Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Review Article - (2024)Volume 13, Issue 4
Introduction: Neural Tube Defects (NTDs) are structural defects of the central nervous system that affect the brain, spine, and spinal column of the developing embryo during the first month of the developmental process. It is one of the top five most serious birth defects in the world. In Somaliland, an accurate estimate of the burden of neural tube defects is still unknown.
Objective: The aim of this study is to determine the overall magnitude and associated factors of neural tube defects in public and private hospitals in Hargeisa, Somaliland.
Methods: We conducted this study in three comprehensive and referral hospitals in Somaliland. A three-year review of the charts of mothers who delivered in these hospitals between January 1, 2019 and December 31, 2022, was done. Moreover, in addition to the data extraction checklist, we developed a structured questionnaire and telephone interviewed 384 randomly selected mothers, including all the mothers with children with neural tube defects. The data were collected by BSc midwives who were trained for 3 days on the methods of data collection. Data were entered, edited, and coded using SPSS Version 23. Descriptive statistics and numerical summary measures were done. Moreover, bivariate and multivariable logistic regression analysis was done to determine factors associated with NTD. Findings were interpreted using the Odds Ratio (OR), with its corresponding 95% C.I. and, P-value <0.05 was considered statistically significant. Finally, results were presented using text, tables, and figures.
Results: A total of 58 NTD cases were identified out of 36,489 live births registered in the three hospitals in Hargeisa, making the overall prevalence of NTDs to be 15.9 per 10,000 births. The most common types of neural tube defects found in the area were hydrocephalus (3.8 cases per 10,000 births), spinal bifida (3.6 cases per 10,000 births) respectively. Mothers in the age groups 33–37 and 38–42 had higher proportions of neural tube defects. According to the multivariable analysis, those with a maternal age of 28–32 have an increased risk of NTD by 27% (AOR: 1.27, 95% CI: 3.32, 4.21), and for those whose ages are between 38 and 42 years, the risk is increased by 9.1 times (AOR: 9.1, 95% CI: 2.70, 30.57). However, gestational age at full term at labor and folic acid intake showed a protective association with neural tube defects (AOR: 0.35, 95% CI 0.16, 0.75) and (AOR: 0.43, 95% CI 0.25, 0.91), respectively. Medication intake increases the risk of developing NTD by 2 times (AOR: 2.05, 95% CI: 1.07, 3.94), while those who take unidentified drugs are 4.47 times more likely to develop NTD (AOR: 4.47, 95% CI: 0.75, 26.72). Caffeine consumption also increased the risk of NTDs by 2.78 times (AOR: 2.78, 95% CI: 1.26, 6.09). Metabolic diseases like gestational diabetes and gestational hypertension were also significantly associated with neural tube defects (AOR: 6.3, 95% CI: 2.01, 19.67) and (AOR: 4.1, 95% CI: 2.06, 8.15), respectively.
Conclusion: The overall prevalence of Neural Tube Defects (NTD) in Somaliland is relatively lower than in other countries in Africa. The most common types of neural tube defects found in the area were hydrocephalus and spinal bifida, respectively. The magnitude of NTDs increased with the mother's age. Maternal age, medication intake, consumption of caffeine, and metabolic diseases like gestational diabetes and gestational hypertension were positively associated with NTDs. However, delivery at full term and folic acid intake during pregnancy were found to have a protective association with NTDs. Hence, health care professionals should focus on maternal safe drug prescription and maternal folate intake and strengthen the existing system in terms of providing maternal health services before and during pregnancy.
Neural tube defects (NTDs) are structural defects of the central nervous system that affect the brain, spine, and spinal column of the developing embryo during the first month of the developmental process [1]. NTDs occur due to incomplete or failed closure of the neural tube. The defects develop during the early weeks of intrauterine development. Failure to close the neural tube during development results in spinal bifida, anencephaly, and encephalocele. These are serious and the leading causes of infant and child mortality, morbidity, and lifelong disabilities [2].
NTDs are multifactorial disorders arising from a complex combination of genetic determinants, including mutations in foliate-responsive or foliate-dependent pathways and family history. Environmental factors include nutritional deficiencies, parental education, maternal ages and occupations, smoking, alcohol consumption, a previous NTD-affected pregnancy, maternal insulin-dependent diabetes, use of anti-epileptic medication, obesity, maternal use of caffeine and medications, exposure to radiation and hyperthermia during early pregnancy.
The death risks and severity of the lesion are determined by factors such as the availability of medical and surgical resources [3]. Advances in medical technology increase the survival rates of babies born with birth defects. But this requires significant financial resources for the long-term care of individuals with disabilities. There is also a significant burden on healthcare systems and caregiver time. It also causes great social and emotional costs for children with NTDs and their families [4].
An estimated 240,000 newborns die worldwide within 28 days of birth every year due to congenital disorders. Congenital disorders cause a further 170,000 deaths in children between the ages of 1 month and 5 years. The most common severe congenital disorders are heart defects, neural tube defects, and Down syndrome [5]. The estimated average global prevalence of NTDs is two cases per 1000 births, amounting to approximately 214,000–322,000 affected pregnancies worldwide annually [6]. The highest burden is in low- and middle-income countries, specifically Africa [2].
Few studies have reported NTD prevalence in low- and middle-income countries (LMICs). However, a recent systematic review of data from available literature, birth defect registries, and published reports from eight countries estimated the NTD prevalence in Africa to be 11.7 per 10,000 live births [7].
In Somaliland, there is a scarcity of data on the magnitude of neural tube defects (NTDs). Moreover, local data are important to understand the real burden of the problem and explore risk factors to design and implement preventive approaches. Hence, this study aimed to determine the overall magnitude and associated factors of NTDs in Somaliland.
Study Site
We conducted this study in three comprehensive and referral hospitals in Somaliland. Namely, Hargeisa Group Hospital, which is a public hospital and the largest and oldest hospital in Hargeisa, was founded in 1953. It provides a variety of health services, including, but not limited to, maternal and child health. The second hospital is Edna Adan Hospital, which is also one of the largest charity maternity hospitals in Hargeisa City. It provides services for the community, especially maternal and child health services, for patients from all parts of Somaliland and other neighborhood regions such as Puntland and southern Somalia. Edna Adan Hospital was founded by a famous lady in the context of Somalia and the world as a whole. Gargar Hospital is the third hospital that has delivered a wide range of health services to mothers and children for over a decade. These hospitals have a better recording and reporting system and data base compared to the other hospitals in Somaliland.
Study design, Period, and Study population
We conducted a three-year’ retrospective chart review on mothers who delivered between January 1, 2019 and December 31, 2022, in the maternity wards of the three hospitals (Hargeisa Group of Hospital, Edna Adan, and Gargar). We reviewed all 36,489 records of women who gave birth at these hospitals during the study period. These hospitals were selected purposefully based on the availability of consistent and valid maternity records.
Data Collection
We developed a data extraction checklist and a pretested structured questionnaire to interview randomly selected (384) mothers who gave birth in those three hospitals, including all the mothers with children with neural tube defects. The interview was through telephone. The data were collected by midwives who have a BSc degree and who were trained for 3 days on the methods of data collection. The pretest was done at Kaah Hospital, which is another nearby hospital located in Hargeisa. Based on the findings from the pretest, modifications were made to the data collection tools. The data collection process was well supervised by the researchers, and to maintain the quality of the data, all checklists and questionnaires were cross-checked on a daily basis.
Data Analysis
Data was entered, edited, and coded using SPSS Version 23. Descriptive statistics and numerical summary measures were done. Moreover, bivariate and multivariable regression analyses were done to determine the association between the independent and dependent variables. Model fitness was checked using the Hosmer and Lemeshow tests. All variables with significant associations in the bivariate analysis were entered into the multivariable logistic regression model to control the confounding effect. Findings were interpreted using the odds ratio (OR), with its corresponding 95% C.I. P-value <0.05 considered statistically significant. Results were presented using text, tables, and figures.
Variables
The dependent variable is neural tube defect (NTD), and the independent variables include sociodemographic characteristics such as age, residence, educational status, occupation, monthly income, folic acid supplementation, gestational age, type of delivery, weight, medication intake, history of diabetes, and hypertension.
Sociodemographic Characteristics of the Participants
A total of 384 women were randomly interviewed, with a response rate of 100%. According to the sex of the children, 53.4% were males and 46.6% were females. The majority (88.5%) of the children’s mothers were married and lived together; about 49.2% had no formal education; 22.7% could read and write; 13.3% had primary education; 8.9% had secondary education; and 6% had a higher level of education. In terms of income, the majority of the respondents (74.2%) had a monthly income between $100 and $400. About 81% of the mothers were housewives, 4.2% were government employees, 4.9% were private employees, and 9.9% were others. Moreover, 64.3% of the participants were urban dwellers, whereas 35.7% were from rural areas [Table 1].
| Variables | n (%) | NGT Status | |
|---|---|---|---|
| Yes | No | ||
| n (%) | n (%) | ||
| Child Sex | |||
| Male | 191 (49.7%) | 31 (53.4%) | 160 (49.1%) |
| Female | 193 (50.3%) | 27 (46.6%) | 166 (50.9%) |
| Mothers’ Marital status | |||
| Married living together | 340 (88.5%) | 48 (82.8%) | 292 (89.6%) |
| Widowed | 24 (6.3%) | 5 (8.6%) | 19 (5.8%) |
| Divorced | 20 (5.2%) | 5 (8.6%) | 15 (4.6%) |
| Mothers’ Education Level | |||
| No formal education | 189 (49.2%) | 27 (46.6%) | 162 (49.7%) |
| Can read and write | 87 (22.7%) | 18 (31%) | 69 (21.2%) |
| Primary | 51 (13.3%) | 9 (15.5%) | 42 (12.9%) |
| Secondary | 34 (8.9%) | 4 (6.9%) | 30 (9.2%) |
| Tertiary | 23 (6%) | 0 (0) | 23 (7.1%) |
| Monthly Income in USD | |||
| 100-250 | 143 (37.2%) | 31 (53.4) | 112 (34.4%) |
| 251-400 | 142 (37%) | 18 (31%) | 124 (38%) |
| 401-600 | 74 (19.3%) | 5 (6.6%) | 69 (21.2%) |
| >600 | 25 (6.5%) | 4 (6.9%) | 21 (6.4%) |
| Mothers’ Occupation | |||
| Housewife | 311 (81%) | 49 (84.5%) | 262 (80.4%) |
| Governmental Employee | 16 (4.2%) | 3 (5.2%) | 13 (4%) |
| Private Employee | 19 (4.9%) | 0 (0) | 19 (5.8%) |
| Others | 38 (9.9%) | 6 (10.3%) | 32 (9.8%) |
| Residence | |||
| Urban | 247 (64.3%) | 23 (39.7%) | 224 (68.7%) |
| Rural | 137 (35.7) | 35 (60.3%) | 102 (31.3%) |
Table 1: The socio-demographic characteristics of the study participants who gave birth in public and private hospitals in Hargeisa, Somaliland
Age of mother and having a child with Neural Tube Defect (NTD)
The following figure denotes the trend of Neural Tube Defect across the different age groups. It implies that there was no as such a difference in the trend of the age group between 18 to 32. However, the trend started to increase with the age groups of 33-37 and 38-42 [Figure 1].
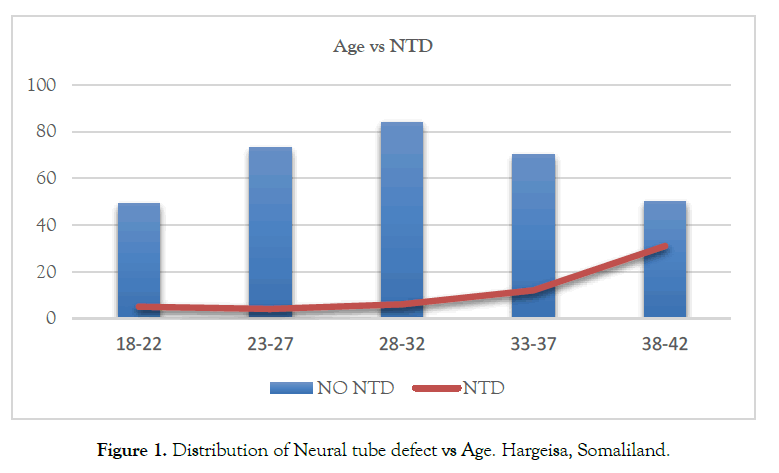
Figure 1. Distribution of Neural tube defect vs Age. Hargeisa, Somaliland.
Reproductive history of the mothers
The majority of the mothers (40.9%) have children aged between 5-8, while 38.8% of the mothers have children aged between 1-4 and the rest 20.6% between 9-13. The majority (94%) of the respondents space their children with 1-2 year’s interval. Around 70% of the respondents did plan to get pregnant. However, 42.2% of the respondents had a history of abortion. Spontaneous Vaginal Delivery accounted for 60% of the mothers, Cesarean section 31.5% and assisted instrumental delivery accounted for 8.3%. Moreover, the majority of mothers (79.7%) who gave birth in these hospitals delivered a preterm baby [Table 2].
| Variables | n (%) | NTD Status | |
|---|---|---|---|
| Yes (n, %) | No (n, %) | ||
| Total Number of children | |||
| 01-Apr | 148 (38.5%) | 28 (48.3%) | 120 (36.8%) |
| 05-Aug | 157 (40.9%) | 15 (25.9%) | 142 (43.6%) |
| Sep-13 | 79 (20.6%) | 15 (25.9%) | 64 (19.6%) |
| History of Abortion | |||
| Yes | 162 (42.2%) | 36 (62.1%) | 126 (38.7%) |
| No | 222 (57.8%) | 22 (37.9%) | 200 (61.3%) |
| Spacing | |||
| 1-2 years | 331 (94%) | 51 (94.4%) | 280 (94%) |
| 3-4 years | 21 (6%) | 3 (5.6%) | 18 (6%) |
| Type of Pregnancy | |||
| Planned | 115 (30%) | 13 (22.4%) | 102 (31.3%) |
| Not Planned | 269 (70%) | 45 (77.6%) | 224 (68.7%) |
| Gestational age at birth | |||
| Term | 78 (20.3%) | 18 (31%) | 60 (18.4%) |
| Preterm | 306 (79.7%) | 40 (69%) | 266 (81.6%) |
| Mode of Delivery | |||
| Spontaneous Vaginal Delivery | 231 (60.2%) | 16 (27.6%) | 215 (65.6%) |
| Instrument assisted vaginal delivery | 32 (8.3%) | 6 (10.3%) | 26 (7.9%) |
| Cesarean section | 121 (31.5%) | 36 (62.1%) | 87 (26.5%) |
Table 2: Reproductive history of the study participants’/children’s mothers, who gave birth public and private hospitals in Hargeisa, Somaliland
Prevalence and types of Neural Tube Defects
During the three years’ period, 36,489 women delivered in the 3 major hospitals in Hargeisa. Of these births a total 58 cases of NTDs were documented. The Overall Prevalence of NTD was found to be 15.9 per 10,000 births. Moreover, the most common types of NTDs were Hydrocephalus (3.8 cases per 10,000 births), Spinal bifida (3.6 cases per 10,000 births), Hydrocephalus and Spinal bifida (4.4 cases per 10,000 births) [Figure 2].

Figure 2. Magnitude and types of NTDs. Hargeisa, Somaliland.
Factors associated with neural tube defects
A bivariate and multivariable logistic regression analysis was conducted to identify factors associated with NTDs. According to the multivariable analysis, those with a maternal age of 28–32 increased the risk of NTDs by 27% (AOR: 1.27, 95% CI: 3.32, 4.21); those whose ages are between 33 and 37 years increased the risk by 3.76 times (AOR: 3.76, 95% CI: 1.05, 13.42); and the age group of 38–42 years increased the risk by 9.1 times (AOR: 9.1, 95% CI: 2.70, 30.57). Gestational age at labor shows a protective association with neural tube defects; being full-term prevents NTDs (AOR: 0.35, 95% CI: 0.16, 0.75). Folic acid intake prevents NTD up to 57% (AOR: 0.43, 95% CI: 0.25, 0.91). Medication intake increases the risk of developing NTDs by 2 times (AOR: 2.05, 95% CI: 1.07, 3.94), while those who take unidentified drugs are 4.47 times more likely to develop NTDs (AOR: 4.47, 95% CI: 0.75, 26.72). Caffeine consumption also increased the risk of NTDs by 2.78 times (AOR: 2.78, 95% CI: 1.26, 6.09). Metabolic diseases like gestational diabetes and gestational hypertension were significantly associated with neural tube defects (AOR: 6.3, 95% CI 2.01, 19.67) and (AOR: 4.1, 95% CI 2.06, 8.15), respectively [Table 3].
| Characteristics | NTD | COR | 95% CI | AOR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Lower | Upper | Lower | Upper | ||||
| Age of the Mother | 18-22 | 5 | 49 | 1 | 1 | 1 | 1 | 1 | 1 |
| 23-27 | 4 | 73 | 0.78 | 0.29 | 2.09 | 1 | 0.22 | 4.21 | |
| 28-32 | 6 | 84 | 0.94 | 0.37 | 2.39 | 1.27 | 0.32 | 4.98 | |
| 33-37 | 12 | 70 | 0.44 | 0.14 | 1.37 | 3.76 | 1.05 | 13.42 | |
| 38-42 | 31 | 50 | 1.7 | 0.68 | 4.33 | 9.1 | 2.7 | 30.58 | |
| Gestational Age | Preterm | 18 | 60 | 1 | 1 | 1 | 1 | 1 | 1 |
| Term | 40 | 266 | 0.5 | 0.27 | 0.93 | 0.35 | 0.16 | 0.75 | |
| History of NTD | No | 43 | 301 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 15 | 25 | 4.2 | 2.05 | 8.59 | 1.57 | 0.62 | 3.9 | |
| History of abortion | No | 22 | 200 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 36 | 126 | 2.6 | 1.46 | 4.62 | 1.32 | 0.69 | 2.51 | |
| Folic acid Use | No | 41 | 165 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 17 | 161 | 0.43 | 0.23 | 0.78 | 0.48 | 0.25 | 0.91 | |
| Use of Medications | No | 26 | 240 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 32 | 86 | 3.44 | 1.93 | 6.09 | 2.05 | 1.07 | 3.94 | |
| Type of Medications | Antihypertensive | 6 | 18 | 1 | 1 | 1 | 1 | 1 | 1 |
| Antidiabetic | 8 | 30 | 0.8 | 0.24 | 2.68 | 0.22 | 0.45 | 1.1 | |
| Antibiotic | 2 | 9 | 0.67 | 0.11 | 3.99 | 0.31 | 0.07 | 1.44 | |
| Herbal drugs | 6 | 4 | 4.5 | 0.94 | 21.56 | 0.29 | 0.04 | 2.25 | |
| Other* | 10 | 26 | 1.15 | 0.36 | 3.74 | 4.47 | 0.75 | 26.72 | |
| Caffeine Intake | No | 11 | 171 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 47 | 155 | 4.71 | 2.36 | 9.41 | 2.78 | 1.27 | 6.1 | |
| History of Thyroiditis | No | 43 | 282 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 15 | 44 | 2.24 | 1.14 | 4.36 | 1.16 | 0.36 | 3.81 | |
| Previous G. diabetes | No | 40 | 279 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 18 | 47 | 2.67 | 1.41 | 5.05 | 0.4 | 0.13 | 1.21 | |
| Gestational Diabetes | No | 41 | 300 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 17 | 26 | 4.78 | 2.39 | 9.58 | 6.3 | 2.02 | 19.68 | |
| Gestational Hypertension | No | 27 | 256 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 31 | 70 | 4.2 | 2.35 | 7.5 | 4.11 | 2.07 | 8.16 | |
Table 3: Factors associated with Neural Tube Defect (NTDs) among mothers who gave birth in public and private hospitals, Hargeisa, Somaliland
In this study of more than 36,400 births, the total prevalence for all types of NTDs was found to be 15.9 per 10,000 births. This finding is one of the lowest NTDs prevalence reported in Africa. It is lower than reports from Somali region and Tigray region in Ethiopia, Tanzania, Eritrea, Sudan and Cameroon (202.4 per 10,000, 131 per 10,000, 30.2 per 10,000, 39 per 10,000, 33.7 per 10,000 and 18.6 per 10,000), respectively [8-13]. Whereas, our findings are in line with similar study conducted in Egypt (16 per 10,000) [14]. Moreover, it’s higher than studies conducted in Congo (10.2 per 10,000) [15]; Malawi (6.3 per 10,000) [16]; and Nigeria (5.2 per 10,000) [17]. It is also higher than all European countries (EUROCAT) [18] and many Southeast Asian regions including Bangladesh (13.8 per 10,000) [19]; Nepal (11.9 per 10,000) [20]; and Thailand (6.3 per 10,000) [21]. These variations could be because of the study designs and studies setting i.e. some are community based while others are institution based.
Furthermore, folic acid supplementation was found to have a protective effect on NTDs (AOR: 0.43, 95% CI 0.25, 0.91). A similar conclusion was reached in a study conducted in Addis Ababa, Ethiopia (AOR, 0.47; 95%, 0.23–0.95) [22]. Together, the present finding enlightens the importance of preconception and during the first three months of conception of folic acid supplementation for prevention of NTDs, which is broadly in line with other studies worldwide too [23, 24].
Nevertheless, study conducted in North Shewa, Ethiopia revealed that there is association between medical illnesses like hypertension and diabetes with NTDs (OR = 2.72, 95% CI 1.94, 10.67), this result is consistent with our finding (AOR: 6.3, 95% CI 2.01, 19.67) and (AOR: 4.1, 95% CI 2.06, 8.15) respectively [25].
Nevertheless, it is also a point of interest to note that our study found that caffeine consumption is significantly associated with NTDs (AOR: 2.78, 95% CI 1.26, 6.09), which is supported other studies conducted in Amhara region, North Shewa and Harar in Ethiopia revealed that maternal caffeine consumption where associated with NTDs (AOR: 2.36, 95% CI: 1.15, 4.86, OR = 42.67, 95% CI = 9.8, 18.98 and AOR = 11.2; 95% CI: 3.1, 23.7), respectively [2, 25, 26]. The main sources of caffeine are coffee and tea. Numerous research findings indicate that coffee consumption during pregnancy may lead to miscarriages, reduce the absorption and metabolism of folate, and disrupt the mother's nutritional intake [27-30].
With regard to the maternal age, those with a maternal age of 28-32 have an increased risk of NTDs by 27% (AOR: 1.27, 95% CI 3.32, 4.21), for those whose ages are between 33-37 years increased the risk by 3.76 times (AOR: 3.76, 95% CI 1.05, 13.42) and the age group of 38-42 years increased with the risk of 9.1 times (AOR: 9.1, 95% CI 2.70, 30.57), which is contrary when compare to similar study conducted in Addis Ababa, Ethiopia which women in lower age are at most risk when compared to older ages, maternal age <19 (AOR 33.7 95% CI 2.53, 448.4) and maternal age 25–29 (AOR 9.7 95% CI 1.39, 67.6) [3]. This difference could be as a result of the sample size; the number of deliveries in the late reproductive age are fewer as compared to the youngest age.
When it comes to gestational age, gestational age at labor shows an association to neural tube defects which is in line with similar study conducted in Harar, Ethiopia [26]. Moreover, a similar study conducted in North Eastern Ethiopia to assess factors associated with neural tube defects found that mothers who took medication during pregnancy had nearly two times more likely to have a newborn with a neural tube defect than their counterparts (AOR 1.83 95% CI 1.08, 3.08), this result ties well with our findings (AOR: 2.05, 95% CI 1.07, 3.94) [4]. In addition, our study found that unidentified drug intake increases the risk of NTDs by 2.78 times (AOR: 2.78, 95% CI 1.26, 6.09), similar conclusion was reached by a study conducted in Addis Ababa and Amhara regions of Ethiopia where unidentified medication uses during early pregnancy (AOR = 4.595; 95% CI: 1.868-11.301) were associated with NTDs [31]. In Somaliland, Drugs with and without prescriptions are sold by pharmacies, clinics, and private drug salespeople. This implies that during the early stages of their pregnancy, mothers are likely to take over-the-counter medications which can increase their risk of congenital abnormal pregnancy outcome.
The findings of this study should be interpreted in the context of potential limitations. This study is a retrospective record review, and because of the nature of the study design, the overall prevalence may be underestimated. However, to prevent the incompleteness of the data, a randomly selected mother with a child having NTD and with normal delivery has been telephone interviewed. Moreover, this study is assumed to provide valuable baseline information to policymakers, researchers, and other stakeholders in the healthcare field.
The overall prevalence of neural tube defects (NTD) in Somaliland is relatively lower than in other countries in Africa. The most common types of neural tube defects found in the area were hydrocephalus and spinal bifida, respectively. The magnitude of NTDs increased with the mother's age. Maternal age, medication intake, consumption of caffeine, and metabolic diseases like gestational diabetes and gestational hypertension were positively associated with NTDs. However, delivery at full term and folic acid intake during pregnancy were found to have a protective association with NTDs. Hence, health care professionals should focus on maternal safe drug prescription and maternal folate intake and strengthen the existing system in terms of providing maternal health services before and during pregnancy. Since the aforementioned factors would be addressed during antenatal care, it is advised to increase pregnant mothers’ awareness regarding the timely initiation of antenatal care.
Ethical clearance was solicited from the office of research and ethical committee of the Edna Adan University Hospital (IRB No. 115/2024), and confirmation of permission to access the data from the archives was secured from these hospital directors. The patient charts were handled appropriately, guaranteeing that the survey's confidentiality was respected both during data extraction and when the charts were returned to the hospital's repository for storage. Moreover, verbal consent was obtained from the mothers for the telephone interview after explaining the risks and benefits of the survey.
We would like to express our gratitude to the three hospitals in Hargeisa, Somaliland, who volunteered to provide us with access to the delivery records and the registration books. We would also like to acknowledge the study participants who provided us with their detailed information.
The datasets used and/or evaluated in this study are available from the corresponding author upon reasonable request.
We, the authors, declare that we have no conflicts of interest.
ABK was responsible for the study concept, design, statistical analysis, and interpretation of the results. MAA and RAA acquired data from the records and interviews and participated in the data analysis and interpretation. MAA and RAA wrote the first draft of the manuscript. ABK: I critically reviewed the manuscript for intellectual content. All authors read and approved the final manuscript.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Ahmed MA, Abdilahi RA, Kahsay AB (2024). Magnitude and factors associated with Neural Tube Defects (NTDs) in Public and Private Hospitals. Hargeisa, Somaliland: A Three-Year Retrospective Study. J Women's Health Care. 13(4):720.
Received: 13-Mar-2024, Manuscript No. 30118; Editor assigned: 17-Mar-2024, Pre QC No. 30118; Reviewed: 29-Apr-2024, QC No. 30118; Revised: 08-Apr-2024, Manuscript No. 30118; Published: 15-Apr-2024 , DOI: 10.35248/2167-0420.24.13. 720
Copyright: © 2024 Ahmed MA, Abdilahi RA, Kahsay AB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited