Mycobacterial Diseases
Open Access
ISSN: 2161-1068
ISSN: 2161-1068
Research Article - (2018) Volume 8, Issue 1
Background: Tuberculosis (TB) is a chronic infectious disease that has a major health problem over the centuries and it has accounted for more human misery suffering and loss of earning and failure of economic and social development than any other disease. The aim of the study was to assess the effect of prognostic factors associated with time to recovery of adult TB patients who were under treatment follow-up of Mizan-Tepi University Teaching Hospital.
Study Design: A retrospective cohort study.
Methods: The data was obtained from medical records of TB patients registered during September 2011 to August 2016 and treated under the DOTS program. Kaplan-Meier and Cox proportional hazards model were applied. Backward selection procedure was used in variable selection.
Results: In this study, 75% were recovered, 4.4% died, 9.7% defaulted, and 4.9% failure, while 6% transferred out rate. The median recovery time of the patients was 185 days (6 months and 5 days) but it varies depending on the covariates included in the study. TB Type (P<0.001), family size (P=0.035), Co-morbidity (P=0.045) and bodyweight (P=0.044) at baseline had a statistically significant.
Conclusion: The effects of TB type, family size, co-morbidity and bodyweight at baseline had a statistically significant impact on time-to-recovery. The variables that are significant should be considered during the selection phase a treatment (combination of treatments) for TB.
Keywords: Tuberculosis; Cox proportional hazards model; HIV; Chronic infection
• The TB treatment success rate of the study was 75%.
• The median recovery time of the patients was 185 days but, varies depending on the covariates included in the study.
• The effects of TB Type, family size, Co-morbidity and bodyweight at baseline had a statistically significant impact on time-torecovery.
Tuberculosis (TB) is a chronic infection disease that has a major health problem over the centuries, it has accounted for more human misery suffering and loss of earning and failure of economic and social development than any other disease (USAID, 2009). In developing countries where population is dense and hygienic standards are poor, tuberculosis remains a major fatal disease; the high frequency of Mycobacterium tuberculosis in Sub-Sahara African countries as a result of poor nutrition, inadequate TB control measures, inadequate program for the disease and rapid growth of the population [1].
In 2016, there were an estimated 1.3 million TB deaths among HIV negative people and an additional 374,000 deaths among HIV-positive people. An estimated 10.4 million people (90% adults, 65% male, 10% people living with HIV) fell ill with TB in 2016. Regionally, the fastest declines in the TB mortality rate are in the WHO European Region and the WHO Western Pacific Region (6.0% and 4.6% per year, respectively, since 2010). High TB burden countries with rates of decline exceeding 6% per year since 2010 include Ethiopia, the Russian Federation, the United Republic of Tanzania, Viet Nam and Zimbabwe and 98% of TB deaths are in the developing world affecting mostly young adults in their most productive years most of them are in Africa [2,3]. TB is one of the major threats to public health in Ethiopia and the Ethiopian Government has identified Multi-Drug Resistant TB (MDR-TB) as a priority public health problem. Ethiopia, having experienced a major increase in the burden of TB, presents one of the most serious public health challenges.
TB is the most abundant disease in the world as it is easily transmitted from TB patient to normal person. Despite of its abundance, this disease has tendency to cause death mostly when its co-morbidity manifested on patient with other disease like AIDS, diabetes and others. It has high chance of making a patient economically dependent on their family/household members rather than the loss it can cause from his/her none productiveness. As economic development starts from individual contribution it needs to overcome the effect of TB on health of individuals in the society [4].
A study at Enfraz Health Center, Northwest Ethiopia, among 94.8% had successful treatment outcome. The overall death, default, and failure rates were 3.4%, 0.5%, and 1.2%, respectively. There was no significant association between sex, age, residence, type of TB, HIV status, and successful TB treatment outcome [5]. A study done in the Upper West Region of Ghana, it was observed that female patients had more chance of recovery than their male counter parts. Variables that significantly contributed to recovery were age, type of patents, duration of treatment, and HIV status of the patient. A median recovery time of TB was 25.43 weeks [6]. A study done on survival analysis of average recovery time of tuberculosis patients in northern region, Ghana, it was observed that the survival rates for males and females were 85.71% and 88.46% respectively. Age of patient at diagnosis, category, and type of patient were crucial determinants of treatment outcome. A median recovery time of 22 weeks in the Region [7]. A study at Shangla, Khyber-Pakhtunkhwa, Pakistan, and the overall mean treatment success rate of the TB patients was 94.93%. The risk of unsuccessful outcome was significantly lower among TB patients age [8]. A study done in Hamadan, Iran, treatment success rate was 83.1%. Key determinants of poor treatment success rate, such as male gender, and not having hospitalization history during the treatment period, should be considered in efforts aimed to improve the treatment outcome in the management of TB [9].
The objective of the study was to assess the effect of prognostic factors associated with time to recovery of TB patients who were under treatment follow-up of Mizan-Tepi University Teaching Hospital. This is the first study to explore the risk of recovery during TB treatment in the study area. A better understanding of the predictors of recovery among the area could provide opportunities for policy makers to estimate the recovery time among active TB cases; thus enabling informed decisions on priorities. The results of this study will also help to engage policy makers, researchers and communities in working together to generate the knowledge that is needed for better care for TB patients in south-western Ethiopia, as well as to promote further research.
The data for the analysis were obtained from Mizan-Tepi University Teaching Hospital, and Institutional ethical clearance was provided by research coordinator of Mizan-Tepi University. Mizan-Tepi University Teaching Hospital wrote a letter of permission for the office of TB, and careful recruitment and training for data collectors were undertook.
Mizan-Tepi University teaching hospital established in 1978 E.C. is one of the oldest hospitals in the federal democratic republic of Ethiopia, found in Bench Maji zone in the southern nation’s nationalities and peoples state roughly some 561 km away from the capital Addis Ababa and it is the only hospital found in the zone. Patients treated under the DOTS program at Mizan-Tepi University Teaching Hospital were our study population. Data were extracted from medical records by health professionals, working at the hospital and variables on socio-demographic factors, clinical factors and time of the event were recorded. A retrospective follow-up study was conducted on patients initiating treatment from the 1st of September, 2011 and 30th of August, 2016 at the Mizan-Tepi University teaching Hospital. All TB patients whose charts were available and who had at least two months of follow-up (having at least two measurements) were eligible for the study.
Recovery (when patients controlled disease) time is the outcome variable (event) that were measured (coded as 1 for recovered and 0 for censored). Patient was considered recovered, if and only if he/she is smear-or X-ray negative test. The time of treatment were determined by calculating the difference between time of initiation and outcome of treatment. The patient surviving till end of the cohort study contributed a censored case. Censorship includes death, treatment failure, default, transfer out and study time completion. Completed treatment: When a patient completed treatment but did not meet the criteria for cure or failure. This definition applies to sputum smearpositive and sputum smear-negative patients with pulmonary TB and to patients with extra-pulmonary disease. Died: When a patient died from any cause during treatment. Failed: When a patient was initially sputum smear-positive and when a patient remained sputum smearpositive at month 5 or later during treatment. Defaulted: When a patient whose treatment was interrupted for 2 consecutive months or more. Successfully treated: When a patient was cured or completed treatment. Socio-demographic information of the patients and clinical characteristics considered were sex, age, TB type, co-morbidity, patients category at the start of follow-up, bodyweight, whether patient alive with person, the household size, patients health facility, and HIV offered test. Data were analyzed using R-software version 3.1.3.
In statistics analysis, model building is the process of developing a probabilistic model that best describes the relationship between the dependent and independent variables. The major issues are finding the proper form (linear or curvilinear) of the relationship and selecting which independent variables to include. Survival analysis examines and models the time it takes for events to occur. Survival data are conveniently summarized through estimates of the survival function and hazard function. Median is the preferred summary measure of the location of the distribution. The K-M survival curves can give us an insight about the difference of survival functions in two or more groups, but whether this observed difference is statistically significant requires a formal statistical test [10]. We used Cox proportional hazard model for the analysis and model building. The Proportional Hazards Moded is used for multivariable analysis to identify factors associated with recovery from tuberculosis and Cox proportional hazards (PH) model. The Cox proportional hazards (PH) regression model [11]. A broadly applicable and the most widely used method of survival analysis. The Cox-PH model is a semi-parametric model where the baseline hazard α(t) is allowed to vary with time-
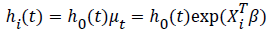 ................(1)
................(1)
Where,h0(t), is the baseline hazard function- Xi is a vector of covariates and β is a vector of parameters for fixed effects. Parameter estimaterefers to the increase in log-hazard with a one unit increase for the continuous covariate.
The final Cox PH model (1) for TB is then given by:-
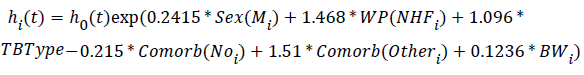
Table 1 presents basic descriptive information that summarizes the Survival status of TB patients in Mizan-Tepi University Teaching Hospital. Among 1151 TB patients, 863 (75%) had successful treatment outcome. The overall default, transfer out, failure, death were 112 (9.7%), 69 (6%), 56 (4.9%) and 51 (4.4%) respectively.
| Status | Number | Percent |
|---|---|---|
| Treatment success | 863 | 75.0 |
| Default | 112 | 9.7 |
| Died | 51 | 4.4 |
| Treatment failure | 56 | 4.9 |
| Transfer out | 69 | 6.0 |
| Total | 1151 | 100 |
Table 1: Treatment outcome of tuberculosis patients.
Table 2 describes the survival status of patients with determinant factors. Out of 1151 TB patients, 863 (75%) were recovered and the rest 288 (25.0%) censored from the study. The median recovery time of the patients was 185 days (6 months and 5 days) but it varies depending on the covariates included in the study.
| Parameters | Total (1151) | Recovered (863) | Median recovery (Day) | ||
| Number | Percentage | Number | Percentage | ||
| Sex | |||||
| Female | 460 | 40.0 | 351 | 40.7 | 289 |
| Male | 691 | 60.0 | 512 | 59.3 | 177 |
| Type of tuberculosis | |||||
| Extra pulmonary TB | 229 | 19.9 | 182 | 21.1 | 184 |
| Pulmonary TB | 922 | 80.1 | 681 | 78.9 | 177 |
| Offered HIV Test | |||||
| No | 160 | 13.9 | 113 | 13.1 | 199 |
| Yes | 991 | 86.1 | 750 | 86.9 | 184 |
| Alive with person | |||||
| No | 113 | 9.8 | 74 | 8.6 | 173 |
| Yes | 1038 | 90.2 | 789 | 91.4 | 188 |
| Co-morbidity | |||||
| HIV | 163 | 14.2 | 117 | 13.5 | 184 |
| No | 976 | 84.8 | 741 | 85.9 | 188 |
| Other | 12 | 1.0 | 5 | 0.6 | 168 |
| Patients working facility | |||||
| From health facility | 16 | 1.4 | 6 | 0.7 | 183 |
| Not health facility | 1135 | 98.6 | 857 | 99.3 | 168 |
| Patients category at beginning | |||||
| New | 1139 | 99.0 | 856 | 99.2 | 185 |
| Relapse | 12 | 1.0 | 7 | 0.8 | 218 |
Table 2: Descriptive baseline of tuberculosis patients for categorical variables.
Amongst the patients infected with TB, 460 (40.0%) were female and 691 (60.0%) were male. Regarding the patients infected with TB, 229 (19.9%) were extra pulmonary and 922 (60.0%) were pulmonary. Among patients, 991 (86.1%) were offered HIV test and 160 (13.9%) were not.
Majority of patients were living (90.2%) with person. Among patents offered HIV test 163(16.5%) have HIV positive. Majority of patients were not infected with the other disease. Among female patients, 351 (40.7%) recovered the disease and the rest 109 (23.7%) loss to follow-up and of male patients, 512 (74.1%) experienced the event and the rest 179 (25.9%) loss to follow-up from the study. The median recovery time for female and male TB patients were 289 and 177 days respectively. As compared to male patients majorities of female patients recovered the disease.
Among Extra pulmonary TB patients, 182 (21.1%) recovered the disease and among Pulmonary TB patients, 681 (78.9%) recovered the disease. Majority of patients with pulmonary TB recover the disease as compared to Extra Pulmonary TB patients. Among TB patients, 1139(99%) were new patients and 12 (1.0%) were relapse. Among patients, 16 (1.4%) working place were from health facility and 1135 (98.6%) were not from health facility.
Figure 1 shows patients with Pulmonary TB have a higher probability to recover than Extra Pulmonary.
The constant graph of the survivor function (Figure 1) for both Extra Pulmonary TB and Pulmonary TB in the first 133 days is the fact that no recovery is possible within that period. Thereafter, the graph for the pulmonary TB declined between 133 and 165 days, indicating that some of the patients had recovered. The Extra pulmonary TB however, started their recovery after 165 days.
Multivariable results of a Cox PH model (1) and Table 3 shows that effects of TB Type (P<0.001), family size (P=0.035), Co-morbidity (P=0.045) and bodyweight (P=0.045) at baseline had a statistically significant impact on time-to-recovery while Sex, and working place from health facility not statistically significant impact on time to recovery.
| Covariates | Hazard Ratio (95% CI) | P-value |
|---|---|---|
| Sex(Male) | 1.27 (0.97, 1.68) | 0.088 |
| Workplace (Not from Health Facility) | 4.34 (0.00, 10.34) | 0.989 |
| Pulmonary tuberculosis | 2.99 (1.89, 4.74) | 0.001 |
| Family size | 0.93 (0.88, 0.99) | 0.035 |
| Co-morbidity with HIV | 0.81 (0.57, 1.14) | 0.219 |
| Co-morbidity without HIV | 4.52 (1.03, 19.75) | 0.045 |
| Bodyweight | 1.13 (1.03, 1.43) | 0.045 |
Table 3: Multivariable cox proportional hazard model using backward selection method.
The 95% confidence interval for hazard ratio that do not include 1 implies that the variables are significant, else not. Again also, the likelihood ratio test (P-value=0.000), Wald test (P-value=0.000) and score (logrank) test (P-value=0.000) are highly significant.
The 95% confidence interval for hazard ratio that do not include 1 implies that the variables are significant, else not. Again also, the likelihood ratio test (P-value=0.000), Wald test (P-value=0.000) and score (logrank) test (P-value=0.000) are highly significant.
The P-value for sex is 0.088. The hazard ratio=exp(coef)=1.27. Because, the p-value for sex greater than 5% implies sex have a smaller contribution to the difference in the HR. For example, holding the other covariates constant, male TB patients induce hazard of recovery by a factor of exp(beta)=1.27, or 27.3%, which is not a significant contribution.
The hazard ratio of recovery for Pulmonary TB type patients was 2.99 (P<0.001) holding other variables constant.
This means that pulmonary TB patients were 2.991 times greater recovery time than extra pulmonary TB patient holding other variables constant. Pulmonary TB patient recover the disease early as compared to extra pulmonary.
There was no significant association between sex, age, workplace, offered HIV test, alive with person in the home, and person category at beginning. Similarly, the P-value for household size of patients is 0.035, with a hazard ratio HR=0.93, indicating, for a unit increase of household size of patients reduces the recovery by a factor of 0.93, holding the other covariates constant.
We conclude that, a small household size of patients associated with good prognostic. Similarly, the P-value for bodyweight of TB patients is 0.045, with a hazard ratio HR=1.13, indicating a strong relationship between the bodyweight value and increase recovery.
Holding the other covariates constant, an additional kg of bodyweight increases daily recovery by a factor of exp(beta)=1.13, or 13%.
A unit increase of bodyweight in kg associated with good prognostic. Active tuberculosis develops primarily in people with weakened immune systems, especially in people with HIV, and can trigger a serious infection to the lungs, resulting in death.
The rate of recovery was 4.52 times TB/ with other co-morbidity (none HIV) patients than cases with TB/HIV co-morbidity holding other variables constant.
TB/HIV co-morbidity patients prolonged recovery time as compared to TB with other co-morbidity.
Types of TB, Co-morbidity, bodyweight at baseline, and household size of patients at baseline are significantly associated with time to recovery of TB patients.
These variables are important factors that should be considered during the selection phase a treatment (combination of treatments) for TB.
Thus, the higher the bodyweight, household size of patients at baseline the faster the rate of the recover from TB.
The baseline survival and hazard are decreasing and increasing respectively as time goes (Figure 2). The Cox PHs model is a semi- parametric model where the baseline hazard h0(t)and survival S0(t) vary with time. The patients’ chance of recovery time up to 152 days slowly decreases and increases for baseline survival and hazard function respectively.
Many researches on tuberculosis (TB) treatment have reported varying recovery times. In the current study, from 1,151 patients on anti-TB treatment at hospital, 75% were recovered, 4.4% died, 9.7% defaulted, 4.9% failure, and 6% transferred out rate. The success rate was below the health development annual target plan (success rate annual target plan 80%) of 2016/17. However, the studies done in Upper West Region of Ghana 73.75% were recovered with 26.25% censored, which is somehow consistent with current study [6]. Unlike study in northwest Ethiopia reports, 94.8% of TB patients recovered, 3.4% death, 0.5% default, and 1.2% failure rate [5]. In addition, a study done in Shangla, Khyber-Pakhtunkhwa, Pakistan the overall mean treatment success rate of the TB patients was 94.93% and a study done in Hamadan, Iran, treatment success rate was 83.1% are above the current study [8,9]. The possible explanations for the lesser recovery in our study might be low counseling sessions in this study.
If TB is detected early, it can be treated in six months whiles it takes between six to ten years to treat for late detection [12]. In this study, the median recovery time of the patients was 185 days (6 months and 5 days) or 24 weeks and 5 days which is consistent with the study done in India but the study done in Northern Region, Ghana reported a median recovery time was 22 weeks in the Region [7,13]. This variation may be due to patients not encouraged to visit the health center regularly, not to take the drugs as prescribed and environmental and nutritional difference.
HIV and TB are associated with a higher mortality, although most deaths in those who receive an effective therapy are due to complications of HIV infection rather than tuberculosis [14,15]. In this study, 14.2% were co-infected by HIV and TB and follow both ART and anti-TB treatment. However, studies done in Dawuro Zone South West of Ethiopia, 8.1% were co-infected by HIV/TB [16]. The possible explanation for the higher prevalence of TB/HIV in current study were poor public knowledge and awareness about the risk factors for TB, symptoms of TB, and the implications of the diagnosis of latent infection.
There was no significant association between age, sex, workplace, offered HIV test, alive with person, and person category at beginning in this study. It might be because younger took medication appropriately and in the same way older took medication correctly, since they know the value of life more than other age group, for their better survival.
Types of TB, Co-morbidity, bodyweight at baseline, and number of people living at baseline are significantly associated with time to recovery of TB patients in this study like study done in Upper West Region of Ghana, unlike study done in IbnuSina Hospital at Gresik District Indonesia [17].
Health Departments and TB-Control Programs of Mizan-Tepi University Teaching hospital should; identify important factors like; types of TB, Co-morbidity, bodyweight at baseline, and number of people living with patients during the selection phase a treatment (combination of treatments) for TB. Identify contacts of patients with infectious TB and treatment of those at risk with an effective drug regimen. Improve public knowledge and awareness about the risk factors for TB, symptoms of TB, and the implications of the diagnosis of latent infection by TB control programs, community-based organizations representing populations at high risk, and academic health sciences institutions. Social determinant of health is becoming more important, and further research in health system (HSR) on factors that influence the disease, such as poverty, malnutrition, addiction, AIDS, education, housing, unemployment, migration, and social beliefs is strongly recommended.
This study is limited by primary data and some of the predictors that had been related to recovery in other studies of TB patients were not assessed because of unavailable in patients’ chart.
The TB treatment success rate of the current study was below the health sector development annual target plan. The median recovery time of the patients varies depending on the covariates included in the study. The effects of TB Type, family size, Co-morbidity and bodyweight at baseline had a statistically significant impact on timeto- recovery. Patients with Extra-Pulmonary TB delay the recovery time as compared to Pulmonary TB.
The TB treatment success rate of the current study was below the health sector development annual target plan. The median recovery time of the patients varies depending on the covariates included in the study. The effects of TB Type, family size, Co-morbidity and bodyweight at baseline had a statistically significant impact on timeto- recovery. Patients with Extra-Pulmonary TB delay the recovery time as compared to Pulmonary TB.
First, we would like to thank Mizan-Tepi University for granting financial support. Secondly, Mizan-Tepi University Teaching Hospital TB patient’s office for their help during data collection. Lastly, not from the least, we thanks to our parents and friends, whose love, trust, encouragement, comfort and support always surround us.
Not all the authors have any possible conflicts of interest.
The Mizan-Tepi University funded the present study.