Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2020)Volume 11, Issue 4
Purpose: To investigate the incidence of unintentional macular displacement by using fundus auto-fluorescence
(FAF) imaging in eyes undergoing PPV for repair of primary rhegmatonous retinal detachment (RRD) and
tamponated with either silicon oil (SO) or gas, its association with symptoms of visual disturbance.
Methods: Prospective study including 40 eyes with fresh RRD. 3 port pars planavitrectomy was done with gas or
silicon oil tamponade. Three months after surgery macular displacement was evaluated by fundus autofluorescence.
Results: Of the 40 cases, After silicon oil removal or complete gas absorption, macular displacement was evaluated
by fundus autofluorescence fundus autofluorescence images showed retinal displacement in 11 eyes (27.5%) after
surgery. In SO group, 3 eyes showed retinal displacement upwards with incidence (15%). In Gas group, 8 eyes showed
retinal displacement downwards with incidence (40%). In the patients with evidence of retinal displacement on FAF,
metamorphopsia and micropsia were present in 81.8% (9/11) eyes and 18.2% (2/11) respectively, on the other hand
in those with no evidence of retinal displacement on FAF , metamorphopsia and micropsia were present in 58.6% (17/29) eyes and 10.3% (3/29) respectively.
Conclusion: Unintentional displacement of the retina after repair of primary and uncomplicated detachments with
PPV may be observed using either SO or gas, but slightly more in gas tamponade, this displacement doesn’t affecting
BCVA of patients.
Macular displacement; Rhegmatogenous retinal detachment; Metamorhopsia
Rhegmatogenous retinal detachment (RRD) is the most common sight- threatening retinal condition requiring urgent intervention [1]. There are three critical preconditions for the occurrence of RRD: liquefied vitreous, tractional forces that creates a retinal break, and fluid gains access towards the subretinal space through the retinal break [2,3]. Surgery is the only effective treatment. The available surgical techniques are scleral buckle (SB) surgery, pars planavitrectomy (PPV) or vitrectomycombined with SB (PPV-SB), while pneumatic retinopexy can also be used in limited cases.
Over the last years, PPV has become the surgery of choice for operating primary RRDs. Although a recent meta-analysis of randomized, prospective, and controlled trials studying scleral buckling versus PPV concluded that there were no significant differences in the results of primary success rate between the two groups, currently, many retinal specialists would choose PPV as the primary technique for the management of uncomplicated RRD. This is because growing advances in instrumentation technology, including direct visualization of vitreous tractions on the retina during surgical steps and the possibility of witnessing the retina reattach intraoperatively, have made PPV more and more popular [2,4-7].
Symptoms of distortion are present between patients who have undergone anatomically successful retinal reattachment, and may occur in despite of good recovery of visual acuity [8-12].
It is likely that visual disturbances following successful rhegmatogenous retinal detachment (RRD) repair results from ectopic replacement of macula photoreceptors [13]. Shiragami et al. described how retinal displacement can be detected postoperatively with help of fundus autofluorescence (FAF) imaging. Hyper-autofluorescent lines were detected parallel to selected retinal blood vessels; it is hypothesised that the hyperautofluorescence is due to hyperactive retinal pigment epithelium (RPE) that had previously been located under main retinal blood vessels and is exposed to light postoperatively. Comparison of the main retinal vasculature and the parallel hyper-autofluorescent ‘ RPE vessel ghost ’ lines thus gives an indication of retinal displacement [14].
Fundus autofluorescence (FAF) has been reported to be an accurate imaging of assessing retinal displacement, and this was the technique of choice in several studies [15]. The aim of this study was to investigate the incidence of unintentional macular displacement by using fundus auto- fluorescence (FAF) imaging in eyes undergoing PPV for repair of primary RRD and tamponated with either SO or gas, its effect on visual acuity and its relation with visual disturbances following rhegmatogenous retinal detachment repair.
This is a prospective observational case series study including 40 eyes of 40 patients underwent three-port PPV with silicone oil or intraocular gas injection for primary RRD. Patients were recruited from the outpatient clinic of the Research Institute of Ophthalmology in Cairo and Fayoum university hospital in Fayoum, Egypt, from the period of October 2017 till December 2018. Uncomplicated primary RRD were defined as RRD without proliferative vitreoretinopathy (PVR) or with PVR grade A (pigment and vitreous haze) or grade B (wrinkling of the inner retinal surface, vessel tortuosity, rolled edge of breaks, and retinal stiffness) [16]. Binocular diplopia wasn’t present in any one of patients preoperatively. All operations were performed by two surgeons, who also decided to choose either silicone oil or gas as intraocular tamponade according to the characteristics of retinal detachment. An informed signed consent was obtained from all participants. Preoperative data collection included a full medical and ophthalmic history, measurement of uncorrected and best-corrected visual acuity (BCVA) using the Snellen chart, which was converted to LogMAR for statistical analysis, characteristics of detachment (location, quadrants involved, number and location of breaks and fovea status), and time from the onset of symptoms to surgery. If more breaks were noted during surgery, they were considered in the final data analysis. Exclusion criteria were history of previous vitrectomy, previous RRD repair, old standing Retinal Detachment (with PVR more than Grade B) and significant media opacity that would preclude adequate fundus imaging.
Surgical procedure
Local anesthesia was induced by peribulbarblock.Twenty threegauge PPV was performed in all patients using EVA Ophthalmic Surgical System (DORC). If needed, a posterior vitreous detachment was induced via active suction with the vitrectomy probe around the optic nerve head. A core and peripheral vitrectomy with scleral indentation was performed, and the vitreous base was shaved to relieve vitreous tractions on the retinal tears.
PFCLs were injected over the the optic disc, if needed, to displace the subretinal fluid to the periphery. None of the eyes underwent peeling of the inner limiting membrane or peeling of ERMs. After cautious inspection of the periphery over 360 degrees, the fluid/air exchange was performed with particular attention to maximal drainage of the subretinal fluid through the original breaks. Neither scleral buckling nor posterior retinotomy was performed. After that endolaser photocoagulation around retinal breaks was performed augmented by 360 degrees barrage if the retina condition required this. PFCLs were completely removed if had been used. Finally, 1000 centistokes SO (polydimethylsiloxane [PDMS]) or long acting gas (C2F6 or C3F8) with the non expansile concentration was used as the internal tamponade. Specifically, gas was used for cases without PVR or PVR grade A, whereas SO was used for cases with PVR grade B and for cases with inferior breaks. Patients were then asked to maintain the prone posture over the next 24 hours after operation.
Post-operative follow up
Patients were followed up on the 1st day post-operatively then after 1 week, 2 weeks, 1 month, 3 months and 6 months respectively.
Full ophthalmological examination was done post-operatively including: BCVA using the Snellen chart which was converted to LogMAR system for statistical analysis, slit lamp examination, dilated fundus examination using indirect ophthalmoscope and the slit lamp bio- microscopy (using 90 diopters lens), Amsler grid testing for metamorphopsia was shown in all cases, and the patients were specifically asked to show to the examiner the location of the distorted lines on the grid, if present. No quantitative assessment of the metamorphopsia was performed. Imaging (FAF & OCT) was typically performed following SO removal for SO cases and after complete absorption of intra ocular gas tamponade for gas cases.
Imaging
Images were obtained with Spectralis HRAOCT (Heidelberg Engineering, Heidelberg, Germany), which combines a spectraldomain OCT with confocal scanning laser ophthalmoscope. FAF photography was performed using a band-pass filter for the excitation light centered at 550 nm (bandwidth, 535_585 nm) and a matched barrier filter centered at 665 nm (bandwidth, 615_715 nm) were obtained at imaging visit. The macular status and the presence of ERMs or any abnormalities were confirmed by the postperative OCT scans.
Image analysis
Postoperatively, the presence of ghost vessels (which was taken as evidence of retinal displacement.) and their position (downward or upward), in B-FAF images , were analyzed in relation to the adjacent retinal vessels by two graders. When there was disagreement between the two graders, a third grader decided which one’s judgment should be accepted.
Statistical analysis
For statistical analysis, patients were split into 2 groups according to their postoperative tamponade: 20 patients in group A with SO and 20 patients in group B with Gas. The collected data was organized, tabulated and statistically analyzed using SPSS software statistical computer package version 22 (SPSS Inc, USA). For quantitative data, the mean and standard deviation (SD) were calculated. Independent t- test was used as test of significance. For qualitative data the number and percent distribution was calculated, Chi squared test or Fischer exact test when appropriate was carried out as a test of significance. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, p<0.05 was considered significant. Only the following predictor variables were included in the multiple logistic regression model: detachment extent (number of quadrants involved), fovea status, PFCL use, macular displacement, visual acuity and visual disturbances after operation, OCT abnormalities and type of tamponade.
Demographics and clinical characteristics of the patient sample
There were 51 eligible patients during the study period of whom 11 were excluded from further analysis due to incomplete followup data.
Specifically, 6 patients did not attend follow-up appointments, 3 patients had early postoperative complications such as retinal redetachment and the two last patients were excluded to equalize the number of patients in each group. Of the 40 patients (22 males, 18 females) whose follow-up data were further analysed, the mean age was 52.8 ± 12.5 years, 20 were treated with PPV, retinopexy and oil tamponade (of whom 18/ 20 had foveainvolving detachments at the time of surgery) and 20 were treated with PPV, retinopexy and gas tamponade (of whom 16/ 20 had fovea-involving detachments at the time of surgery), with no significant difference between the two groups in macular state. The duration of retinal detachment based on the selfreported symptoms was (mean ± SD)12 ± 7.7 days and the number of quadrants detached based on preoperative examination was (mean ± SD) 2.4 ± 0.8.
Macula displacement
After successful retinal reattachment, macular displacement was detected in 11 eyes of 40 eyes (27.5%) based on the presence of ghost vessels on B-FAF imaging. There was agreement between the two graders relative to the presence and location of ghost vessels in relation to the adjacent retinal vessels. In SO group, 3 eyes showed retinal displacement upwards with incidence (15%). In Gas group, 8 eyes showed retinal displacement downwards with incidence (40%). While incidence of retinal displacement in gas group is higher than silicon oil group, but this difference between the two groups in retinal displacement wasn't statistically significant (p value 0.077) (Figure 1).
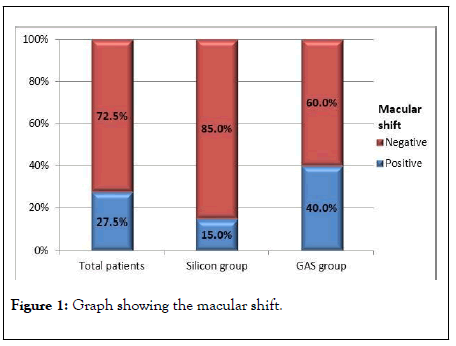
Figure 1: Graph showing the macular shift.
The group with and without retina displacement were comparable for preoperative and postoperative BCVA as well as for anatomic variables such as the extent of RRD and fovea status (Table 1). Intraoperative use of PFCL did not significantly differ between the two groups.
| Macular shift | p value | ||
|---|---|---|---|
| Positive (N=11) | Negative (N=29) | ||
| Mean ± SD | |||
| Pre BCVA | 2.2 ± 0.6 | 2.1 ± 0.9 | 0.934 |
| Post BCVA | 0.7 ± 0.2 | 0.8 ± 0.3 | 0.151 |
| Fovea state | N (%) | ||
| On | 1 (9.1) | 5 (17.2) | 1 |
| Off | 10 (90.9) | 24 (82.8) | |
| Number of quadrants detached | |||
| 1 | 1 (9.1) | 4 (13.8) | 0.642 |
| 2 | 4 (36.4) | 15 (51.7) | |
| 3 | 5 (45.5) | 7 (24.1) | |
| 4 | 1 (9.1) | 3 (10.3) | |
Table 1: The comparison of group with and without retina displacement.
Visual disturbances
In the patients with evidence of retinal displacement on FAF, metamorphopsia and micropsia were present in 81.8% (9/11) eyes and 18.2% (2/11) respectively, on the other hand in those with no evidence of retinal displacement on FAF, metamorphopsia and micropsia were present in 58.6% (17/29) eyes and 10.3% (3/29) respectively (Table 2).
| Variable | Macular shift | p value | |
|---|---|---|---|
| Positive (N=11) | Negative (N=29) | ||
| N (%) | |||
| Metamorphopsia | |||
| Positive | 9 (81.8) | 17 (58.6) | 0.27 |
| Negative | 2 (18.2) | 12 (41.4) | |
| Micropsia | |||
| Positive | 2 (18.2) | 3 (10.3) | 0.603 |
| Negative | 9 (81.8) | 26 (89.7) | |
Table 2: Table showing macular shift.
There was no statistically significant correlation between neither metamorphopsia nor micropsia with the incidence of retinal displacement.This may indicate that retinal displacement is not the only cause of the symptoms of distortion.
Statistical analysis of OCT findings
Overall among 40 eyes treated with vitrectomy for rhegmatogenous retinal detachment, 57.5% (23/40) had an OCT abnormality at this time of imaging (for SO group mean time of imaging is 21.2 ± 7.0 days after SO removal and for gas group first follow up visit following absorption of intraocular gas tamponade). Of the SO group eyes, the abnormalities detected were disturbed the foveal ellipsoid zone (EZ) 5 eyes (25.0%), epiretinal membrane (ERM) 6 eyes (30.0%), cytoid macular edema (CME) 3 eyes (15.0%), Macular hole 1 eye (5%) and subretinal fluid (SRF) 2 eyes (10%). On the other hand, of the Gas group eyes, the abnormalities detected were disturbed the foveal ellipsoid zone (EZ) 1 eye (5%), ERM 8 eyes (40.0%), CME 2 eyes (10%) and SRF 1 eye (5%), with no significant difference between the two groups in distribution of OCT abnormalities.
Statistical values of OCT findings in relation to macular shift
In the patients with evidence of retinal displacement on FAF, the abnormalities on OCT which detected in 7 patients were as follow: ERM 6 eyes (6/11) and CME 2 eyes (2/11) because one eye had both ERM and CME (Figures 2 and 3).
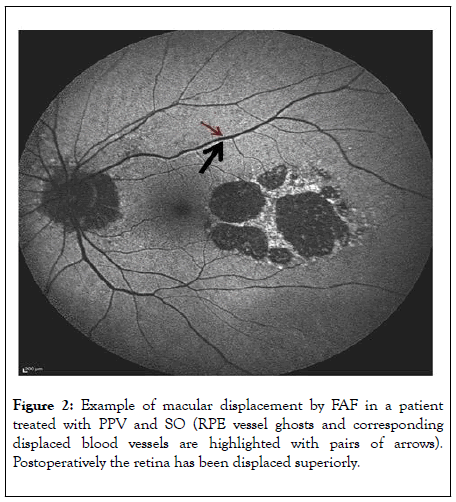
Figure 2: Example of macular displacement by FAF in a patient treated with PPV and SO (RPE vessel ghosts and corresponding displaced blood vessels are highlighted with pairs of arrows). Postoperatively the retina has been displaced superiorly.
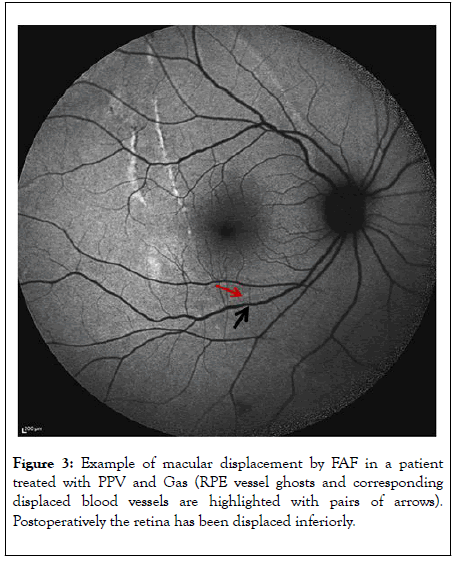
Figure 3: Example of macular displacement by FAF in a patient treated with PPV and Gas (RPE vessel ghosts and corresponding displaced blood vessels are highlighted with pairs of arrows). Postoperatively the retina has been displaced inferiorly.
The purpose of this study was to investigate the incidence of unintentional macular displacement by using fundus autofluorescence (FAF) imaging in eyes undergoing PPV for repair of primary RRD and tamponated with either SO or gas, its association with symptoms of visual disturbance and OCT changes following rhegmatogenous retinal detachment repair.
Incidence of macular displacement
After retinal reattachment, retinal displacement was observed in 11 of 40 eyes (27.5%) based on the presence of RVPs on B-FAF imaging. In SO group, 3 eyes showed retinal displacement with incidence (15%) .In GAS group, 8 eyes showed retinal displacement with incidence (40%).
This is matching with the recent studies conducted by Dell'Omo et al. and Guber et al. in which documented the displacement in 35.2% and 34% of cases respectively [17,18].
Dell'Omo et al. reported that 40 of 97 (41.2%) eyes tamponated with gas versus only 4 of 28 (14.3%) eyes tamponated with SO showed retinal displacement. The small difference in overall incidence of retinal displacement between this study and ours related to the unequal number of each group in their study. While the difference between Guber et al. study and ours may be explained be all their cases were macula off and using gas only.
In the other hand, Codenotti and his associates documented the displacement in 52.2% of cases and the occurrence of retinal displacement was higher in eyes with gas tamponade (10 of 14 eyes; 71.4%) compared with eyes with silicone oil (2 of 9 eyes; 22.2%). The difference between this study and ours is not only the unequal number of each group, but also that Codenotti et al. reported that adjuvant retinotomies were performed to achieve complete retinal reattachment if required [19].
Similar to Shiragami et al. and Cobos et al., showed higher incidence of retinal displacement than ours which were 62.8% and 60% respectively. This may be explained again by using gas only as tamponade [14,15].
While Lee et al. documented the displacement in 72% of 32 consecutive fovea-involving detachments treated with vitrectomy and gas, in 5/17 foveal-sparing cases treated with vitrectomy and gas and in two of two patients with fovea-involving detachments treated with vitrectomy and oil. This results are higher than ours, we detected retinal displacement in only.
29.4% of 34 fovea-involving detachments treated with vitrectomy and in one eye of 6 foveal-sparing cases treated with vitrectomy. This may be related to their using of posterior retinotomies to maximise drainage [20].
Regarding the retinal displacements which were detected in the two patients (2 of 2) who were treated by vitrectomy and oil, Lee and his colleagues concluded that the numbers were not sufficient to justify a definite conclusion and the most likely explanation for displacement in the patients they report relates to their presentation; one with a giant retinal tear; the tear extended from 1 to 5 o’clock temporally, resulting in a very mobile retina and the other with multiple tears in the inferior, temporal and superior quadrants.
Macular displacement and extent of the detachment
In contrast to older studies conducted by Shiragami et al. and Codenotti et al., we did not find any correlation between the number of quadrants involved in RRD and the postoperative presence of macular displacement .While the results of recent studies done by Cobos et al. and Guber et al. in accordance with our result [14,15,18,19].
Macular displacement and PFCL using
In their work on trying to avoid macular displacement, Lee and his colleagues, hypothesized that the use of PFCLs might theoretically reduce the incidence of postoperative retinal displacement evident on FAF by reducing the residual postoperative SRF based on the fact that most studies attribute the displacement to the effect of the residual SRF postoperatively acting as a downward force on the retina hence causing downward displacement of the retina following retinal detachment surgery.
However in our study, of the 11 cases that showed retinal displacement on FAF, PFCL was used in 5 eyes (45.5%) and not used in 6 eyes (54.5%) indicating that its use has no statistical significance in the incidence of retinal displacement.
This is matching with the studies performed by Shiragami et al.Codenotti et al. and Dell'Omo et al. in who also found no statistically significant correlation between the use of PFCLs and reducing the incidence of retinal displacement [14,17,19].
This could be secondary to the fact that a complete drainage of subretinal fluid is not achievable despite PFCL use as shown by intraoperative OCT studies [21,22].
However, Guber and his associates, recommend using of PFCL in macula off retinal detachment repair to prevent retinal slippage [18].
Macular displacement and Visual improvement
Also, we analyzed the functional correlates by analyzing BCVA and the macular displacement in the postoperative follow-up. The logarithm of the minimum angle of resolution BCVA improved from 2.2 ± 0.6 to 0.7 ±0.2 and from 2.1 ± 0.9 to 0.8 ± 0.3 for the eyes with and without displacement, respectively; P value for preoperative mean BCVA is 0.934 and for final mean BCVA is 0.151. There is no statistically significant difference in the final mean BCVA was found between the eyes with and without displacement.
This is similar to the studies published by Shiragami et al. and Dell'Omo et al. who both found no correlation between the incidence of retinal displacement and the final BCVA [14,17].
Type of tamponade and direction of macular displacement
In SO group, we detected hyper-autofluorescent lines, inferiorly and parallel to main retinal vessels, indicating upward retinal displacement in all 3 eyes with displacement.
In Gas group, after gas tamponade, we detected analogous lines superiorly to main retinal vessels course because of retinal downward shifting in all 8 eyes with displacement.
Similar results of the direction of macular shift were obtained with Shiragamiet et al. reported that retinal displacement occurs in downwards direction with gas tamponade. Also Codenotti and his associates reported that retinal displacement occurs in upwards direction with silicon oil tamponade [12,14,19,20].
In the other hand, the study by Dell'Omo, et al. stated that downward and upward displacements may occur with both tamponades, but downward displacement is more common [17].
Metamorphopsia
In this study, metamorphopsia was detected in 26 (65%) patients. In SO group, metamorphopsia was detected in 12 patients (60%). In Gas group , metamorphopsia was detected in 14 patients (70%).
In the 1980s, Amemiya et al. administered a questionnaire about postoperative visual disturbances to 299 RRD patients who underwent scleral buckling. Metamorphopsia was present in 31.10% of them. Okamoto et al. conducted a prospective study among 129 patients who had repaired RRD by either vitrectomy or scleral buckling. Fifty patients (38.76%) had metamorphopsia, which was quantified by M-CHARTS [23,24].
Dell'Omo et al. reported that 22 patients (66.67%) presented with metamorphopsia of 33 patients who had RRDs after vitrectomy. Our results are consistent with the Lee et al. which reported metamorphopsia in 69% of patients. The prevalence of metamorphopsia in our study was 65%, which is at a moderate level when compared with the results from other countries. Many studies have specifically analysedmetamorphopsia among RRD patients with involvement of the macula. Van de Put et al., prospectively followed up 45 patients with macula-off RRDs, and metamorphopsia was present in 39 patients (86.67%) [25,26].
In another series, done by Rossetti et al., consisting of only six eyes with macula-off RRDs, all patients presented with metamorphopsia, which faded with time but persisted in four eyes (66.67%) at 5 years to 6 years after scleral buckling. Zhou and his associates demonstrated that the prevalence of metamorphopsia was 46.58% (177/380), whereas in macula-off cases this number increased to 56.69% (144/254) after a mean follow-up period of 33.94 months. The prevalence of metamorphopsia in our study compared favorably with the results from other studies [27,28]. Potential explanations for this discrepancy may lie in the following aspects. First, the sample sizes differed greatly (our study included 40 eyes and the other studies included 6-380 eyes). However, small sample sizes might be unable to capture the true characteristics of an RRD population. Second, the surgical approaches were dissimilar. In our study, patients underwent only vitrectomy similar to Dell'Omo et al. and Lee et al., other studies had only scleral buckling to repair the RRD [20,25]. The Okamoto’s study, the Van de Put’s study and the Zhou’s study, the patients either underwent vitrectomy or scleral buckling [24,26,28].
Macular displacement and metamorphopsia
In SO group, metamorphopsia was detected in 2 patients of 3 patients who had retinal displacement on FAF (66.7%). In Gas group, metamorphopsia was detected in 7 patients of 8 patients who had retinal displacement on FAF (87.5%). Overall in 11 patients who had retinal displacement on FAF, metamorphopsia was detected in 9 eyes (81.8%).This is in accordance with the study published by Lee and his associates, which reported metamorphopsia in 82.7% of patients with macular displacement (19/23) [20].
On the other hand, our results are slightly less than the results published by Dell'Omo et al., who reported metamorphopsia in 94.7% (18/19) of the patients who had macular displacement. In comparison with Guber et al., our results are higher than their results which were 58.8% (10/17) [18,25].
Additionally, other variances may relate to the different measures to test metamorphopsia, multiple surgeons with diverse experiences, dissimilar patient selection criteria and varied follow-up periods.
Micropsia
Among 40 patients, 5 patients (12.5%) complaining of dysmetropia. All patients who had dysmetropia in our study had micropsia and not macropsia; this is in accordance with the study published by Ugarte and Williamson and Lee and his associates [20,29].
Lee and his associates, agreed with that micropsia would be explained by the fixation target stimulating a smaller number of foveal photoreceptors than in the fellow eye and so further supports the theory that at least some of the displacement seen is due to retinal stretch and hence greater separation between foveal photoreceptors. But surprisingly, in our study, the macular displacement had no correlation with micropsia. Only 2 patients (18.1%) of 11 patients who had macular displacement complaining of micropsia.One patient in each group [20]. Furthermore, we think that there are other mechanisms contribute to micropsia with retinal stretch theory. Such as the facts that RD affects the biochemical interplay between RPE and retinal photoreceptors. And the earliest light microscopic manifestation is: accumulation of subretinal fluid (SRF) with loss of photoreceptor outer segment (OS), and if the process persists the whole photoreceptor layer may become atrophic. Apoptosis apparently has a role in the photoreceptor cell timedecay after occurrence of RD [30].
Simply, micropsia would be explained by the fixaton target stimulating a smaller number of foveal photoreceptors due to loss of many of foveal photoreceptors especially in early postoperative period.
We acknowledge that our study is limited with small number of patients, short follow up period and we did not quantify the metamorphopsia. Further studies using improved OCT and OCT angiography technologies with a larger sample size may more precisely elucidate the relationship between macular microstructures, its vasculature and visual function.
From our point of view, the strengths of this study include its prospective design as well as being randomized also to our knowledge we're the first study to collectively compare the results of vitrectomy with silicon oil and gas, in equal numbers, with nearly similar basal characteristic of both groups as age, duration of retinal detachment and grade of PVR, in terms of anatomical and functional outcomes as well as combining novel imaging modalities as Optical Coherence Tomography (OCT) and Fundus Autofluorescence (FAF) in the comparison of the results between the two groups.
Citation: AbdAllah KK, Kamal MA, Abada MAA, Hatata RM, Azaab AA (2020) Macular Displacement Following Rhegmatogenous Retinal Detachment Repair Using either Silicone Oil or Gas Tamponade: A Comparative Study.J Clin Exp Ophthalmol. 11: 851. DOI: 10.35248/2155-9570.20.11.851
Received: 29-Jun-2020 Accepted: 06-Jul-2020 Published: 13-Jul-2020 , DOI: 10.35248/2155-9570.20.11.851
Copyright: © 2020 AbdAllah KK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.