to maintaining the chronic inflammatory process. The use of LLLT has shown a decrease in these inflammatory factors by causing a thrombosis of these vessels and thus preventing the release of inflammatory mediators to the meibomian glands and with it an improvement in ocular symptoms, as well as an objective decrease in the presence of telangiectasias, similar works such as the one carried out by Park, et al. [16] also describe positive results by obtaining an improvement at the level of the eyelids, noting a reduction in swelling and a decrease in telangiectasias, as well as an increase in the secretion of the meibomian glands. On the other hand, in the work of Park, et al. [16-19] in the evaluation of the rest of the eyelid such as swelling and telangiectasias as well as discharge and expressibility, only a slight improvement was obtained without significant differences.
In comparison, in our study, significant positive results were obtained, regarding the evaluation of the eyelid, finding at the beginning of the treatment the presence of moderate to severe telangiectasias in 97.2% and after treatment only mild telangiectasias were observed in 92.3%, which reinforces the use of these new therapies for the treatment of MGD. Low-level light therapy+compression of meibomian glands is considered a safe and effective treatment in improving the symptoms of dry eyes, in addition to reducing inflammation of the eyelids by reducing telangiectasias and an improvement in quality of expression of the meibomian glands maintaining an effect of up to a time of 6 months to 8 months. For what we consider, more research is needed to define the time of effect in the improvement of symptoms.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Cayatopa FS, Lazo LKV, Mendez PT, Mendez ALG (2023) Low Level Light Therapy plus Compression of Meibomian Glands for the Treatment of Evaporative Dry Eye. J Clin Exp Ophthalmol. 14:958.
Received: 25-Aug-2023, Manuscript No. JCEO-23-25437; Editor assigned: 28-Aug-2023, Pre QC No. JCEO-23-25437 (PQ); Reviewed: 11-Sep-2023, QC No. JCEO-23-25437; Revised: 18-Sep-2023, Manuscript No. JCEO-23-25437 (R); Published: 26-Sep-2023 , DOI: 10.35248/2155-9570.23.14.958
Copyright: © 2023 Cayatopa FS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.