Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
+44 1300 500008
ISSN: 2167-7948
+44 1300 500008
Case Report - (2020)Volume 9, Issue 1
Papillary-type thyroid cancers are common malignancies in the head and neck region. They mostly appear without any metastasis because most cases are discovered incidentally. According to recent guidelines, papillary microcarcinoma can be safely followed over ten years, and only a small percentage will show significant growth or metastasis. Approximately one third of adults have papillary microcarcinomas in their thyroid, but most will never progress into metastatic cancer. Here, we describe a male adult treated for cervical metastasis of papillary cancer in the thyroid gland. The patient underwent total thyroidectomy, central neck dissection, and lateral neck dissection. A meticulous histological examination showed papillary thyroid cancer metastasis in the central compartment as well as in region 4 in the lateral compartment. There was no sign of primary papillary cancer in the thyroid gland. Only a few cases have been found in the literature when cervical metastasis of papillary cancer appears without any detectable primary focus in the thyroid gland.
Papillary thyroid cancer; Unknown primary tumor; Lymph node metastasis; Thyroid surgery
Differential diagnosis of a solitary lateral cervical mass can be difficult. Pathologies behind a cervical mass include benign conditions (reactive lymphoid enlargements, brachial cysts); malignancies such as branchiogenic cancer; and lymph node metastases from oro-nasopharyngeal, thyroid, or salivary gland carcinomas. Guidelines in patients with cervical lymph node metastasis suggest that PET/CT detects the primary site in 37% of cases. Diagnostic evaluation should be individually guided. The first step is to take a detailed medical history including family history followed by a physical examination that covers the head and neck region, breasts in females, the testis in men, and a digital rectal examination. Tumor markers and viral serology activities (especially in head and neck region) may also present useful information. Diagnostic evaluations such as ultrasound, fine needle aspiration biopsy (FNAB), CT, MRI, PET/CT, mammography, and upper/lower endoscopy could be helpful in differential diagnosis.
Further examination is also needed to exclude other primary malignancies in the head and neck region such as squamous cell carcinoma or melanoma that can lead to metastasis in the neck lymph nodes [1]. Aspiration cytology in practiced hands can help to define the origin of the primary tumor. For thyroid cancer, the appropriate surgical procedure is thyroidectomy and central neck dissection for biopsy-proven metastasis in the central neck region. In most thyroid cancer cases, the primary tumor is located in either lobe or in the isthmus. Papillary thyroid cancer (PTC) is the most common thyroid malignancy. Surgery is considered for patients with a solitary, cytologically indeterminate nodule, and thyroid lobectomy is the recommended initial surgical procedurethis procedure can be modified based on sonographic evaluations or molecular assays. Completion thyroidectomy is recommended based on the indeterminate nodule being malignant following lobectomy after histological revision.
According to guidelines, the recommended treatment of patients with thyroid cancer presenting biopsy-proven cervical lymphadenopathy is total thyroidectomy with appropriate ipsilateral and/or modified contralateral modified radical neck dissection [2]. The prognosis is usually good when surgery is followed by radionuclide scanning and lifelong thyroid supplementation. Here, we report a case of an occult papillary thyroid carcinoma appearing in the form of a soliter lateral cervical mass.
A 46-year-old male patient with no past medical problems was referred to our department by primary care physician with a painless left neck mass that had increased in size over the last nine months. He had no associated fever, weight loss, or night sweats. Physical examination showed a left mobile mass of 3 cm with firm consistency in the left supraclavicular fold. Family and social history were unremarkable. The neck ultrasound (Figure 1) revealed a left thyroid lobe that was 45 mm × 16 mm × 18 mm lower and a right lobe (45 mm × 15 mm × 20 mm) with a 10-mm cystic nodule in its lower pole. Ultrasound detected a 33 × 24 mm enlarged lymph node mass in the left supraclavicular fossa. A detailed examination of the head and neck along with flexible fiberoptic laryngoscopy was negative for any suspicious lesions. The result of the aspiration cytology from this mass was metastasis from a papillary thyroid cancer.
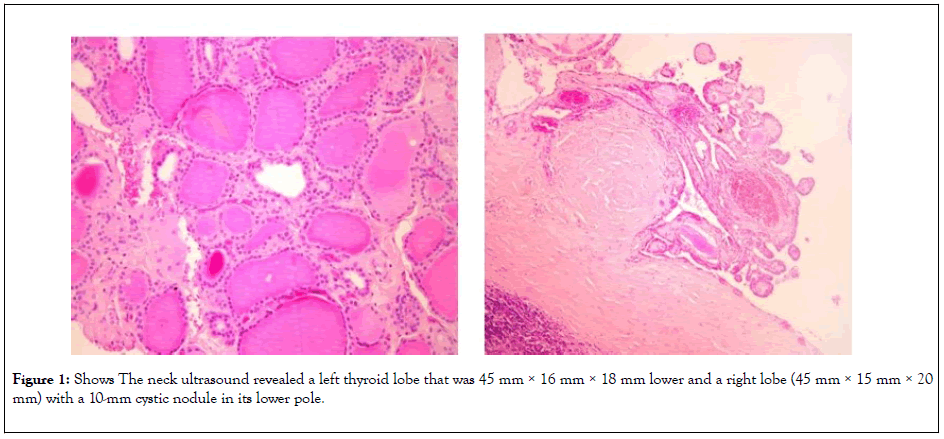
Figure 1: Shows The neck ultrasound revealed a left thyroid lobe that was 45 mm × 16 mm × 18 mm lower and a right lobe (45 mm × 15 mm × 20 mm) with a 10-mm cystic nodule in its lower pole.XXXXXXXimage PendingXXXX
The patient underwent a total thyroidectomy, central compartment neck dissection, and left lateral neck dissection. The lymph nodes were dissected on the left side from levels 2, 3, 4, and 5 as well as from the central neck compartment. The lymph node at level 4 and in the central compartment were positive for metastatic papillary carcinoma. The immunohistochemical study of tumor cells was positive for thyroglobulin confirming the diagnosis. Careful pathologic examination of the thyroid gland was surprisingly negative for the presence of primary thyroid carcinoma (Figure 2).
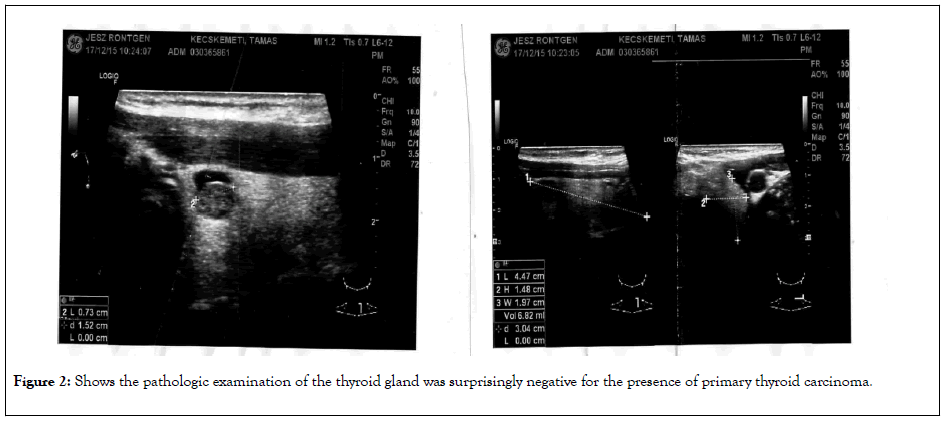
Figure 2: Shows the pathologic examination of the thyroid gland was surprisingly negative for the presence of primary thyroid carcinoma.
RAI therapy was instituted postoperatively to treat occult foci of PTC. A radioiodine nuclear scan performed three months later and did not show any uptake. The patient was started on a thyroxine supplement.
According to the European Network of cancer registries, the incidence of thyroid cancer in Europe was 6.3 cases per 100,000 person-years [3]. The most common type (~90%) is differentiated thyroid cancer (follicular and papillary) originating from the follicular epithelium. Papillary thyroid cancer is the most common type [4,5]. Recent guidelines recommend that small<1 cm (or 1 ml volume) thyroid nodules can be followed with active surveillance (ultrasound, combined with cytologic examination). Several studies have shown that it is safe and effective to follow up low-risk papillary microcarcinomas (<1 cm) over 5-10 years. During this time, only 12%-14% of papillary microcarcinoma show a significant increase in size (more than 50%), and novel lymph node metastases are detected in only 2%-5% of the cases [6]. Almost one third of adults live with papillary microcarcinoma in the thyroid, and most have no symptoms [7].
Diagnostic options to examine these cervical lymph nodes include ultrasound, magnetic resonance imaging (MRI), computed tomography (CT) scan, and fine needle aspiration (FNA). Twenty-five percent of patients with a thyroid malignancy may have normal thyroid imaging, which poses a diagnostic challenge. The thyroid nodules can be benign lesions as well. Aspiration can be useful if a nodule is suspicious for malignancy [8].
The first manifestation of PTC is isolated cervical lymphadenopathy. The primary focus is not detectable in some cases. Advanced cases can present with laryngeal nerve palsy, cysts, distant metastasis, and isolated cervical lymphadenopathy as seen in our patient. Most palpable cervical lymph nodes are located at the mid-jugular level (48%), lower jugular level (29%), the posterior triangle (9%), upper jugular level (9.7%), and in the submandibular lymph nodes (3.2%) [9]. In some case, the incidence of clinical and/or radiological lymphadenopathy at the time of cancer diagnosis is estimated at 20% to 25% for all sizes of thyroid tumors [10].
Agosto-Vargas et al. [11] reported a case of a young man who presented with a lateral neck mass that was found to be a malignant transformation of heterotopic thyroid tissue. Ectopic thyroid tissue on the neck originates from abnormal thyroid migration during fetal development. This is commonly found in the cervical midline. Only 1%-3% is located to the lateral neck. The accurate incidence of lateral neck ectopic thyroid carcinoma is not known, and it is almost impossible to distinguish these from metastasis originating from the primary thyroid carcinoma. Malignant transformation of ectopic thyroid tissue is extremely rare: Only 43 cases have been reported. For example, Vazquez et al. [12] reported a rare presentation of mediastinal ectopic thyroid tissue transforming into aggressive, radioiodine uptakelacking, metastatic PTC.
The thyroid has a specific lymphatic network exhibiting rich anastomoses. The anatomy of the lymphatic drainage in the thyroid gland can explain the multifocal localization and contralateral occurrence of PTC [13,14] Although it is rare (ca. 1%), malignant transformation in the thyroglossal duct cyst can also present as a cystic midline mass [15]. Batoriet al. [16] reported an occult 3-mm papillary thyroid cancer presenting with an ipislater 4 cm large cervical mass infiltrating the adjacent internal jugular vein and recurrent laryngeal nerve. Following radical neck dissection, total thyroidectomy, and radioiodine treatment, the patient had no recurrence for 7 year postoperatively. The incidence of PTC with synchronous lymph node metastasis is about 20%-90%, but first presentation of occult PTC as a lateral cervical mass is extremely rare. Davidson et al. [17] reported the case of an 84-year old woman diagnosed with intrathyroidal PTC, total thyroidectomy, and radioiodineremnant ablation. The post-therapy whole body scan was negative. Two years later, the woman developed biopsy-proven, FDG-avid PTC metastasis in her pancreas. The authors reviewed the literature and between 1991 and 2017 they found only 11 cases of pancreas metastases of PTC reported in PubMed. There was no other metastasis except for the pancreas in four patients and their own patient out of 12 total.
Schwaiger et al. [18] described a similar case as oursa very rare case of a large slow-growing lateral neck metastasis originating from a 6-mm large papillary thyroid microcarcinoma. The patient underwent complete resection of the metastasis and the thyroid followed by radioiodine therapy to achieve a complete cure.
Lateral cervical cystic masses rarely only present in occult thyroid carcinoma. In most cases, it is indeed a metastatic lesion from a primary thyroid lesion, but it could also be ectopic tissue associated with a branchial cyst [19]. The definition of occult carcinoma by the National Cancer Institute is “cancer in which the site of the primary (original) tumor cannot be found” [20]. Boucek et al. [21] used initial presentation and final detection of the primary tumor to define four categories of occult thyroid carcinoma: 1. incidental microcarcinoma found incidentally in the thyroid specimen after removal for benign disease; 2. microcarcinoma incidentally detected by ultrasound and proved by FNAC; 3. Metastasis detected first with primary tumor not found by imaging before surgery; microcarcinoma is found in the histological specimen; and 4. thyroid cancer in ectopic thyroid tissue with apparent metastases. Liu et al. [22] recently added a fifth group comprising two types: Sub-type one is thyroid cancer metastases in the central lymph nodes after total thyroidectomy for benign disease. Sub-type two is distant metastases that presents before a primary thyroid carcinoma. They further reported a case of the fifth group of occult thyroid carcinoma [23].
Most metastases from occult primary tumors are found in the head and neck. Of these, papillary thyroid cancer presenting as a metastatic cervical lymphadenopathy is extremely rare. However, the thyroid gland seems normal clinically and radiologically; thus, the appropriate treatment is total thyroidectomy with central and lateral neck dissection followed by postoperative radioiodine treatment and lifelong thyroid hormone substitution. The outcome is usually favorable. PTC is rarely an aggressive cancer. Most ultrasound-detected, FNAC-proven papillary microcarcinomas could be safely followed over 5-10 years without removing them. It is unclear why 2%-5% of the cases metastasize, and there is no explanation why the primary PTC in the thyroid can sometimes not be found. One study reported cyclin D1 overexpression in 90.9% of metastasizing PTC. In contrast, this was only 8% in non-metastasizing PTC. We present this file for its rarity: a large cervical papillary cancer metastasis but with the total absence of tumor foci during microscopic examination of the thyroid specimen. Only a few such cases have been reported in the literature. The heterogenous genetic background, the burn out of the primary cancer, and defective immune surveillance could all play a role in the remission of the primary tumor while giving rise to a local or distant metastasis.
Citation: LévayB, Boér A, Oberna F, Dohán O (2020) Metastatic Papillary Thyroid Cancer with no Primary Tumor in the Thyroid Gland. Thyroid Disorders Ther. 9:236. DOI: 10.35248/2167-7948.20.09.236
Received: 01-May-2020 Accepted: 15-May-2020 Published: 22-May-2020 , DOI: 10.35248/2167-7948.20.09.236
Copyright: © 2020 Lévay B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.