
Journal of Perioperative Medicine
Open Access
ISSN: 2684-1290

ISSN: 2684-1290
Research Article - (2022)Volume 5, Issue 1
Introduction: Medical comorbidities are diseases unrelated to the causality of the primary surgical finding. Detecting and stabilizing patients with comorbid illness in the preanesthetic evaluation clinic is an essential for reducing perioperative morbidity and mortality. The aim of this study was to determine the magnitude of comorbid illness and their adverse anesthesia outcomes in patients scheduled for elective surgery.
Method: A hospital-based cross-sectional study design was applied to a total of 300 adult patients who were scheduled for elective surgery and visited the preanesthetic clinic from November 2019 to February 2020 G.C. The descriptive data were analyzed by using SPSS version 25 computer program.
Results: Out of 300 patients, 36 (12%) patients had at least one comorbid illness. More than half (55.55%) comorbid illness patients had previously been known and 16 (44.44%) were newly detected. The cardiovascular system comorbid illnesses were 27 (9%). Hypertension 23 (7.7%) was the most common comorbid illness, followed by diabetes mellitus 6 (2%). Out of 300 patients, 17 (5.7%) patients were canceled for different reasons. Referral to medical specialist due to medical comorbid illness was the most frequent reason for elective procedure cancelation. Of all patients with comorbid illness, 19 (52.8%) patients developed intraoperative adverse anesthesia outcomes. Hypertension 13 (68.4) was the most common intraoperative adverse anesthesia outcome, followed by tachycardia 6 (31. 8%).
Conclusion: Comorbid illnesses were not rare in elective surgical patients who visited the preoperative assessment clinic. Cardiovascular comorbid illness, especially hypertension, was the most common comorbid illness detected. Hypertension was also the most common intraoperative adverse anesthesia outcome. In our institution, the presence of comorbid illnesses became the main reason for elective surgeries cancellation.
Comorbid illness; Adverse outcome; Preanesthetic evaluation; Elective
The Medical comorbidities are diseases unrelated to the causality of the principal diagnosis, or they are chronic conditions such as Chronic Obstructive Pulmonary Disease (COPD) and hypertension [1]. Preanesthetic evaluation is the process of clinical assessment by an anaesthetist before the delivery of anaesthesia care for surgical procedures and consists of detailed patient history, physical examination, and investigations based on the patient profile [2]. The preoperative assessment provides an opportunity to optimize the treatment of existing disease and make a detailed plan for care during and after surgery [3].
Traditionally, elective surgical patients have been admitted to the hospital the day before surgery for preanesthetic assessment, risk optimization, and preoperative preparation [4]. The current trend in anaesthesia practice also includes evaluation of risks to compare outcomes, control costs, allocate resources, and postpone surgery until interventions improve risk [5]. Preoperative risk assessment has to be modified, and surgical strategies should go forward with the patient’s preoperative comorbidities rather than age itself [6]. Comorbidity is an independent prognostic factor that has a negative impact on the survival of ovarian cancer patients [7]. Preoperative anaemia is associated with adverse postoperative outcomes in women undergoing gynecological surgery. Unfortunately, this associated risk of preoperative anaemia didnot appear to be corrected by the use of perioperative transfusion [8]. Co morbid patients have more abnormal preoperative laboratory results than non co morbid patients, but the impacts of such tests are nearly indifferent [9]. Some studies indicate that the presence of comorbidity did not significantly affect the outcome of anaesthesia in elective surgical patients. Most of the patients had improved assessment in the last follow-up, but patients from rural regions and those with comorbidity had a higher likelihood of poor cardiovascular outcomes [10,11]. The presence of comorbidities in surgical patients is a significant factor in preoperative morbidity and mortality risk assessment. Coexisting diseases, age, physiologic status, and type of procedure are the four main factors of surgical risk and outcome in patients older than 65 years old [12]. Therefore, any patient undergoing surgery with anaesthesia needs a thorough preoperative evaluation to identify medical illnesses that can affect aesthetic management. Preoperative aesthetic evaluation is aimed primarily to detect and accurately estimate the severity and effects of such medical conditions on patients and the course of the procedure. A study conducted in Taiwan showed that thirty-seven comorbidities can independently predict post aesthetic mortality. This study also indicated that chronic renal failure is the leading contributing comorbidity of 30 days mortality after anaesthesia, which can be explained by the large number of haemodialysis procedures. Another study in Ethiopia indicated that the presence of comorbidity was one of the factors for a prolonged stay in the intensive care unit [13]. Coexisting disease in surgical patients is a significant factor for perioperative morbidity and mortality. Detecting different comorbidities by preanesthetic evaluation is very important for reducing perioperative morbidity and death by determining aesthetic risk, optimizing the detected comorbid illness, planning appropriate anaesthetic techniques, and postoperative care. A study conducted in Nigeria showed that the presence of comorbid illness did not significantly affect the outcome of anaesthesia in elective surgical patients [14]. On the other hand, preoperative anaemia is associated with adverse postoperative outcomes and might not be corrected by perioperative blood transfusion [15]. Many factors, such as age, sex, residency, genetics, and lifestyle, can determine the magnitude of coexisting diseases and their outcome of surgery and anaesthesia. Therefore, the study’s findings in other countries might not be similar to our country. Therefore, this study aimed to determine the extent of comorbidity disease and the adverse anaesthesia outcomes in patients with comorbid illness amongst patients who underwent elective surgery. This study was conducted to evaluate the process of care for these critically ill patients in a non-ICU setting at EWMSC [16,17]. The care required is substantially greater for these cases, requiring more trained staff who understands the importance of each part of the patient care plan. Secondarily, to determine the morbidity and mortality of mechanically ventilated patients cared for outside of the ICU.
Study setting and design
A cross sectional study was conducted on adult patients who were aged 18 years and above who were scheduled and visited the preanesthetic evaluation clinic from November 2019 to February 2020 G.C for elective surgery.
Eligibility
All patients >18 years old who were scheduled for an elective procedure at the study area within the study period
Sample size
All patients 18 and above years old who fulfilled the inclusion criteria and visited the preanesthetic evaluation clinic in the three consecutive months, from November 2019 to February 2020
Data collection process and technique
Questioners and checklists were prepared in the English language that included Sociodemographic data, types of procedures, adverse anaesthesia outcomes, reasons for procedure cancelation, and other intraoperative data. The preoperative and intraoperative data were collected by six anaesthetists after they had received training. The presence of comorbid illness, time of comorbid illness detection, presence and reasons of case cancelation, intraoperative adverse anaesthesia outcomes such as hypertension, hypotension, bradycardia, tachycardia, and other intraoperative data were recorded by assigned data collectors.
Data quality control and assurance
All data collectors were trained by the principal investigator. The pre-test was conducted on 5% of the sample at ‘Soddo Cristian general hospital’. During data collection, regular supervision and follow-up were performed appropriately. The questionnaire was cross-checked for completeness and consistency of data every day. All materials used for data collection were arranged sequentially and stored in a safe and secure place.
Data processing and analysis
The collected data were checked manually for completeness and then coded and entered into epi-data manager version 4.6.0.2 and then transferred to the SPSS version 25 computer program for analysis. Descriptive statistics such as frequency and percentage were used to summarize the data.
Operational definitions
Comorbid illness: Are any concomitant medical illness that happens besides the actual causality that needs surgical intervention?
Cancelation: It is postponing of planned procedure for another day adverse anaesthesia outcome is any unwanted event after the patient gets anaesthesia i.e. cardiac arrest, death, hypertension, hypotension, hypoglycaemia, tachycardia, bradycardia, and shivering delayed recovery.
Pre-existing: Any medical comorbid illness that is detected previously or before pre-anaesthetic evaluation and newly detected is any medical comorbid illness that is first detected during preanesthetic evaluation. Anaemia was defined as low patient haemoglobin when it was <11 g/dl or low patient haematocrit when it was <HCT 30%.
Hypertension is a high patient’s blood pressure when it increases more than 20% of preoperative baseline blood pressure.
Hypotension: Low blood pressure when systolic blood pressure is less than 90 mmHg
Bradycardia: Low heart rate when the heartbeat is less than 60 bpm
Cardiac arrest: It is an absence of apical heartbeat when auscultated by functional stethoscope
Tachycardia: An increased heart rate when the heart rate is more than 130>bpm
Sociodemographic and patient characteristics
A total of 300 patients were involved in this study. Out of 300 patients, 141 (47%) were male and 159 (53%) were female. The mean age of the study participant patients was 39.21 years with a standard deviation of 14.88. All of the study participants had ASA status of III (Table 1).
| Variables | All patients N=300 | Percent % |
|---|---|---|
| Sex | ||
| Male | 141 | 47 |
| Female | 159 | 53 |
| ASA status | ||
| ASA I | 215 | 71.7 |
| ASA II | 78 | 26 |
| ASA III | 7 | 2.3 |
| Smoking status | ||
| Smoker | 5 | 1.7 |
| Nonsmoker | 295 | 98.3 |
| Alcohol taking history | ||
| Yes | 23 | 7.7 |
| No | 277 | 92.3 |
| Age | Mean | Std |
| 39.21 | 14.88 | |
Note: Std: Standard deviation; ASA: American Society of Anesthesiologist
Table 1: Sociodemographic and patient characteristics in WSUTRH from November 2019 to February 2020 G.C.
In this study, the magnitude of comorbid illness was 36 (12%) patients. Out of the 36 patients with comorbid illness, 20 (55.55%) had previously known comorbid illness, while 16 (44.44%) were newly detected in the preanesthetic evaluation clinic. The majority of patients (35.7%) who visited the preanesthetic clinic were scheduled for general surgery followed by gynecology and obstetrics procedures 28%. Spinal anesthesia is a commonly administered anesthesia technique. Out of 300 patients, 17 (5.7%) were canceled. Referral to the medical specialist as a result of comorbid illness was the most common reason 9 (52.94%) (Table 2).
| Type of surgery | Patient with comorbidity | Patient without comorbidity | Total n (%) |
|---|---|---|---|
| General surgery | 15 | 92 | 107 (35.7) |
| Gynecology and obstetrics | 9 | 75 | 84 (28.0) |
| Orthopedics | 3 | 35 | 38 (12.7) |
| Urology | 9 | 36 | 45 (15.0) |
| Neurological | - | 1 | 1 (0.3) |
| ENT | - | 24 | 24 (8.0) |
| Ophthalmology | - | 1 | 1 (0.3) |
| Canceled case | 9 | 8 | 17 (5.7) |
| Anesthesia Technique | |||
| General Anesthesia | 9 | 114 | 123 (41.0) |
| Spinal Anesthesia | 17 | 139 | 156 (52.0) |
| Epidural Anesthesia | - | 1 | 1(0.3) |
| Peripheral Anesthesia | - | 3 | 3(1.0) |
Note: n:number; %:percentage; n%:no comorbid illness, ENT: Eye, Neck and Throat
Table 2: Type of surgery, anaesthesia, and comorbid illness and case cancelation in WSUTRH from November 2019 to February 2020 G.C.
Referral to a medical specialist as a result of medical comorbid illness was the most frequent reason for elective procedure cancelation (Figure 1).
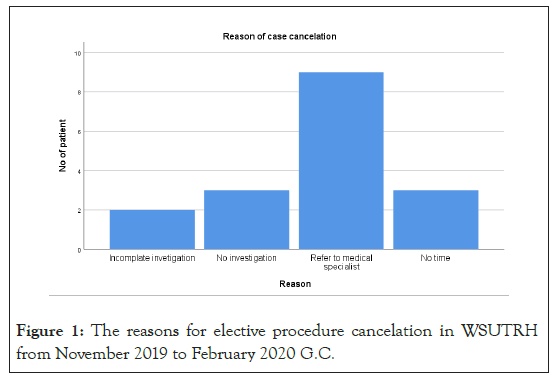
Figure 1: The reasons for elective procedure cancelation in WSUTRH from November 2019 to February 2020 G.C.
Out of 36 (12%) patients who had a comorbid illness, 27 (9%) were identified as the cardiovascular system, while hypertension 23 (7.7%) was the most common comorbid illness followed by diabetes mellitus 6 (2%). Three patients also had both diabetes mellitus and hypertension concomitantly (Table 3).
| Body system affected | No of patients | Percent % |
|---|---|---|
| Cardiovascular system | 27 | 9 |
| Hypertension | 23 | 7.7 |
| Valvular heart disease | 2 | 0.7 |
| Heart block | 2 | 0.7 |
| Reparatory system | 6 | 2 |
| Asthma | 4 | 0.7 |
| Tuberculosis | 2 | 1.3 |
| Central nervous system | 1 | 0.3 |
| Epilepsy | 1 | 0.3 |
| Endocrine system | 7 | 0.3 |
| Diabetes mellitus | 6 | 2.3 |
| Thyrotoxicosis | 1 | 0.3 |
| Gastrointestinal system | 1 | 0.3 |
| Peptic ulcer disease | 1 | 0.3 |
| Hematological system | 2 | 0.7 |
| Anemia | 2 | 0.7 |
| Others systems | 5 | 1.7 |
Table 3: Various comorbid illnesses in elective patients visited the preanesthetic evaluation clinic in WSUTRH from November 2019 to February 2020 G.C.
Out of all patients who had a comorbid illness, 19 (52.8%) patients had developed an intraoperative adverse anesthesia outcome. Intraoperative hypertension was the most common adverse anesthesia outcome, followed by intraoperative tachycardia, which were 6 (16.66%) (Table 4).
| Adverse anesthesia out come | No of patients | Percent% |
|---|---|---|
| Yes | 19 | 6.3 |
| No | 8 | 2.7 |
| Types of adverse anesthesia outcome | ||
| Hypertension | 13 | 4.3 |
| Hypotension | 5 | 1.7 |
| Tachycardia | 6 | 2 |
| Bradycardia | 2 | 0.7 |
| Shivering | 1 | 0.3 |
| Delayed recovery | 2 | 0.7 |
| Hypoglycemia | 3 | 1 |
Table 4: Intraoperative adverse anesthesia outcome among patients with comorbid illness in WSUTRH from November 2019 to February 2020 G.C.
This cross-sectional study aimed to determine the magnitude of comorbid illness and their adverse anesthesia outcomes amongst patients who visited the preanesthetic evaluation clinic after they were scheduled for elective surgeries. Therefore, this study revealed that the overall magnitude of comorbid illness among study participants was 36 (12%). This study’s results do not match those of a similar study conducted in Nigeria and India, which found that the overall comorbidity was 27.3%, 26.5%, and 33.6%, respectively [1-5]. The reasons for this dissimilarity might be due to differences in geographic setting, socio-demographic status, dietary status, ethnicity, lifestyle and number of study participants.
In the current study, among patients with comorbid illness, less than half (44.44%) had newly detected comorbid illness. This result had wide variation from a previous study done in India [6] that showed that 79.7% were newly detected during pre- anesthetic assessment. Around 55.55% percent of comorbidities were previously known before planed procedure schedule and preanesthetic evaluation. The reason might be due to improved information regarding the importance prevention and screening of non-communicable diseases. Hence some study participant might be screened before to know their health status prior they suffer from surgical health problems.
Among the different types of comorbid illness, hypertension (23, 63.9%) was found to be the most common comorbid illness. This finding was similar to the results of a previous study conducted in England, Nigeria, and India (64.3%, 48.8% and 13.8%, respectively) [7-10], but another study revealed that abnormal ECG change was the most common comorbid illness [11]. The reason for this discrepancy might be due to population differences such as age, body mass index, alcohol consumption, life style, dietary habit, and residence i.e. urban or rural. This study also indicated that diabetes mellitus was the second most common comorbid illness, which was a similar study performed in India [12]; however, a study conducted in Nigeria stated that anemia was the second most common comorbid illness.
In the current study, 9 patients with comorbid illness (52.94% of total case cancelation) were canceled because of referral to a medical specialist for further evaluation and management procedure cancelation of elective surgery [13]. This current finding was contradicted by a previous study conducted at other sites in Ethiopia, as the shortage of time and surgeon related were the most common reasons for case cancelation [14]. Another study conducted in Nigeria also reported that there was no cancelation of elective surgery among patients with comorbidity [15]. The reason for this discrepancy might be the difference in the clinical setup of the study site; for example, in the current study site, the preanesthetic evaluation clinic service, including screening and stabilization of patients with comorbid illness, was commenced recently [16]. In this study, among patients with comorbid illness who underwent surgeries, more than half, 52.8% developed intraoperative adverse anesthesia outcomes. Intraoperative hypertension was the most frequent unwanted anesthesia outcome. The current finding contradicted a study in Nigeria that showed that intraoperative hypotension was a more common adverse anesthesia outcome [17]. The reason for this difference might be due to difference in trend of pre anesthetic assessment and stabilization, anesthetic management, fluid management, and even the patient’s response to various anesthetic techniques and surgeries.
The current study revealed that comorbid illness among elective surgical patients was not rare. Cardiovascular comorbid illness, especially hypertension, was the most common comorbid illness among elective surgical patients who visited the preanesthetic assessment clinic. Comorbid illnesses were the most frequent reason for elective procedure cancelation. Even though intraoperative cardiac arrest or death did not occur, the presence of comorbid illness did not mean that it was free of adverse outcomes. Intraoperative hypertension was the most common adverse outcome, followed by tachycardia. A further clinical trial study was recommended on both elective and emergency patients who have a comorbid illness.
The main strengths of this study are obtaining enough study participant patients and using a reliable and comprehensive data collection tool that provides an extensive list of socio- demographic and perioperative variables available, but our study also has limitations, such as failing to control confounding factors of intraoperative adverse anesthesia outcome.
Before conducting the study, ethical clearance was obtained from the WSU ethical review committee. Then, a formal letter detailing the objective of the study was given to the hospital administrator. After permission was obtained from hospital managers, data collectors provided informed consent from each patient. During the data collection process, norms, values, and morals of patients were respected by all data collectors.
None
The authors declared that there is no conflict of interest
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Schoar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Search] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Ayele T (2022) Magnitude and Adverse Anaesthesia Outcome of Co-Morbid Illnesses in Elective Surgical Patients. J Perioper Med. 5:119.
Received: 03-Feb-2022, Manuscript No. JPME-21-7625; Editor assigned: 05-Feb-2022, Pre QC No. JPME-21-7625 (PQ); Reviewed: 17-Feb-2022, QC No. JPME-21-7625; Revised: 24-Feb-2022, Manuscript No. JPME-21-7625(R); Published: 24-Feb-2022 , DOI: 10.35248/2684-1290.22.5.119
Copyright: © 2022 Ayele T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.