
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Research Article - (2024)Volume 14, Issue 4
Introduction: The intervention effect of lifestyle combined with metformin on pre diabetes population in Asia is still unclear. This meta-analysis aims to analyze and evaluate the prevention effect of joint intervention on pre diabetes population in Asia.
Materials and methods: The search strategy was developed according to the PICOS principle, searching in databases such as PubMed, The Cochrane Library, Web of Science, and Embase until October 9, 2023. RCTs in adults with prediabetes, interventions lasting ≥ 1 year. And the outcome indicator was the incidence of diabetes. Relative Risk (RR) was used as the statistical effect size, with interval estimation using a 95% Confidence Interval (CI).
Results: Of 4 studies included in the systematic review, involving 2682 subjects, with 1314 in the experimental group. The results showed that, compared to lifestyle intervention alone, the addition of metformin to lifestyle intervention could further reduce the risk of progression to T2DM by about 17% (95% CI: 7-26, p=0.001) in Asian prediabetes patients.
Conclusions: In Asian prediabetes population, lifestyle intervention combined with metformin can further reduce the risk of diabetes in prediabetes patients compared with lifestyle intervention alone, especially in male patients with abnormal glucose tolerance whose age is less than 45 years old, BMI>25 kg/m2, and HbA1c ≤ 5.6%, which can reduce by 17%, and the effect is positively related to the dose of metformin and the intervention time.
Metformin; Diabetes; Pre-diabetes; Glucose tolerance; BMI
With the rising incidence rate of obesity and type 2 diabetes, more and more patients face the risk of macrovascular and microvascular complications, which severely impact their quality of life and also impose a substantial economic burden. Pre Diabetic (PD) patients are considered a reserve force for diabetes. According to data from the International Diabetes Federation (IDF), the number of adults with PD worldwide is rising annually [1].
The American Diabetes Association (ADA) proposed that targeted intervention measures can effectively delay the progression of diabetes in high-risk populations. The intervention includes lifestyle adjustment such as healthy meals, increased physical exercise, and weight reduction. Although the benefits of lifestyle intervention, but long-term adherence to this intervention remains a challenge for many individuals, leading to diminishing benefits and potential advantages. Therefore, it is necessary to add other treatment methods. ADA has listed metformin combine with lifestyle intervention as a grade A recommendation for primary prevention [2].
In Asia, especially in regions like China and India, pre diabetic patients account for 60% of the proportion. The effect of lifestyle intervention combine with metformin are not clear. Therefore, this meta-analysis will help us to analyze and evaluate the prevention effect of joint intervention on pre diabetes population in Asia.
Inclusion and exclusion criteria
Inclusion criteria:
• Prediabetic populations aged 18 years, regardless of gender, age, ethnicity, etc.
• The intervention group received lifestyle changes plus metformin, with no restrictions on metformin formulation, dosage, or course of treatment; the control group received only lifestyle intervention or combined with placebo treatment.
• The outcome indicator was the incidence of diabetes.
• Included studies were Randomized Controlled Trials (RCT).
• The study duration was 1 year, and the literature was in English.
Exclusion criteria:
• Total sample size <100 cases.
• Reviews, meta-analyses, case reports, conference abstracts, animal experiments, etc.
• Did not provide relevant outcome indicators.
• Unable to obtain full text data or incomplete data.
• The presence of other incomparable confounding factors.
Literature search strategy
The protocol of this review was registered in PROSPERO (ID: CRD42024558676). The search strategy was developed according to the PICOS principle, searching in databases such as PubMed, The Cochrane Library, Web of Science, and Embase until October 9, 2023. Manual searches were also conducted to comprehensively retrieve related literature.
Search terms included three parts: Lifestyle intervention, metformin, and PD, using a combination of subject words and free words with Boolean logic operators [3].
Literature screening and data extraction
Two researchers independently conducted literature searches according to the retrieval strategy, imported the searched literature into EndNote X9 software, organized the literature, removed duplicate literature, exclude articles that do not meet the inclusion criteria by reading the article title, abstract, full text, etc. Crosschecked to determine the included studies, and extracted data including general information about the study (study title, publication year, sample size, follow-up time, PD diagnostic criteria, intervention measures, etc.), basic characteristics of the included participants (age, gender, weight, BMI, HbA1c level), and study results (number of people developing type 2 diabetes).
Disputes in the above process were resolved through discussion and negotiation; if resolution was still not possible, a third party was involved. For data that could not be obtained, authors might be contacted.
Quality assessment
Quality assessment was independently conducted by two researchers using the Cochrane randomized controlled trial bias risk assessment tool RoB2.
Statistical methods
Meta-analysis was performed using Review Manager 5.3 software. Heterogeneity of the included study results was analyzed using the I² test. When p>0.05, I²<50%, suggesting less heterogeneity, a fixed-effect model was used for meta-analysis. Conversely, it indicated greater heterogeneity, and a random-effects model was used for meta-analysis, with further analysis to identify sources of heterogeneity.
Subgroup analysis was applied to handle heterogeneity, grouped by gender, age, race, etc., to eliminate confounding factors, analyzing heterogeneity among the included study results and also enabling a comprehensive analysis of the included data. Funnel plots were used to assess publication bias.
The outcome indicator was the incidence rate of diabetes, a binary variable, thus Relative Risk (RR) was used as the statistical effect size, with interval estimation using a 95% Confidence Interval (CI). When the effect size <1, 95% CI did not include 1, p<0.05, indicating that the lifestyle combined with metformin intervention group had a better therapeutic effect on PD patients than the control group, with a statistically significant difference. Conversely, the intervention group had no significant advantage over the control group in treating PD [4].
Literature search process and results
According to the search strategy, a total of 2771 documents were retrieved. After removing 673 duplicate documents, 2098 remained. After reading titles and abstracts, 20 documents proceeded to fulltext reading. Excluding non-RCTs, controls that did not match, experimental indicators that did not match, and those where the full text could not be obtained left 4 documents for meta-analysis, including 2 from India [5,6-8], one from China [9], and one from Pakistan [10]. Figure 1, show the details on the screening process.
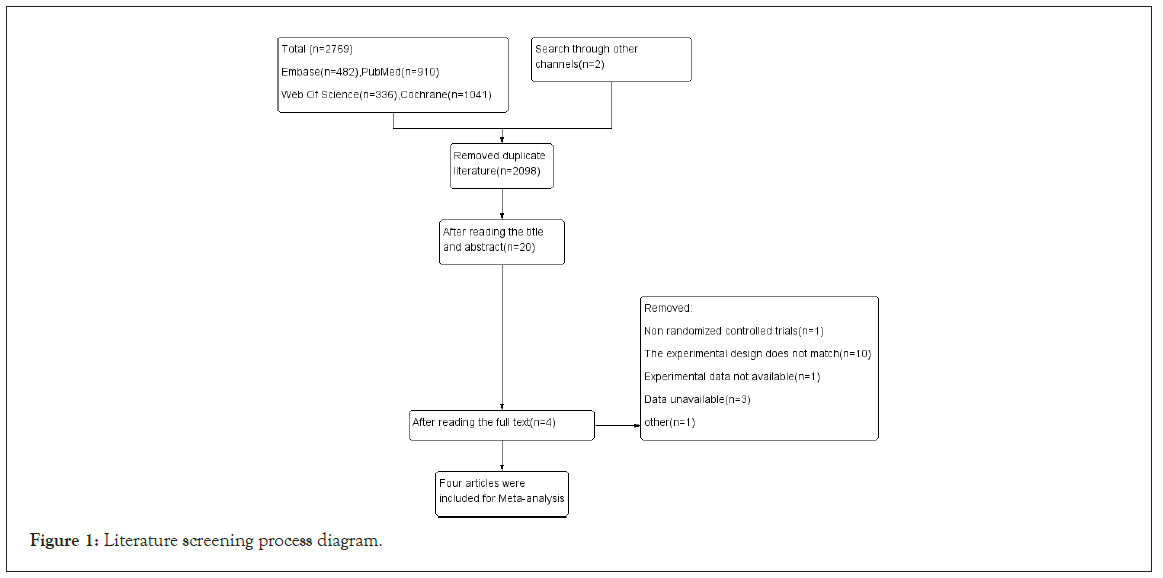
Figure 1: Literature screening process diagram.
Basic characteristics of included studies
The study included 4 articles, involving 2682 subjects, with 1314 in the experimental group. The basic characteristics of the included studies are shown in Table 1. The publication years of the included literature ranged from 2006 to 2023, with an average follow-up time ranging from 1.5 to 3 years. The sample size ranged from 371 to 1678 people, mostly aged 40-60 years. All four studies applied the WHO's diagnostic criteria for PD. Among the various groups of the included studies, over 50% had a family history of diabetes.
| Author, country, year | Duration (years) | Participants type | N | Intervention | Male (N) | Age (years) | BMI (kg/m2) | HbAlc (%) |
|---|---|---|---|---|---|---|---|---|
| Ramachanderan A, India, 2006 | 2.6 | IGI | 531 | Control | 104 | 45.2 ± 5.7 | 26.3 ± 3.7 | 6.2 ± 0.5 |
| Lifestyle | 104 | 46.l ± 5.7 | 25.7 ± 3.3 | 6.1 ± 0.5 | ||||
| Metformin | 107 | 45.9 ± 5.9 | 25.6 ± 3.7 | 6.2 ± 0.6 | ||||
| Combine | 105 | 46.3 ± 5.7 | 25.6 ± 3.3 | 6.2 ± 0.6 | ||||
| Weber M, India, 2016 | 3 | IFG | 576 | Lifestyle | 183 | 44.0 (9.5) | 27.8 (3.7) | 6.0 (0.5) |
| IGT | Combine | 181 | 44.5 (9.0) | 27.9 (3.7) | 6.0 (0.5) | |||
| Zhang L, China, 2023 | 2.03 | IFG | 1678 | Lifestyle | 397 | 53 (45-55) | 26.28 (2.81) | 5.90 (0.41) |
| IGT | Combine | 396 | 53 (45-59) | 26.27 (2.8b) | 5.86 (0.44) | |||
| lqbal Hydrie MZ, Pakistan, 2012 | 1.5 | 1GT | 317 | Control | NA | 44.2 ± 10.9 | 27.0 ± 5.7 | NA |
| Lifestyle | NA | 43.l ± 10.1 | 26.1 ± 4.7 | NA | ||||
| Combine | NA | 43.5 ± 8.4 | 28. I ± 4.3 | NA |
Note: IFG: Impaired Fasting Glucose; IGT: Impaired Glucose Tolerance.
Table 1: Characteristics of studies included.
Quality assessment of included studies
All four documents included in the analysis were RCT studies, assessed for quality using the Cochrane randomized controlled trial bias risk assessment tool RoB2. All studies employed randomized grouping with no obvious bias in the randomization process. During the experiment, there were instances of participants deviating from the intended interventions, but the number of deviations in both the control and intervention groups was comparable, with similar reasons, and far less than the number of diabetes cases, insufficient to cause a clinically significant impact on the experimental intervention results. The intention-to-treat analysis method was applied; all studies reported complete data. Since the experimental intervention was evident, none of the studies included in the analysis adopted blinding, posing a high risk, but the experimental results were evaluated using a unified standard and were laboratory indicators, thus comparable among studies. See Figures 2 and 3, for the quality assessment of the included studies.
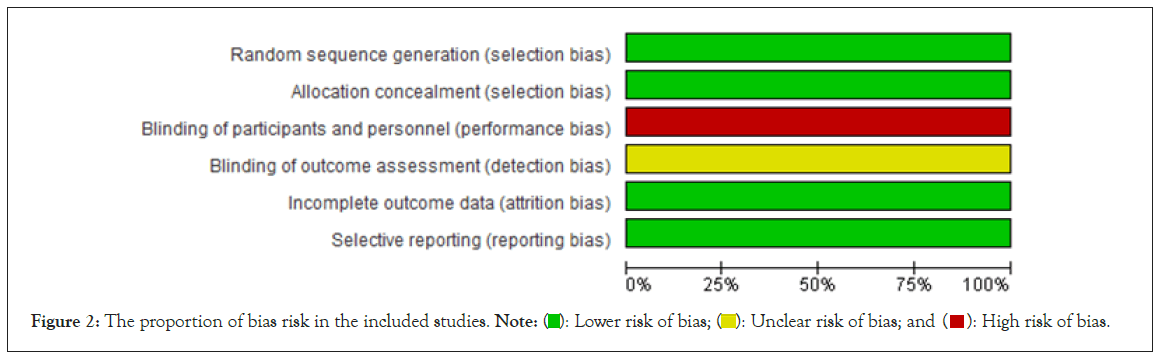
Figure 2: The proportion of bias risk in the included studies. Note:  : Lower risk of bias;
: Lower risk of bias;  : Unclear risk of bias; and
: Unclear risk of bias; and  : High risk of bias.
: High risk of bias.
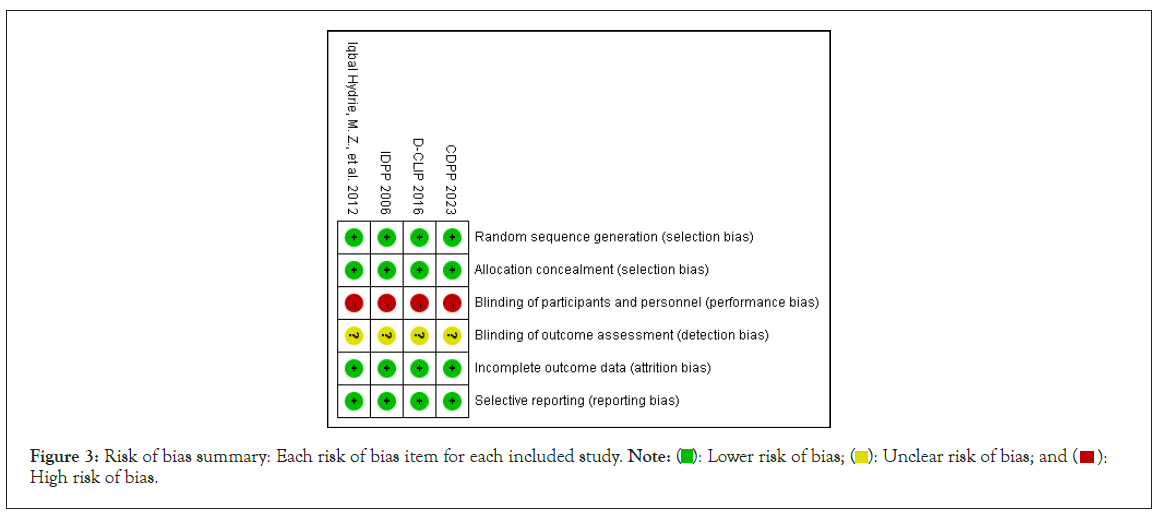
Figure 3: Risk of bias summary: Each risk of bias item for each included study. Note:  : Lower risk of bias;
: Lower risk of bias;  : Unclear risk of bias; and
: Unclear risk of bias; and  : High risk of bias.
: High risk of bias.
Meta-analysis results
Incidence of diabetes: In the included studies, participants were from Asian prediabetic populations [5,8-10]. The studies compared the control group (only lifestyle intervention) with the experimental group (lifestyle combined with metformin intervention) in terms of diabetes prevention effects. There was no heterogeneity between the results of each study; a fixed-effect model was used for meta- analysis. The results showed that compared to lifestyle intervention alone, lifestyle combined with metformin intervention could further reduce the risk of diabetes onset by about 17% (95% CI: 7-26). The difference was statistically significant (p=0.001) (Figure 4).
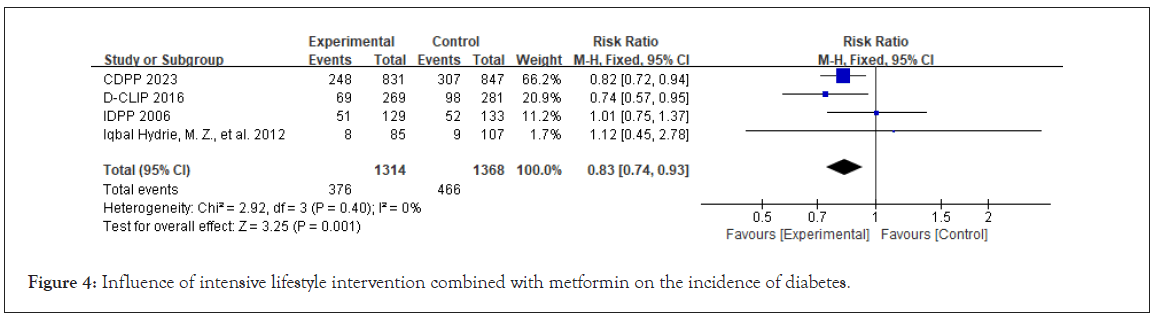
Figure 4: Influence of intensive lifestyle intervention combined with metformin on the incidence of diabetes.
Publication bias
Funnel plots were used to analyze publication bias regarding the results of diabetes incidence rates included in the studies. As shown in Figure 5, the points included in the studies were distributed roughly symmetrically on both sides of the top midline, evenly. The risk of publication bias in the results included in the studies was small.
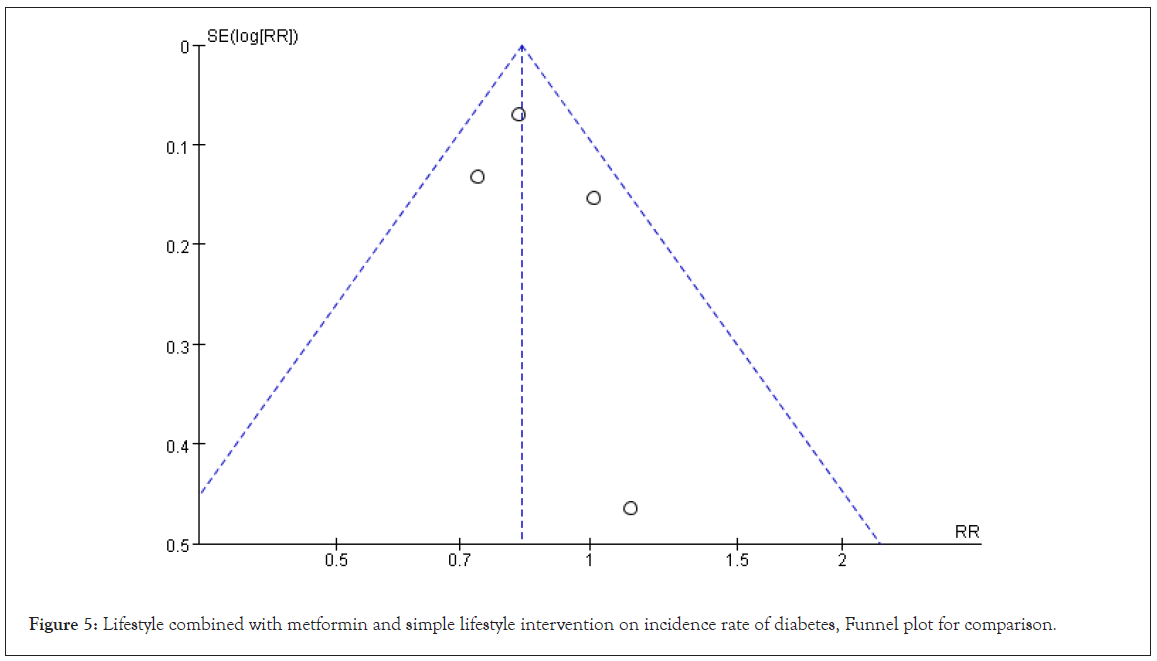
Figure 5: Lifestyle combined with metformin and simple lifestyle intervention on incidence rate of diabetes, Funnel plot for comparison.
Subgroup analysis
All four studies included in this meta-analysis were randomized controlled trials that met the set inclusion and exclusion criteria. An assessment of the risk of publication bias was conducted, observing that the funnel plot results showed this risk to be relatively small. It can be considered that the quality of the included literature is reliable, and the analysis results have high credibility. Meanwhile, this Meta-analysis used subgroup analysis to compare the effects of different intervention methods on diabetes prevention in Asian prediabetic patients with different characteristics.
The subgroup analysis results are shown below. According to the metformin dosages in the included trials, they were divided into 1000 mg/d and >1000 mg/d. The results are shown in Figure 6; all included studies used intensive lifestyle interventions, with little heterogeneity among the study results. The results showed that lifestyle with a larger dose of metformin (>1000 mg/d) could further reduce the risk of diabetes onset (RR=0.82, 95% CI: 0.72- 0.94, p=0.006; vs. RR=0.85, 95% CI: 0.70-1.03, p=0.09). In the subgroup of age, the results indicated that in PD patients younger than 45 years old, lifestyle combined with metformin intervention could further reduce the risk of diabetes onset compared to lifestyle intervention alone, with an RR value of 0.69 (95% CI: 0.53-0.90, p=0.007) (Figure 7A). In patients of different sexes, the results showed that lifestyle combined with metformin intervention had a better effect on diabetes prevention for men, further reducing the risk of diabetes onset (RR=0.73,95% CI: 0.61-0.88, p=0.0008) (Figure 7B). According to WHO BMI classification, divided into two groups at 25 kg/m². The results are shown in Figure 7C; lifestyle intervention combined with metformin intervention had a better effect on diabetes prevention in patients with BMI>25 kg/ m², with an RR value of 0.74 (95% CI: 0.63-0.86, p=0.0001).
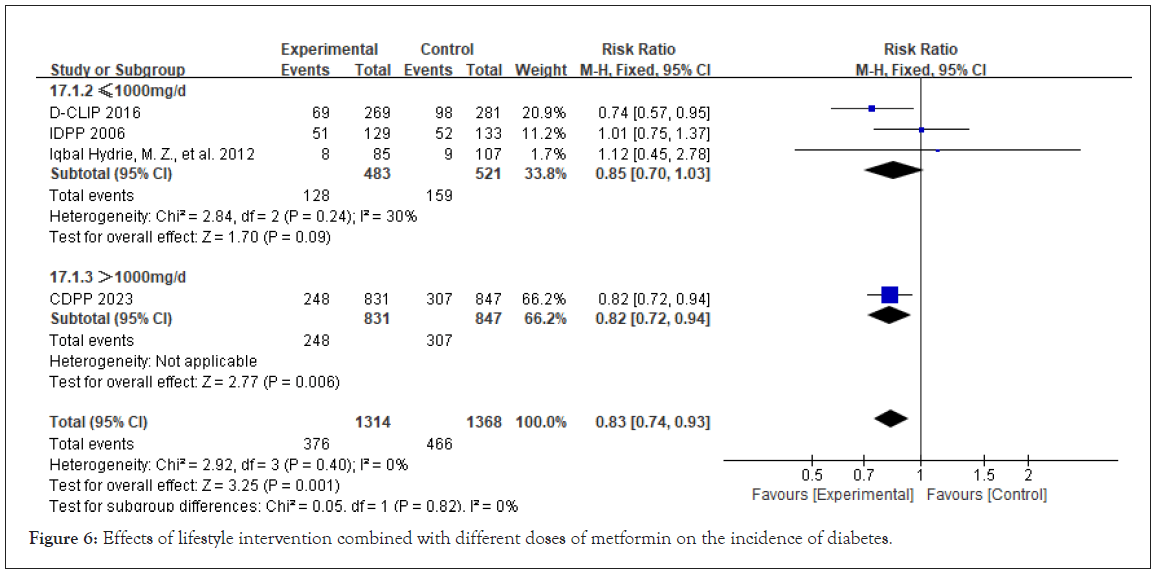
Figure 6: Effects of lifestyle intervention combined with different doses of metformin on the incidence of diabetes.
For the effect of intervention measures in different HbA1c groups are shown in Figure 7D. According to the ADA definition of diabetes in the early stage, with the HbA1c value of 5.6% as the boundary, they are divided into two groups. There is no obvious heterogeneity between the experimental results. Meta-analysis using fixed effect model shows that in patients with HbA1c ≤ 5.6% PD, lifestyle combined with metformin can further reduce the risk of diabetes by about 30% compared with simple lifestyle (95% CI: 1-51, p=0.04).In patients with HbA1c>5.6% PD, lifestyle combined with metformin intervention is more effective than the simple lifestyle intervention can further reduce the incidence rate of diabetes by about 13% (95% CI: 1-24, p=0.04).
PD includes IFG and IGT. The pathogenesis of each type is different, so different types of subgroup analysis is conducted to evaluate the effect of primary prevention of diabetes in patients with different types of PD. Figure 7E, indicate that compared with lifestyle intervention alone, lifestyle combined with metformin has better primary prevention of diabetes in IGT population, with a RR value of 0.82 (95% CI: 0.69-0.98), and the difference is statistically significant (p=0.03). To clarify the impact of the intervention time on the incidence rate of diabetes, the included studies were grouped according to the length of the intervention time. The results were as shown in Figure 8. In the subgroup with a follow-up time of 2 years, the lifestyle combined with metformin could effectively prevent the occurrence of diabetes and further reduce the risk of diabetes by 17% compared with the simple lifestyle (95% CI: 8-26, p=0.0009).
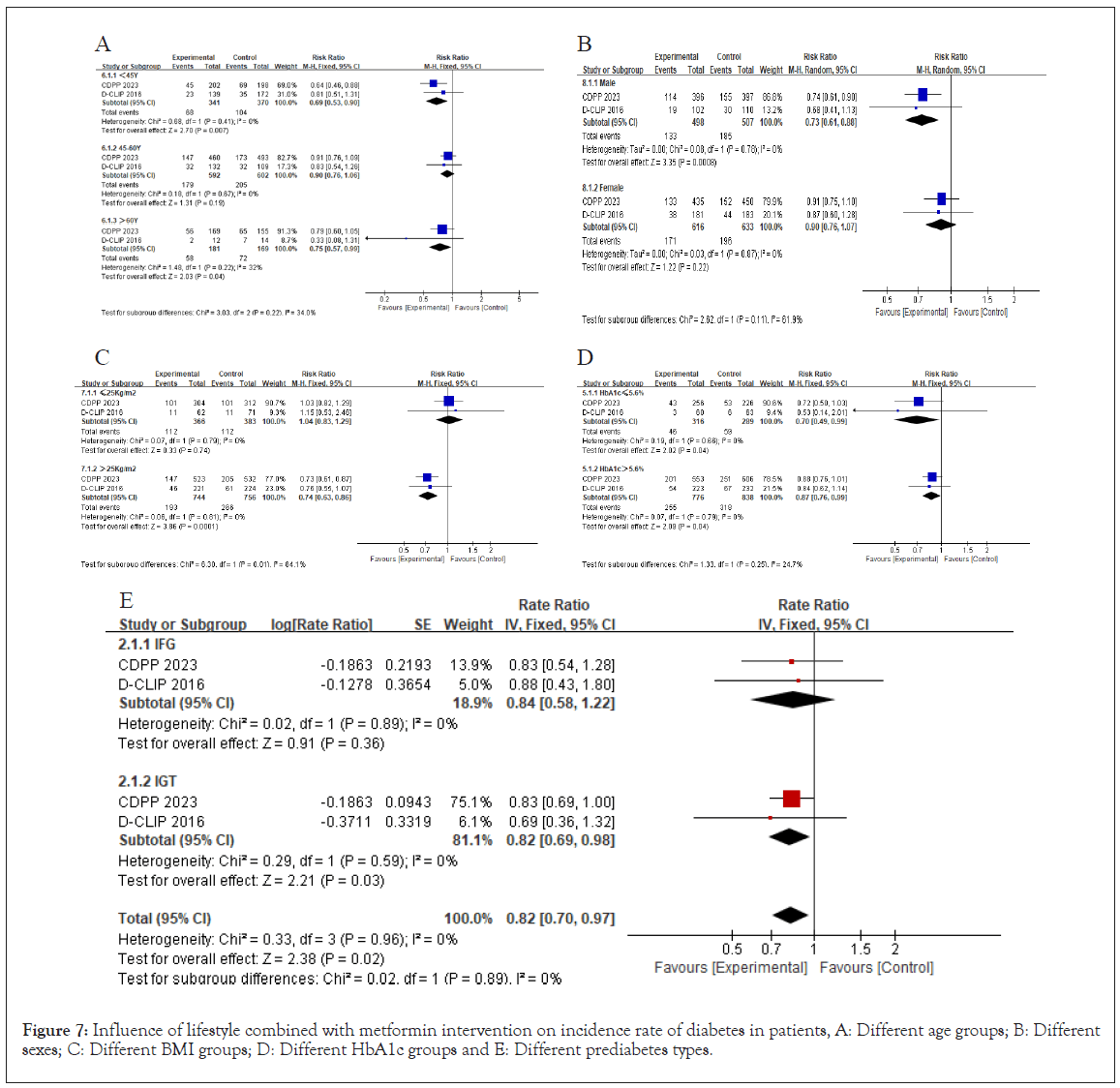
Figure 7: Influence of lifestyle combined with metformin intervention on incidence rate of diabetes in patients, A: Different age groups; B: Different sexes; C: Different BMI groups; D: Different HbA1c groups and E: Different prediabetes types.
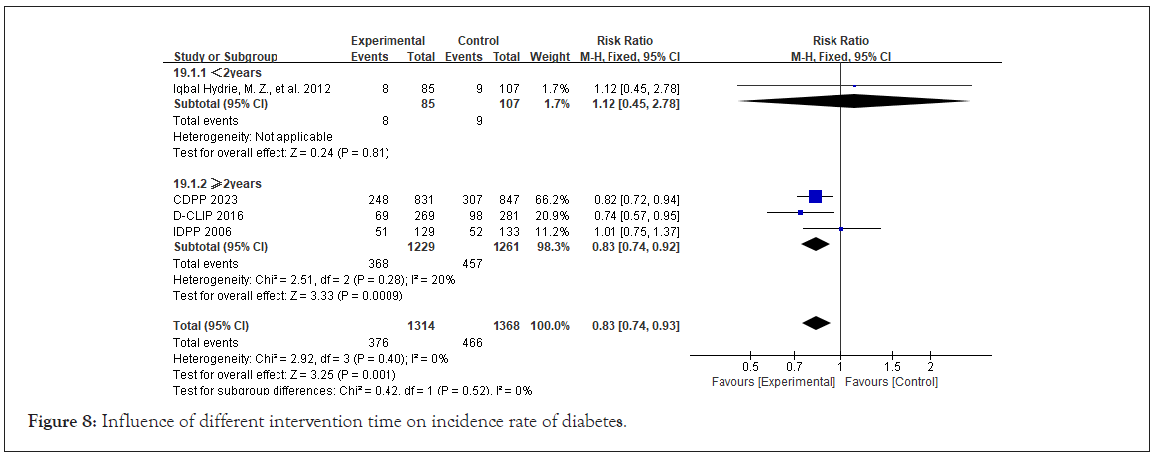
Figure 8: Influence of different intervention time on incidence rate of diabetes.
PD is a high-risk group of diabetes with a high prevalence rate. If no intervention is given, about 25% of PD patients will develop diabetes in the next 3-5 years, and 70% will develop diabetes at some stage of life [11]. In addition, studies have shown a significant increase in the risk of microvascular and macrovascular complications in PD patients, even existing during the PD period [12-14]. Therefore, it is necessary to intervene in the PD population. At present, research shows that lifestyle change can effectively reduce the risk of diabetes in PD patients [2-4]. Even so, in the long-term followup study, it was found that there are still some PD patients who develop diabetes, and long-term lifestyle intervention is difficult to adhere to, thus reducing the benefits [15,16]. Therefore, drug intervention has become a supplementary treatment based on lifestyle intervention. At present, research focuses on the preventive effect of hypoglycemic drugs on diabetes, of which metformin is the most abundant evidence. The ADA proposed to add metformin to high-risk PD population with the possibility of developing diabetes, such as those with BMI 35 kg/m2, high fasting glucose (e.g. 110 mg/ dL) and higher HbA1c. Due to different ethnic groups, the above high-risk population accounts for a relatively small proportion in Asia. Therefore, this Meta-analysis is based on four RCT studies, involving a total of 2682 subjects, demonstrating the efficacy of lifestyle combined with metformin in the prevention of diabetes in Asian patients with pre diabetes.
The results of this meta-analysis show that the combined intervention of intensive lifestyle and metformin can reduce the risk of diabetes in PD patients more than that of only intensive lifestyle intervention, about 17%. This result is similar to the research results of China's diabetes prevention plan [9], but lower than the results in the study of the USA diabetes prevention plan [2], which may be due to the lower BMI and more severe insulin resistance of Asian people, and may be caused by factors such as gene composition and lifestyle of Asian pre diabetes population. A Japanese study shows that KCNJ15 gene mutation can significantly increase the risk of type 2 diabetes. Compared with the western population, the proportion of Asian population with gene mutation is significantly higher than that of the western population, no matter fat or thin [17]. At the same time, the diet structure of Asian population is mostly carbohydrate, and there is more demand for insulin. In addition, lack of exercise leads to the reduction of insulin sensitivity, which further aggravates insulin resistance.
In subgroup analysis, the results showed that the combination of intensified lifestyle and metformin had better effects on IGT males aged <45 years and with a BMI>25 kg/m2. In IGT population, the effect of lifestyle intervention and metformin intervention has been relatively clear [2-4,18-20], but there are few studies on the intervention effect of IFG patients at present [8,9].The research results show that the combination of intensive lifestyle intervention and metformin intervention does not reduce the risk of diabetes in IFG patients compared with only intensive lifestyle intervention. However, no blank control group has been set in the above two studies, so it cannot be determined whether only intensive lifestyle intervention can reduce the risk of diabetes in IFG patients. In theory alone, metformin can inhibit liver glucose output, increase peripheral tissue insulin sensitivity, and increase glucose utilization to reduce fasting blood sugar. This is symptomatic for IFG patients, so more rigorous clinical trials are needed to study the efficacy of this intervention on the IFG population, and even more basic experiments are needed to explore whether there are more pathological and physiological mechanisms that affect the blood sugar levels of IFG patients. This Meta-analysis shows that combined metformin intervention is necessary, and the effect of higher doses of metformin (>1000 mg/d) on reducing the risk of diabetes is better, which is inconsistent with the research results of IDPP, but the hypoglycemic effect of metformin is dose dependent, so the effect of adding higher doses of metformin on the basis of lifestyle intervention is better, which is in line with the characteristics of drug action itself. In the subgroup analysis of intervention time, a longer time (>2 years) of lifestyle and metformin combined intervention showed a better effect in preventing diabetes, and the age subgroup analysis showed that the combined intervention was more effective in young (<45 years old) patients with prediabetes. Therefore, the younger the age of patients with prediabetes, the longer the combined intervention should be taken, which is different from the view in daily clinical practice. The reason may include some patients' concerns about drug dependence [9]. Therefore, in clinical diagnosis and treatment, PD patients should be educated about the necessity and effectiveness of joint intervention, to relieve patients' concerns about drug use, increase patients' compliance, and achieve better prevention effect. In the current study, most of the effects of intervention methods are achieved through weight loss. Some studies show that weight loss is the main predictor of the reduction of diabetes incidence rate. Every 1 kg weight loss reduces the risk of diabetes by 16% [21]. The studies included in this Meta-analysis also reported weight loss, with the combined intervention group showing more significant weight loss than the simple lifestyle intervention group. However, due to insufficient data in the included study reports, meta-analysis cannot be conducted.
In Asian prediabetes population, compared with the single lifestyle intervention, lifestyle intervention combined with metformin can further reduce the risk of diabetes in prediabetes patients, especially in male patients with abnormal glucose tolerance whose age is less than 45 years, BMI>25 kg/m2, and HbA1c ≤ 5.6%, which can reduce by 17%, and the effect is positively related to the dose of metformin and the intervention time.
As the intervention measures included in the experiment were obvious, the study did not use blinding, and there was a high risk of implementation bias in the quality evaluation of the article. Although the outcome indicators were all laboratory indicators, they may also affect the participants' ability to act, compliance, and other aspects, which may have unpredictable effects on the experimental results. In terms of statistical processing, the actual benefits of some subgroup analysis data come from individual literature, so extra caution should be exercised when drawing conclusions and discussions.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Li J, Ma Y, Lu J, Wang W, Wang X, Hao Y (2024). Meta-Analysis on the Impact of Lifestyle Intervention Combined with Metformin on the Incidence of New-Onset Diabetes in Prediabetic Asian Populations. J Clin Toxicol. 14:570.
Received: 24-Jun-2024, Manuscript No. JCT-24-33296; Editor assigned: 27-Jun-2024, Pre QC No. JCT-24-33296 (PQ); Reviewed: 11-Jul-2024, QC No. JCT-24-33296; Revised: 18-Jul-2024, Manuscript No. JCT-24-33296 (R); Published: 25-Jul-2024 , DOI: 10.35841/2161-0495.24.14.570
Copyright: © 2024 Li J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.