Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Review Article - (2024)Volume 13, Issue 1
Objectives: Determine the frequency of ectopic pregnancy, specify the epidemiological and clinical profile of patients, describe paraclinical and therapeutic aspects, and assess maternal prognosis and factors associated with the type of ectopic pregnancy, treatment outcome and fertility after ectopic pregnancy.
Patients and methods: This was a retrospective, descriptive and analytical study conducted over a 31-month period (January 1, 2019 and July 31, 2021) and focused on the management of ectopic pregnancy at the Gynecology-Obstetrics Department of the IHS Hospital. We studied patients' socio-demographic characteristics, history, clinical and paraclinical data, therapeutic and prognostic aspects. Data were entered and analyzed using Excel 2010 and Epi info 7.2 software.
Results: We recorded 60 cases of EP in 5091 births, representing a frequency of 1.2% of deliveries. The epidemiological profile of the patients was that of a woman aged 29 years on average, nulliparous (40%), married (76.7%) and a housewife (68.3%). Functional signs were dominated by amenorrhea (100%), pelvic pain (80%) and metrorrhagia (65%). Hemodynamic status was stable, with cardiovascular collapse noted in 3 patients (5%). Abdominal palpation revealed abnormal sensitivity (55%) and a cry from the umbilicus (30%). Vaginal touch combined with abdominal palpation revealed a latero-uterine mass in 23.3% of cases. Plasma β-hCG assays were performed and found to be positive in 25 patients (41.7%), with levels mostly between 1,000 and 4,999 IU/L (20%). Blood counts revealed anemia in 17 patients (28.3%). Pelvic ultrasonography performed on all patients revealed direct signs of EP in 5 (8.3%). Indirect signs were dominated by uterine vacuity (80%), the existence of a latero-uterine mass (78.3%) and hemoperitoneum (73.3%). Fifty-three patients (88.3%) had undergone surgical treatment as first-line treatment, while the remaining 7 (11.7%) had undergone medical treatment with methotrexate. For the latter, we noted 4 cases of failure (57.3%), all of whom had undergone secondary surgery. Surgical procedures were dominated by total salpingectomy (96.5%). Short-term outcome was favorable (75%), with no maternal deaths. Fifteen patients (25%) had complications, dominated by anemia (16.7%). In the year following the EP, 7 pregnancies were recorded, representing a fertility rate of 11.7%. These resulted in 6 live births (10%) and one abortion (1.7%). No cases of recurrent EP were recorded. Ruptured EP was more frequent regardless of age (p=0.07) and parity (p=0.99). The outcome of medical treatment was more favorable the lower the serum β-hCG level (p=0.57) and the higher the dose used (p=0.001). More than a third of patients who had undergone primary surgery (36.8%) achieved pregnancy within a year of the EP, whereas this rate was nil in those who had received medical treatment (p=0.5).
Conclusion: Ectopic pregnancy is not uncommon in our practice. Despite the high proportion of ruptured ectopic pregnancies, which is the most frequent clinical form in our series, the maternal prognosis remains favorable thanks to well-codified, early and appropriate management.
Ectopic Pregnancy, Ultrasound, Salpingectomy, Fertility
Ectopic pregnancy (EP) is defined as the implantation and development of an egg outside the uterine cavity, most often in the fallopian tube [1]. It is a major surgical emergency and the leading cause of maternal mortality in the 1st trimester of pregnancy [2]. Its frequency is increasing in our practice, due to the resurgence of risk factors [1]. The maternity ward of the Institut d'Hygiène et Sociale hospital, which is a reference in the southern district of Dakar, has been involved for several years in the management of cases of ectopic pregnancy. Although few studies have been carried out in this field, we decided to carry out this study, the main aim of which was to evaluate our practice in the diagnosis and management of ectopic pregnancy. To achieve this objective, we sought to:
• Determine the frequency of EP.
• Define the epidemiological and clinical profile of patients presenting with EP.
• Describe the paraclinical and therapeutic aspects of EP.
• Assess the maternal prognosis.
Our study took place in the Maternity Hospital of the Institut d'Hygiène Sociale de Dakar (IHS), which has been a level 1 Public Health Establishment (EPS 1) since 2010.
We conducted a retrospective, descriptive and analytical study on the management of ectopic pregnancy over a 31-month period from January 1, 2019 to July 31, 2021.
We included all patients managed for ectopic pregnancy in the facility during the study period. We did not include in our study patients in whom a suspicion of EP was not confirmed. Data were collected from patients' medical records and from registers of operating protocols, the triage room and hospital wards. Additional information was collected by telephone. Analysis was performed using Excel 2010 and Epi info 7.2 software.
Descriptive Results
Frequency
During the study period, we recorded 60 cases of EP and 5091 deliveries, i.e. a frequency of 1.2% of deliveries or 1 EP per 85 deliveries. They were distributed as follows: 14 (23.3%) in 2019, 29 (48.3%) in 2020 and 17 (28.3%) in 2021 [Figure 1].
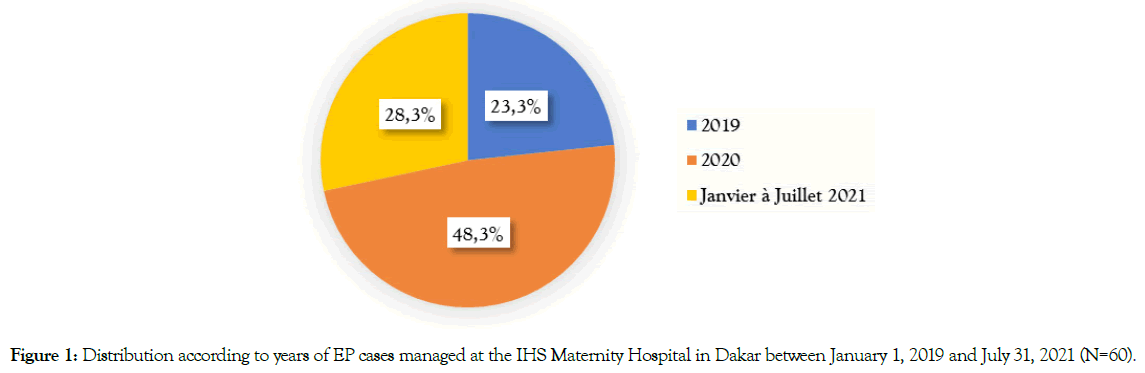
Figure 1. Distribution according to years of EP cases managed at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
Socio-demographic characteristics
Age
The mean age of the patients was 29 years, with extremes of 18 and 42 years. The 25-30 age group was the most represented (28.3%) [Figure 2].
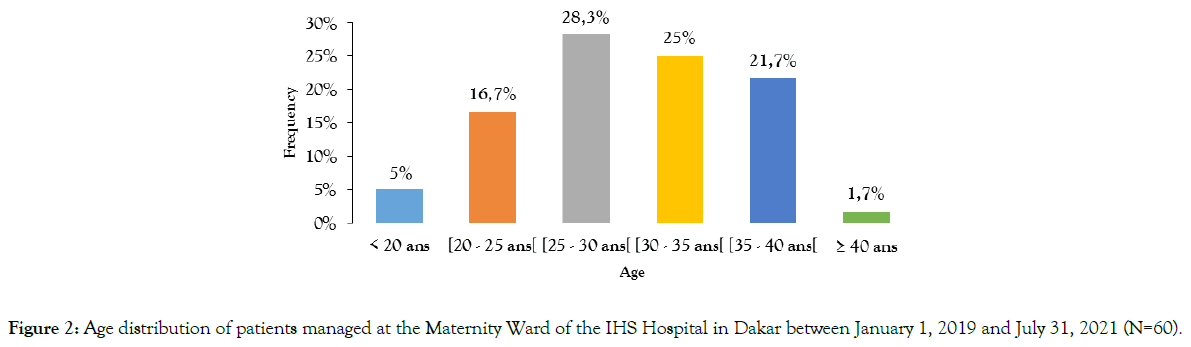
Figure 2. Age distribution of patients managed at the Maternity Ward of the IHS Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
Marital Status
In our series, most patients were married (76.7%). There were 9 single patients (15%).
Profession
Most patients were housewives (68.3%). Employees and shopkeepers represented 16.7% and 15% of our study sample respectively.
Clinical data on admission
Mode of admission
The majority of patients (65%) were evacuated to us. Twenty-one (35%) were self-referred.
Reasons for consultation
In our series, the reasons for consultation were dominated by amenorrhea (100%), sometimes associated with acute pelvic pain (80%) and/or metrorrhagia (65%) [Figure 3].
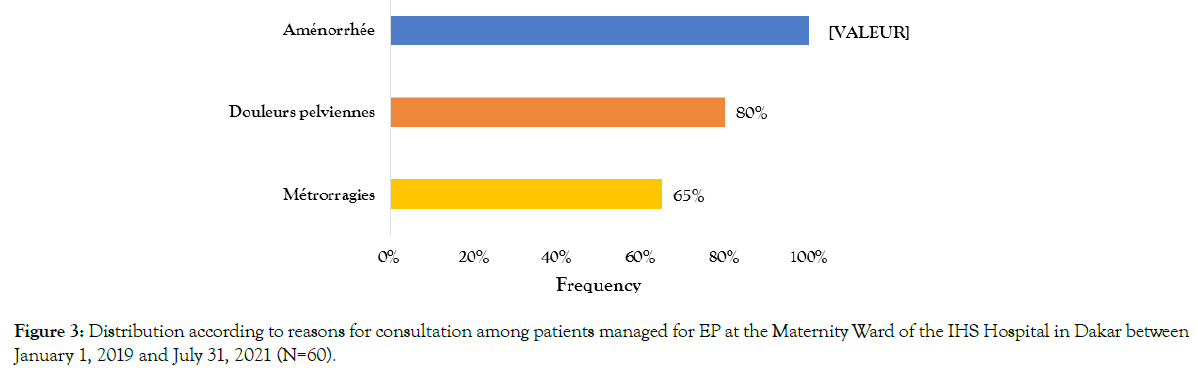
Figure 3. Distribution according to reasons for consultation among patients managed for EP at the Maternity Ward of the IHS Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
History
Gynecological history
In our series, the most frequent gynaecological antecedents were lower genital infection (53.3%), dysmenorrhoea (50%) and previous contraception (43.3%).
Among those with a history of contraception, the methods most frequently used were progestogen or oesoprogestogen pills (26.9%) [Figure 4].
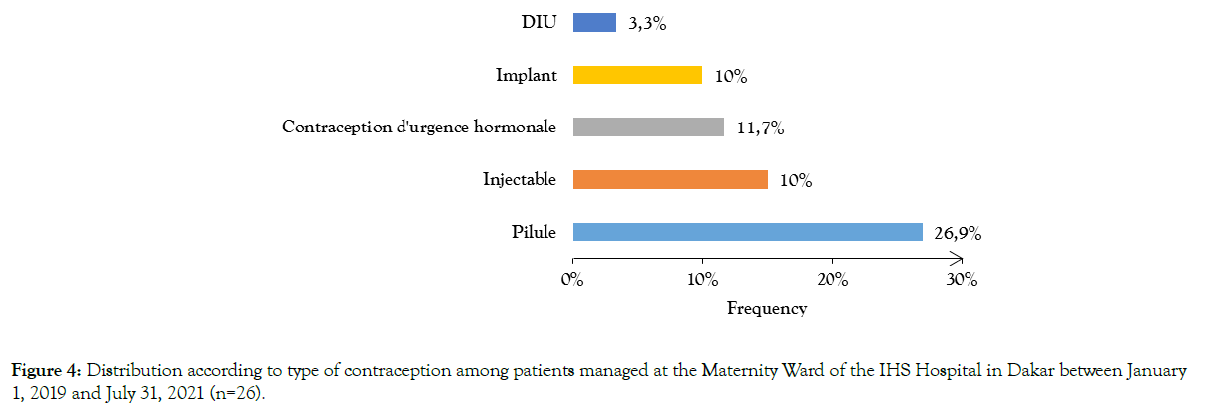
Figure 4. Distribution according to type of contraception among patients managed at the Maternity Ward of the IHS Hospital in Dakar between January 1, 2019 and July 31, 2021 (n=26).
Obstetrical history
In our series, most patients were nulliparous (40%). A history of abortion and EP was found in 35% and 5% of patients respectively [Table 1].
| Obstetrical History | Number (n) | Frequency (%) |
|---|---|---|
| Gestate | ||
| Primigestes | 18 | 30 |
| Paucigest | 35 | 58,3 |
| Multigest | 7 | 11,7 |
| Parity | ||
| Nulliparous | 24 | 40 |
| Primiparous | 14 | 23,3 |
| Pauparous | 19 | 31,7 |
| Multiparous | 3 | 5 |
| Abortion | ||
| None | 39 | 65 |
| 1 à 2 | 20 | 33,3 |
| 3 | 1 | 1,7 |
| History of EP | ||
| Yes | 3 | 5 |
| No | 57 | 95 |
| Caesarean section | ||
| Yes | 7 | 11,7 |
| No | 53 | 88,3 |
Table 1: Distribution according to obstetrical history of patients managed for EP at the Maternity Hospital IHS Dakar between January 1, 2019 and July 31, 2021 (N=60).
Clinical Examination Data
General examination
Most patients were in good general condition (91.7%). Cardiovascular shock was noted in 3 patients (5%).
Physical examination
Palpation of the abdomen revealed overall tenderness in 33 patients (55%), with a cry from the umbilicus in 18 (30%). Speculum examination results were mentioned in only seven cases (11.7%). In all cases, it confirmed the endo-uterine origin of the bleeding. The vaginal touch combined with abdominal palpation revealed a latero-uterine mass in 14 patients (23.3%) and a Douglas cry in 35 (58.3%) [Table 2].
| Physical Examination | Number (n) | Frequency (%) |
|---|---|---|
| Examination of the abdomen | ||
| Sensitive to palpation | 33 | 55 |
| Cry of the umbilicus | 18 | 30 |
| Speculum examination | ||
| Bleeding | 7 | 11,7 |
| Leucorrhoea | 1 | 1,7 |
| Inflamed cervix | 1 | 1,7 |
| Polyp | 1 | 1,7 |
| Vaginal touch | ||
| Latero-uterine mass | 14 | 23,3 |
| Douglas cry | 35 | 58,3 |
| Bleeding | 38 | 63,3 |
Table 2: Distribution according to physical examination findings in patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31 (N=60).
Paraclinical Data
Biology
The blood count showed anemia in 17 cases (28.3%). Urine and plasma β-hCG assays were performed in 19 (31.7%) and 25 (41.7%) patients respectively. Serum β-hCG levels were most frequently between 1000 and 4999 IU/L.
Pelvic ultrasound
In our series, all patients underwent pelvic ultrasonography. Direct signs of EP were found in 5 cases (8.3%). For the remainder of the sample (91.7%), indirect signs of EP were found. These included an empty uterus in 48 patients (80%), a latero-uterine mass (78.3%) or hemoperitoneum (73.3%). We also recorded 4 cases of heterotopic pregnancy (6.7%).
Therapeutic Data
The majority of patients (88.3%) had undergone surgical treatment in the first instance. Medical treatment concerned 7 patients (11.7%), of whom 3 were successful and 4 failed, necessitating secondary surgery [Table 3]. In addition, 3 patients (5%) underwent resuscitation.
| Type of Treatment | Number (n) | Frequency (%) |
|---|---|---|
| 1st-line surgical treatment | 53 | 88,3 |
| 1st line medical treatment | 7 | 11,7 |
| Surgical treatment after failure of medical treatment | 4 | 6,7 |
Table 3: Distribution according to the treatment used in patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
Modality of surgical treatment
All patients underwent laparotomy. The EP was predominantly located on the right (56.1%) and was most often ampullary (75.4%). We recorded 40 ruptured EPs (66.7%). Associated anomalies were dominated by pelvic adhesions (12.3%) and uterine fibroids (10.5%). Salpingectomy was the most frequently performed surgical procedure (96.5%) [Table 4].
| Surgery Procedures | Number (n) | Frequency (%) |
|---|---|---|
| Approach | ||
| Pfannenstiel | 44 | 77,2 |
| Joel Cohen | 7 | 12,2 |
| Not specified | 6 | 10,5 |
| Topography of the EP | ||
| Ampullary | 43 | 75,4 |
| Cornual | 4 | 7 |
| Interstitiel | 2 | 3,5 |
| Infundibular | 4 | 7 |
| Isthmic | 2 | 3,5 |
| Ovarian | 2 | 3,5 |
| Associated pathologies | ||
| Adhesions | 7 | 12,2 |
| Uterine fibroid | 6 | 10,5 |
| Ovarian cyst | 5 | 8,7 |
| Annexes | ||
| Ruptured tubal pregnancy | 40 | 70,2 |
| Unruptured tubal pregnancy | 18 | 31,5 |
| Unruptured ovarian pregnancy | 2 | 3,5 |
| Contralateral pathological adnexa | 3 | 5,2 |
| Surgical procedure | ||
| Total salpingectomy | 55 | 96,5 |
| Ovariectomy | 2 | 3,5 |
Table 4: Distribution by modality of surgical treatment indicated in patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (n=57).
Medical treatment
Medical treatment with methotrexate was carried out in 7 patients (11.7%). This was most often a single intramuscular injection (57.1%). We recorded 3 successes (42.8%) and 4 failures (57.1%).
Prognosis in short-term outcome
Forty-five patients (75%) had a favorable outcome. Fifteen (25%) presented a complication. The most frequent complication was anemia (16.7%).
Post-treatment follow-up
Chlamydia and mycoplasma antibodies were tested in 20 patients (33.3%), and were positive in three (15%). Hysterosalpingography was carried out in only 7 patients (11.7%), in all of whom the contralateral tube was found to be permeable.
Fertility Prognosis
Twenty-six patients (43.3%) had regular follow-up up to one year after the EP. During this follow-up, 7 pregnancies were recorded, representing a fertility rate of 26.9%. Their progress was marked by 6 full-term deliveries (85.7%) and one abortion (14.3%) [Table 5].
| Fertility 1 year after EP | Number (n) | Frequency (%) |
|---|---|---|
| Live birth | 6 | 10 |
| Abortion | 1 | 1,7 |
| Absence of pregnancy | 19 | 31 |
| Lost to follow-up | 34 | 56,7 |
| Total | 60 | 100 |
Table 5: Distribution of patients according to fertility at 1 year in patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (n=60).
Analytical Results
Age by type of EP
In our series, ruptured EPs were more frequent in all age groups, except in the 35-40 age group, where we recorded 69.2% unruptured EPs. However, there was no statistically significant relationship between age and type of EP (p=0.07).
Parity according to type of EP
In our series, ruptured EP was more frequent whatever the patient's parity. Indeed, we recorded rates of 66.7%, 64.3%, 68.4% and 66.7% of ruptured EP respectively in nulliparous, primiparous, multiparous and large multiparous women, with no statistically significant relationship between parity and type of EP (p=0.99).
Outcome of medical treatment according to serum β-hCG level
In our series, the outcome of medical treatment was more favorable the lower the serum β-hCG level. In fact, for all patients with a serum β-hCG level below 1000 IU/L, medical treatment was successful, whereas above this level, failure was observed [Table 6].
| Successful Medical Treatment | Total | |||
|---|---|---|---|---|
| Level of β-Hcg | Yes | No | P | |
| <1000 UI/L | 3 (100%) | - | 3 | 0,57 |
| 1000 à 2499 UI/L | - | 1 (25%) | 1 | |
| 2500 à 5000 UI/L | - | 3 (75%) | 3 | |
| Total | 3 | 4 | 7 | |
Table 6: Outcome of medical treatment according to serum β-hCG level of patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
Fertility at one year according to type of treatment
In our series, 26 patients benefited from regular follow-up up to one year after EP. More than a third of patients who had undergone primary surgery (36.8%) achieved pregnancy within a year of the EP, whereas this rate was nil in those who had received medical treatment. However, there was no statistically significant relationship between the type of treatment and fertility one year after the EP (p=0.5) [Table 7].
| Fertility after EP | ||||||
|---|---|---|---|---|---|---|
| Type of treatment | Pregnancy achieved | No Pregnancy | Total | |||
| N | % | N | % | P | ||
| Primary surgery | 7 | 36,8 | 12 | 63,2 | 19 | 0,5 |
| Medical treatment | - | - | 3 | 100 | 3 | |
| Surgery after medical treatment | - | - | 4 | 100 | 4 | |
| Total | 7 | 19 | 26 | |||
Table 7: Fertility at one year according to type of treatment in patients managed for EP at the IHS Maternity Hospital in Dakar between January 1, 2019 and July 31, 2021 (N=60).
Frequency
The prevalence of EP varies from one author to another. According to the literature, it varies between 1% and 2% [3]. The frequency of 1.2% of deliveries found in our series is comparable with the literature. Indeed, [4] in Senegal, [1] in N'Djaména and [5] in Madagascar found EP frequencies of 1%, 2.4% and 2.3% respectively. The same trend can be observed in France, where the rate of EP is 1.6% [3], and in Germany, where the incidence is 1% according to a recent study [6]. However, in some sub-Saharan African countries, the incidence is higher, sometimes reaching 4% [1]. This increase in the frequency of EP in certain countries could be explained by the resurgence of sexually transmitted infections, which used to be the main risk factor.
Epidemiological Profile
In our series, the epidemiological profile of patients was that of a woman with an average age of 29 years, nulliparous (40%), married (76.7%) and a housewife (68.3%). This profile is comparable to those found in the literature. Indeed, [7] in Senegal and [8] in Cameroon found the same average age in their respective studies. [9] recorded a lower average age of around 26 years.
The age group most concerned in our series was between 25 and 30 (28.3%). The same observation was made by [1] in Chad and [3] in Niger, with a predominance of the 25-29 (34.6%) and 25-34 (67.8%) age groups in their respective series. This may be explained by the fact that this age group coincides with the period of genital activity when women are most sexually active.
EP is often associated with low parity, as we found in our series. [11] In Dakar and [12] in Morocco also found a predominance of nulliparous women in their series, with frequencies of 45.5% and 17.7% respectively. Some authors, such as [10] and [7], recognize low parity, and in particular pauciparity, as a factor predisposing to EP. A German study also incriminated pauparity [13]. In our series, EP was associated with other risk factors, in particular a history of lower genital infection (53.3%), use of the progestin-only pill (26.9%) and EP (5%). [10] and [4] reported lower genital infection rates of 18.9% and 16% respectively. Some cases of vulvovaginitis carry the risk of complications such as salpingitis, which can lead to tubal sequelae, notably complete or incomplete obstruction, exposing the woman to EP. The literature shows that repeated infection with chlamydia trachomatis increases the risk of EP [14]. With regard to the use of progestin-only contraception, [5] and [10] found it to be less common in their patients than in ours, with proportions of 12.1% and 13.3% respectively. [8] in Cameroon, [15] in Benin and [16] in Gabon reported rates of 5.9%, 7.3% and 16.3% respectively of previous EP.
Clinical and Paraclinical Data
In our series, the reasons for consultation were dominated by amenorrhea (100%), pelvic pain (80%) and metrorrhagia (65%). This is the symptomatic triad classically found in EP. [4] and [15] reported 95% and 77.4% amenorrhea respectively. As for pelvic pain, slightly higher rates were recorded by [12], [1] and [10], with 90%, 94, 2% and 100% lateralized pelvic pain respectively. This symptom may indicate tubal distension by the hematosalpinx, but it should also suggest a probable rupture of the EP. In our series, metrorrhagia was the 3rd most frequent reason for consultation. In their respective studies, [11] and [10] found higher rates in the order of 70.4% and 80.4%. In contrast, [8] and [16] found a lower frequency of metrorrhagia, at 31.3% and 66.7% respectively. This variability in the functional signs of EP between authors confirms the clinical polymorphism noted for this pathology, and explains the difficulty in making the diagnosis. In our study, most patients (91.7%) were hemodynamically stable. This rate is slightly higher than those recorded by [12] and [1], which were 73% and 80.7% respectively, which contrasts with the predominance of ruptured EPs in our study. This is probably due to the early stage of diagnosis, when the patient's general condition is still intact. In our series, physical examination often revealed abdominal tenderness (55%), sometimes associated with a cry from the umbilicus (30%). [11] made the same finding in his work, with 52.5% of patients presenting with abdominal tenderness. On the other hand, [10] and [5] recorded rates higher than ours, with values of 62.3% and 96.3% respectively. The variable frequency of abdominal tenderness in different studies is certainly linked to the subjectivity of this data. A latero-uterine mass was found in almost a quarter of our patients (23.3%), a low proportion compared with that recorded by [11], which was 35.7%. In his study, [8] reported adnexal impaction in 97.7% of patients. Perception of the laterouterine mass in EP may be hampered by tenderness, defensiveness and/or contracture of the abdomen, especially in cases of ruptured EP. This could explain the low rate we found in our patients, especially as the EP was ruptured in 66.7% of cases.
With regard to complementary examinations, plasma β-hCG assays were carried out in 25 patients (41.7%). The same observation was made by [10] in Niger, who reported a frequency of 44% corresponding to the number of patients with a positive β-hCG assay. On the other hand, [11] in Senegal found a frequency of 92%. This proves that a plasma β-hCG assay is not essential for the diagnosis of EP.
In our series, normocytic normochromic anemia was noted in 28.3% of patients. [4] and [11] reported 60% and 68.2% anemia respectively. This is a frequent complication of EP, especially in our developing countries, where diagnosis is often delayed until the rupture stage. In our study, 5 patients (8.3%) showed direct signs of EP on ultrasound, while most had indirect signs: uterine vacuity (80%), latero-uterine mass (78.3%) and hemoperitoneum (73.3%). In [10], direct ultrasonographic signs of EP were found in 16.9% of cases. This finding may be explained by the fact that ruptured EP, which is the most frequent clinical form in our practice, is characterized by the presence of hemoperitoneum on ultrasound. Ultrasound should always be the first line of defence in cases of suspected EP, as it enables early diagnosis of EP, pinpointing its location in over 73.9% of cases [3]. The discovery of an EP does not exclude its association with an intrauterine pregnancy. In our series, we recorded 4 cases of heterotopic pregnancy (6.7%). In their respective series, [4] and [17] found one and seven cases of heterotopic pregnancy. This is a rare clinical situation, but one that should always be considered in cases of EP. Indeed, failure to recognize an associated UGI could compromise its prognosis.
Therapeutic Aspects
In our study, 95% of patients had undergone surgical treatment by laparotomy. The same observation was made in the studies by [10] and [4]. The latter reported 87.4% and 79.5% surgical treatment respectively and laparotomy was the approach used in all cases. This predominance of surgery in our patients may be due to the much higher frequency of ruptured EP, which represents a contraindication to medical treatment. The laparotomy approach could also be explained by the same reason, but also by the unavailability of laparoscopy, which is the reference approach for surgical treatment of unruptured EP. Ruptured EP concerned 66.7% of patients in our study. This rate is comparable to that of [16] in Gabon, who found 75% tubal rupture. Radical surgical treatment by salpingectomy was observed in 96.5% of patients in our series. [11], [9] and [13] made the same observation, with 92.1%, 63.7% and 66.7% of salpingectomy in their respective series. This is explained by the frequency of tubal rupture, which often makes preservation impossible and salpingectomy necessary to ensure haemostasis. On the other hand, in industrialized countries, where EP is diagnosed earlier, conservative treatment is more common. Indeed, [6] in Germany reported a 97.3% rate of salpingotomy and 2% of salpingectomy in his study. Medical treatment was carried out in 7 patients (11.7%), with a success rate of 42.8%. (1, 3%). On the other hand, in a study carried out in Senegal, [11] reported 20.4% medical treatment. This variability in the frequency of medical treatment noted in the literature could be explained by the difficulties encountered in patient follow-up, notably the risk of being lost to follow-up, but also the high cost of medical treatment compared with surgery. In France, [18] based on the Auvergne register, recorded a success rate for medical treatment of between 65% and 95%. This may be explained by early diagnosis, but also by the availability and accessibility of monitoring resources.
Maternal prognosis and subsequent fertility
In our study, no maternal deaths were recorded. The same observation was made by [11]. On the other hand, [1] reported one maternal death, i.e. a case-fatality rate of 1.9%. It is only in the United States that the mortality of EP has been the subject of precise studies. The mortality rate fell from 1.4 to 0.8 per thousand EP, while the frequency of EP doubled [2]. However, mortality is 3.2 times higher in black women for a frequency 1.6 times higher [2].
In our series, the pregnancy rate one year after EP was 11.7%. These resulted in 6 live births (10%) and one abortion (1.7%). Reported a lower rate of around 7.8%. Of the fifty or so studies selected, pregnancy rates after EP are satisfactory (60%), whatever the mode of treatment, with the ideal surgical approach being laparoscopy. Recurrence rates are around 28% [19]. [7] and [16] reported recurrence rates of 8% and 2% respectively. In our series, we observed no cases of recurrence. This is probably due to the short follow-up period of only one year.
Ectopic pregnancy is a major surgical emergency, threatening the patient's vital prognosis through hemorrhagic shock. Our study was characterized by a better vital prognosis, but a relatively short time to assess fertility after treatment. It is necessary to act on STI risk factors, and to perform pelvic ultrasound for diagnosis.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: SAMB F, Niang MM, Owane DRM, Cisse CAT (2024) Management of extra-uterine pregnancy at the gynecology-obstetrical department of the Dakar social hygiene institute: about 60 cases collected between January 1, 2019 and July 31, 2021. 13(1):706.
Received: 26-Dec-2023, Manuscript No. JWH-23-28651; Editor assigned: 29-Dec-2023, Pre QC No. JWH-23-28651; Reviewed: 12-Jan-2024, QC No. JWH-23-28651; Revised: 16-Jan-2024, Manuscript No. JWH-23-28651; Published: 23-Jan-2024 , DOI: 10.35248/2167- 0420.24.13.706
Copyright: © 2024 SAMB F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited