Chemotherapy: Open Access
Open Access
ISSN: 2167-7700
ISSN: 2167-7700
Perspective - (2023)Volume 11, Issue 3
Lung cancer continues to be the largest cause of cancer-related death in both men and women Lung cancer is caused by smoking and the use of tobacco products in about 90% of cases. Tobacco use accounts for 87% of lung cancer, it affects primarily in 5 or 6th decade of life. In 70% of lung cancer patient, disease has spread to distant organs. Lung carcinoma is a malignant lung tumour characterized of the lung. If left untreated, this growth has the potential to spread beyond the lung via metastasis into nearby tissue or other parts of the body (Figure 1).
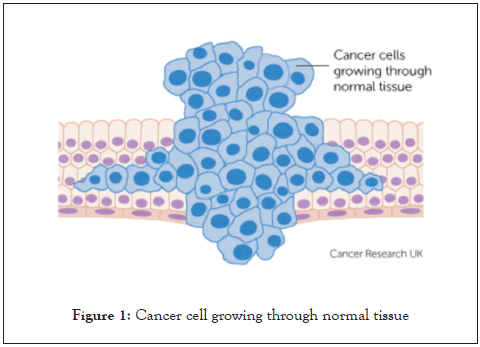
Figure 1: Cancer cell growing through normal tissue.
Non-Small Cell Lung Cancer (NSCLC)
• Large cell carcinoma: NSCLC, which accounts for about 75% to 85% of all cancers, is the most prevalent kind and grows slowly. It is further classified into the following i.e. Epidermoid carcinoma or squamous cell carcinoma.
• Adenocarcinoma: About 25%-30% of lung cancer. The mucus gland of the bronchiole is the source of this substance. It was slow in growth, rarely cavity, strongly linked to cigarette smoking.
• Squamous cell carcinoma: About 30%-35% of lung cancer. The bronchial epithelium causes slow development and cavitation, although metastasis is uncommon.
Small Cell Lung Cancer (SCLC)
It usually begins in one of the larger breathing tubes, grows quickly, and is large by the time it is diagnosed.
• Spreads more quickly and aggressively.
• Accounts for 15% of cases.
• Found mostly in heavy smokers (Figure 2).
Figure 2: Cancer cell growing in lungs.
Etiology:
• Tobacco smoke Smoking is by far the most significant risk factor for lung cancer. Smoking is considered to be responsible for about 80% of lung cancer fatalities.
• Workplace exposure to other cancer-causing chemicals, such as uranium. Chemicals such as beryllium, silica, coal products, and mustard gas can all be inhaled.
• Certain dietary supplements two large studies discovered that smokers who used beta carotene supplements had a higher risk of lung cancer.
• Exposure to asbestos- People who work with asbestos.
• Talc and talcum powder are minerals that may include asbestos in their natural state.
Sign and symptoms:
• A cough that does not go away or gets worse
• Unexplained weight loss
• Infections that do not go away or return, such as bronchitis and pneumonia.
• Shortness of breath
• Hoarseness
• Coughing up blood or rust-colored sputum (spit or phlegm)
• Chest pain that is often worse with deep breathing, coughing, or laughing
• Loss of appetite
• Feeling tired or weak
• New onset of wheezing.
Medical history and physical exam
Blood test:
• A complete blood count (CBC) determines whether patient blood has normal number of different types of blood cells.
• Blood chemistry test can help spot abnormalities in some of patient organs, such as the liver and kidney. For example, e.g. high level of lactate dehydrogenase (LDH).
Imaging tests:
• Chest x-ray: This is often the first test will do to look for any abnormal areas in the lungs.
• Computed tomography (CT) scan: ACT scans uses to make detailed cross-sectional images of patient body. Can reveal the size, shape, and location of any lung tumours, as well as enlarged lymph nodes.
• CT guided needle biopsy: If a suspected area of cancer is deep within patient body, a CT scan can be used to guide a biopsy needle into the suspected area.
• Needle biopsy: Can often use a hollow needle to get a small sample from a suspicious area.
• Thoracoscopy: Spread to the spaces between the lungs and the chest wall, or to the linings.
While lung cancer remains a difficult disease to treat, new treatments based on advances in cancer research are being developed. A more personalized approach to treatment based on biological markers and a combination of therapies is likely to produce better results in the future.
None.
The authors declare that they have no conflict of interest.
Citation: Yan ZL (2023) Lung Cancer: Types, Symptoms, Diagnostic Evaluation. Chemo Open Access. 11: 196.
Received: 27-Oct-2021, Manuscript No. CMT-21-14059; Editor assigned: 29-Oct-2021, Pre QC No. CMT-21-14059 (PQ); Reviewed: 12-Nov-2021, QC No. CMT-21-14059; Revised: 22-Sep-2023, Manuscript No. CMT-21-14059 (R); Accepted: 04-Oct-2021 Published: 29-Sep-2023 , DOI: 10.35248/2167-7700.23.11.196
Copyright: © 2023 Yan ZL. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.