Research Article - (2024)Volume 9, Issue 2
Purpose: The previous meta-analyses have illustrated that Multiple Sclerosis (MS) is correlated with multiple health outcomes. We designed an umbrella meta-analysis to evaluate the breadth, validity and presence of biases of the associations of MS with diverse health outcomes.
Methods: We searched three databases (PubMed, Web of Science and Embase) to recalculate the summary effect sizes, 95% CI, heterogeneity and small-study effects in the included meta-analyses. For each meta-analysis, we assessed the quality with AMSTAR2 and graded the epidemiologic evidence.
Results: A total of 28 articles comprising 84 unique meta-analyses were included in this study. Among the 84 unique outcomes, 52 unique outcomes had significant associations (p<0.05). Only 6 outcomes (Inflammatory Bowel Disease (IBD), Ulcerative Colitis (UC), Crohn’s Disease (CD), atrial fibrillation, herpes simplex virus type 2-IgG, hypothyroidism) showed high quality of epidemiological evidence. The remaining 46 outcomes were assessed to moderate or weak quality of evidence.
Conclusion: In our study, MS seems to increase the risk of IBD, UC, CD, herpes simplex virus type 2-IgG and hypothyroidism while decrease the risk of atrial fibrillation, with high epidemiological evidence. In order to verify our results, more prospective observational studies are needed.
Multiple sclerosis; Health outcomes; Epidemiological evidence; Meta-analysis; Density
CI: Confidence Interval; HR: Hazard Risk; RR: Relative Risk; OR: Odd Ratio; SMD: Standardized Mean Difference; g: Hedges; PPMS: Progressive Primary Multiple Sclerosis; RRMS: Relapsing-Remitting Multiple Sclerosis; BMD: Bone Mineral Density; ToM: Theory of Mind
Multiple Sclerosis (MS) is the origin of a chronic inflammatory and autoimmune demyelinating disease. The main factors of the MS development include genetic, environmental and exogenous factors. MS is characterized by multifocal and temporally scattered Central Nervous System (CNS) damage, leading to the axonal damage [1]. This damage disrupts the nervous system's ability to transmit signals, leading to physical signs and symptoms, and sometimes mental disorders. The disease often leads to disability and even cognitive decline. These physical and cognitive limitations can affect the quality of life of people with MS [2]. The MS atlas that is an open source global data compilation, and the availability of resources for people with MS reported at country, regional and global levels shows that the 2020 global prevalence is 35.9 (95% CI: 35.87, 35.95) per 100,000 people is 30% higher than in 2013. By 2020, it is estimated that the number of people with MS worldwide has increased to 2.8 million [3]. More unfortunately, MS can cause significant mental and physical symptoms, notably muscle weakness, abnormal walking mechanics, balance problems, cognitive impairment, depression, fatigue and spasticity. Patients with MS frequently decrease physical activity for the fear of worsening the symptoms, which can result in reconditioning [4].
Some meta-analyses have shown that MS could exacerbate risks for incurring a variety of adverse medical end points. For example, compared to healthy controls, MS was significant associated with increased risk of social cognitive dysfunction [5]. A great many of results indicated the prevalence of depression and anxiety were increased in MS [6]. What's more serious is that MS may lead to patients' suicide risk, which makes us pay special attention to MS patients [7]. In addition to those, people with MS have an increased risk of developing any type of stroke and ischemic stroke in particular [8]. There are lots of articles showing that MS can affect many convenient human health, however, there is no systematic summary to evaluate the validity, breadth of the associations of MS with multiple health outcomes. Because the umbrella meta-analysis integrates existing systematic reviews and meta-analyses, and it has the potential to provide evidence of the highest quality if properly performed and interpreted [9], we conducted this study that integrated existing studies and systematically evaluated the recorded associations between MS and medical end-points. We believe that this article may help to improve the understanding of MS relation to other health problems and also raise awareness of MS.
We have registered a protocol in PROSPERO (CRD42022323620). The study was conducted based on Preferred Reporting Items from Systematic Reviews and Metaanalyses (PRISMA) regulations [10].
Literature search
Two reviewers searched PubMed, Web of science and Embase in duplicate, using the search term: (Multiple sclerosis (title/ abstract)) and (meta-analys*(title/abstract)), from inception to 2022/4/6 and limited the search to humans and English language, as the vast majority of reviewed studies are published in English language, peer reviewed journals. Any discrepancies were evaluated and resolved by a third reviewer.
Study selection
Articles that met the following criteria were included:
• Meta-analyses of observational studies (cohort, case-control,
and cross-sectional studies) with quantitative analysis.
• Meta-analyses of observational studies that evaluate the
associations of MS with any medical end-points in humans.
• Participants are not limited by age, sex, race, region, or health
status.
• The studies were in English.
Articles that met the following criteria were excluded:
• Letters, conference abstracts, and research protocols.
• Studies are only reviews.
• The studies involve animal research.
• Multiple sclerosis is not the exposure of interest.
When multiple meta-analyses investigated the same health outcomes, we selected the study containing the largest number of primary studies or the most recent study.
Data extraction
Two researchers (LS and LZ) extracted the information independently form the included studies.
We extracted the following information: Name of first author, publication year, health outcomes, study design (case-control, cross-sectional, or cohort studies), number of studies included in each meta-analysis, number of participants and events, type of metric (RR, relative risk; OR, odds ratio; HR, Hazard Ratio; SMD, Standardized Mean Difference; g, hedges’g ), summary effect size, 95% Confidence Interval (CI) of the results, P-values for statistically significant level, Q-test and Egger’s test.
Data analysis
We used the extracted data obtained from the eligible studies to re-analyze each meta-analysis. If the data we want was missing, we tried our best to find the raw data to calculate the value and the summary effect size and its 95% CI were all re-estimated. We used I2 metric and Cochran’s Q-test to evaluate the heterogeneity. When the I2 is greater than 50%, we choose the random effect model; otherwise, we choose the fixed effect model. We also calculated the P value of the publication bias using Egger’s test. P<0.1 for heterogeneity and publication bias were considered statistically significant. All differences that arose during the extraction process with a third person (ST).
Assessment of methodological quality and epidemiologic evidence quality
We applied A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR2), a robust and validated tool, to assess the methodological quality of each included study. AMSTAR2 contains 16 items, seven of which are key items, and it classifies the study quality into four ranks as following: Critically low, low, moderate and high [11]. To evaluate the evidence quality of the association between MS and each health outcomes, grading parameters that have been adapted in various researches were used in this study [12-14].
According to the criteria (precision of the estimate, number of cases, heterogeneity and small study effects), the strength of epidemiologic evidence was categorized into high, moderate, weak or not applicable. The above assessment process was independently completed by LS and LZ.
Search result
The flowchart of study selection process for our umbrella metaanalysis was showed in Figure 1. Overall, a total of 3111 articles were identified form three databases (1112 articles from PubMed, 631 form Web of science, and 1368 from Embase). After excluding 1490 duplicates, we read the title and abstract of each citation carefully, and then retrieved the full text of the article that might meet the reading requirements. On the basis of the inclusion and exclusion criteria, we found the remaining 54 articles with full-text available. Because 26 articles with identical outcomes were not the most included studies, we excluded them and 28 eligible articles with 84 unique health outcomes were remained finally. All 28 articles were published between 2006 and 2022. The characteristics of these metaanalyses were all shown in Supplementary Table 1. Health outcomes due to MS were involved to following categories of diseases: digestive diseases (n=3), cardiovascular diseases (n=7), infectious diseases (n=8), allergic diseases (n=4), skeletal system disorders (n=13), immune and metabolic diseases (n=5), cognitive affective disorders (n=18), serum marker disorders (n=14), other outcomes (n=12) (Figure 2).
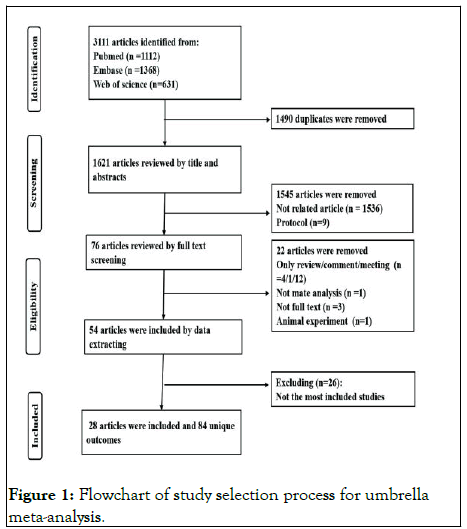
Figure 1: Flowchart of study selection process for umbrella meta-analysis.
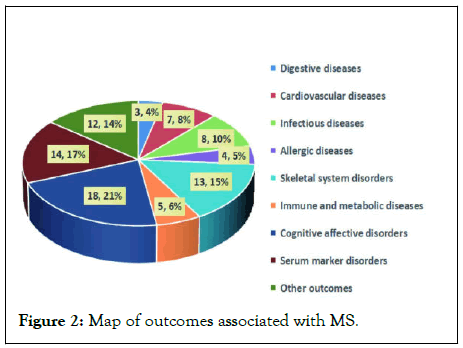
Figure 2: Map of outcomes associated with MS.
Digestive diseases
The adverse effects of MS on digestive diseases are presented in Supplementary Table 1. We observed three digestive diseases were linked to MS. Previous data indicated that MS increased risk of IBD, UC and CD [15,16].
Cardiovascular diseases
MS was significantly associated with an increased risk for myocardial infarction, heart failure, any type of stroke and ischemic stroke in particular. We found no difference for ischemic heart disease, bradycardia and preeclampsia in MS or without MS. But the risk of atrial fibrillation was lower in MS (Supplementary Table 1) [17,18].
Infectious diseases
This study has showed that MS had significant relationship with an increased risk for Human Herpes Virus 6 (HHV6) infections, Herpes Simplex Virus (HSV) infection and Chlamydia pneumonia [19-21]. In Asian countries, Varicella-Zoster Virus (VZV) infection was more common in MS patients than in controls, but no significant association was found in European countries. Cytomegalovirus (CMV) infection was lower among people with MS than controls in Europe. On the contrary, CMV was more common in MS patients than in controls from the Middle East region and there was no significant association in North America (Supplementary Table 1) [22-23].
Allergic diseases
The data showed that there is no evidence to support the connection between allergic diseases, asthma, allergic rhinitis, eczema and MS (Supplementary Table 1) [24].
Skeletal system disorders
MS was associated with an increased risk for tibia fracture risk, femur fracture risk, hip fracture risk, pelvis fracture risk, humerus fracture risk, and vertebrae fracture risk, but not for ribs and radius/ulna. The study suggests that MS patients have reduced overall BMD compared with healthy controls (Supplementary Table 1) [25,26].
Immune and metabolic diseases
An increased risk of between MS and type 1 diabetes, diabetes and hypothyroidism were observed in this study. But MS was not related to either Systemic Lupus Erythematosus (SLE) or Rheumatoid Arthritis (RA) (Supplementary Table 1) [27].
Cognitive affective disorders
There was no difference between Progressive Primary MS (PPMS) and secondary progressive MS in overall ToM, cognitive ToM, affective ToM, and facial emotion recognition. However, patients with Relapsing-Remitting MS (RRMS) had more serious defects in facial emotion recognition. PPMS patients showed significantly more cognitive impairment in almost all cognitive domains: in particular, verbal learning and all measures of verbal memory discriminated between PPMS and RRMS, whereas no significant differences emerged for either anxiety and depression or fatigue (Supplementary Table 1) [28,29].
Serum marker disorders
MS had higher serum levels of homocysteine, malondialdehyde and lipid hydroperoxide by tert-butyl hydroperoxide-initiated chemiluminescence (CL-LOOH) compared with control groups. In contrast, concentrations of albumin were significantly decreased in MS patients when compared to HC subjects. We found no associations between MS and advanced oxidation protein product, total oxidative status, total antioxidant status, copper, cholesterol superoxide dismutase, glutathione, uric acid, vitamin B12 and folate (Supplementary Table 1) [30,31].
Other outcomes
MS was related to an increased risk of suicide, primary headaches, vitiligo, female sexual dysfunction, restless legs syndrome, psoriasis. The risk of cancer in patients with MS was lower than the general population. There was no association between traumatic injury and multiple sclerosis. People with MS had greater center of mass displacements and longer response times and had significantly worse reactive balance than healthy controls (Supplementary Table 1) [32-39].
Heterogeneity
Among 84 included meta-analyses, we could not re-analyze the heterogeneity for 11 meta-analyses due to lack of detailed data from original studies. Twenty-seven meta-analyses showed low heterogeneity (I2%<50%), while the remaining 48 show high heterogeneity (I2>=50%) in our study (Supplementary Table 1).
Publication bias
Eight (9%) of the 84 included meta-analyses had significant publication bias, 61 (73%) studies did not show significant publication bias and 15 (18%) studies did not appear publication bias due to insufficient number of studies (Figure 3).
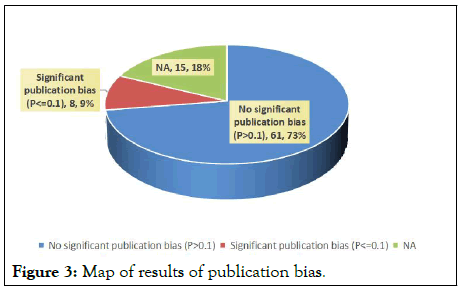
Figure 3: Map of results of publication bias.
AMSTAR2 and strength of epidemiologic evidence
We observed that there had no high/moderate methodological quality according to the strict AMSTAR2 tool. Only 1 (4%) article was rated as low, with the other 27 (96%) articles were rated as critically low (Figure 4). The detailed information of 16 items in AMSTAR2 and the results of specific quality scores were shown in Supplementary Table 2.
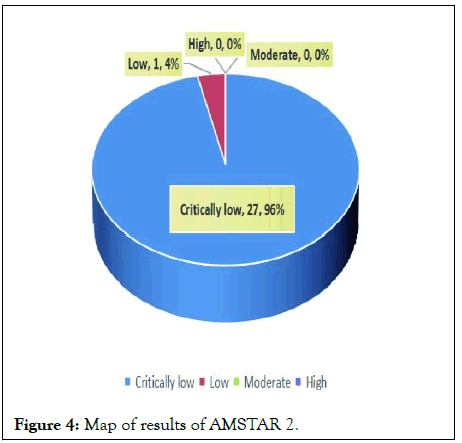
Figure 4: Map of results of AMSTAR 2.
According the criteria (Supplementary Table 3), the assessment of epidemiologic evidence was not applicable for 32 (38%) medical ramifications because the p-values for their summary effects were greater than 0.05. Among 52 significant medical ramifications, 6 (7%), 12 (14%) and 34 (41%) medical ramifications were rated as high, moderate and weak epidemiologic evidence, respectively (Figure 5).
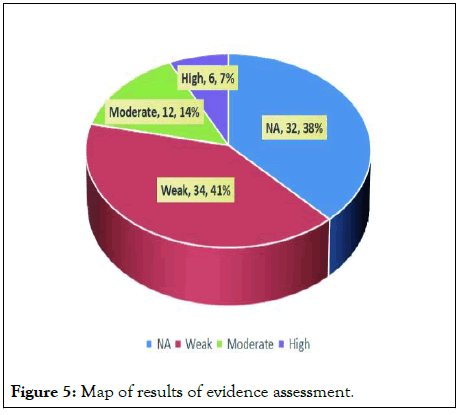
Figure 5: Map of results of evidence assessment.
Main findings and possible explanation
Our study included 28 articles that covered 84 health outcomes. The umbrella meta-analysis provided a broad overview of the current evidence of relationships between MS and digestive diseases, cardiovascular diseases, infectious diseases, allergic diseases, skeletal system disorders, immune and metabolic diseases, cognitive affective disorders, serum marker disorders, other outcomes. The results showed that MS increased the risk of 50 health/medical end points and reduced the risk of atrial fibrillation and cancer. However, only 6 (7%) health outcomes (increased risk of IBD, UC, CD, herpes simplex virus type 2- IgG, hypothyroidism and decrease the risk of atrial fibrillation) showed high epidemiologic quality evidence, 12 (14%) showed moderate level of evidence, 34 (41%) were rated as weak epidemiologic evidence.
As is known to all, MS is also a demyelinating disease of the central nervous system. Literature suggests that patients with IBD can present with demyelinating events in the central and peripheral nervous system [40]. A large number of studies shed light on the biological basis of comorbidity between MS and IBD. The interactions between autonomic dysfunction and the immune system, as well as the role of autonomic dysfunction in the pathogenesis and progression of MS have become a matter of increasing interest [41]. MS was considered as cause, of central origin, for autonomic dysfunction. Both MS and IBD are moderately heritable, with estimated liability-scale Single Nucleotide Polymorphism (SNP) heritability of 19% for MS and approximately 25% for IBD (27% for UC and 21% for CD). MS patients had a higher prevalence of IBD than controls (RR=1.53, 95% CI 1.38-1.70, p<0.00001). Our analysis found that MS offers harmful effect on IBD (included UC and CD) with high epidemiologic evidence. Another meta-analysis included ten observational studies about IBD (included UC and CD) was consistent with our findings [42-44].
Studies have shown that mice with the strain of type 2 Herpes Simplex Viruses (HSV-2) causes brief encephalitis associated with multifocal central nervous system demyelination [45]. MS might have a higher risk of HSV-2 infection and the exact mechanism remains to be further studied. MS has been described as the archetypal autoimmune disease of the central nervous system and the gene most strongly associated with MS is the HLA-DRB1*1501 MHC class II haplotype, and in the large scale genome wide association studies, and many other genes related to immune function, has been associated with multiple sclerosis [46]. The study of the risk of additional autoimmune diseases in both MS patients and their first degree relatives has been conducted for many years, with studies employing a variety of designs and yielding conflicting results [47]. Based solely on population based studies, thyroid disease (6.44%) was more prevalent autoimmune comorbidities, and the incidence of autoimmune thyroid disease in MS was increased, which was similar to our study [48-51].
Our study found the risk of atrial fibrillation was lower in MS (HR 0.7, 95% CI 0.6 to 0.8, I2 0%, n=354,070) with high quality of evidence. Although the sample size was large and nationwide, the association between atrial fibrillation and MS was only based on three cohort study. Therefore, the association between MS and atrial fibrillation should be interpreted with more caution. We speculated that the known risk factors (hypertension and cardiac value disease) for atrial fibrillation were less frequent in MS patients, which may be the possible explanation for the result.
In addition to discovering that MS can decrease the risk of atrial fibrillation, our research also found that the risk of cancer in patients with MS is less than the general population, even if rated as moderate evidence. One explanation for the lower risk of cancer in MS is anti-tumor immune-surveillance. The other explanation is shorter life spam of MS patients and smoking cessation at early stages of the disease. In theory, this could represent a genuine reduction in risk or “diagnostic neglect”, that cancer is undiagnosed when symptoms are misattributed to MS. A large amount of research and theory are needed to confirm this point of view.
However, in most meta-analyses, there is significant heterogeneity among studies. The following factors contributed to the heterogeneity of the included studies: Age, sex, geographical area, education, MS subtypes, disease duration and study design. The standards of methods implemented in all selected meta-analyses was categorized as “critically low” or “low”, and none was grade as high/moderate based on the AMSTAR2 criteria. The following reasons may be responsible for the above mentioned results: Without a pre-recognized explicit statement/protocol, a list of excluded studies, funding source details of primary studies and report of potential sources for conflicts of interest, and heterogeneity observed in the metaanalysis.
As we know, this is the first critical assessment of the scope and validity of reported relationships between MS and various health outcomes. We applied robust search term to identify eligible articles in three databases to ensure the research result as far as possible and reasonable. Then, two authors independently screen the articles and extract the data form eligible studies. At the same time, AMSTAR2 tool and a strong evaluation method of evidence were used to assess the quality of methodology and the epidemiologic evidence. We believe that this work can improve the understanding of MS to provide a strong scientific basis.
Notwithstanding, some limitations and defects inevitably existed in this study. Firstly, we conducted the study based on the published studies with the largest number of included primary studies, but some individual studies might be too small or missed, failed completely to find the full text and under developed meta-analysis were beyond the scope which could affect the results, such as the concentration of pregnancy outcome. Secondly, due to lack of raw data, most of the metaanalyses failed to be conducted subgroup analyses. For example, the meta-analysis shows MS had an increased risk of suicide, but sex, ethnic and geographical differences were not considered. The proportion of suicide was found to be significantly higher among females and those aged 18 years-25 years [52]. What calls for special attention is that are disease subtype and regional problems. Cytomegalovirus (CMV) infection was lower among people with MS than controls in Europe. In contrast, CMV was more common among MS patients compared to controls in the Middle East region and there was no significant association in North America [53]. An international group of MS experts, the MS phenotype group, recently revised the multiple sclerosis phenotypic classifications and issued their recommendations in 2014. Recent research developments have helped improve the accuracy of multiple sclerosis diagnosis. There was no way to perform subgroup analyses to provide more reliable and accurate results due to the lack of data. Thirdly, the study extracts data of Hedges'g, which is different with general umbrella meta-analysis. Due to small sample size, we should expand the sample size to increase credibility. Finally, this study only included the publications in English, caused some outcomes may have been overlooked, which may increase the selection bias.
In a word, this study provided a detailed evaluation of all available data on links between MS and various health/medical end points. The results showed that MS increased the risk of 5 health/medical end points and reduced the risk of atrial fibrillation. Considering that evidence for most outcomes were categorized as “moderate” and “weak,” additional high quality prospective cohort studies are required in order to draw a powerful, persuasive conclusion.
None.
The authors would like to acknowledge all authors of the original studies that were included in this meta-analysis.
The study does not involve animal subjects or human participants and no ethical approval was required.
The authors declare no conflicting interests.
The data used to support the findings of this study are included in the article/supplementary material, further inquiries can contact to the corresponding author.
The authors’ responsibilities were as follows-LS, FL, LZ, LL, SC, and ST contributed to the conception and design of the study; LS, LL, SC and ST drafted the manuscript; LS, LZ, LL and SC were involved in statistical analysis; LS and FL interpreted the results; ST supervised the whole process; All authors read and approved the final manuscript.
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Schloar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shen L, Long F, Zhong L, Chen S, Li L, Tang S (2024) Multiple Sclerosis and Health Outcomes: A Comprehensive Analysis Based on Observational Meta-Analyses. Immunogenet Open Access. 9:228.
Received: 05-Apr-2023, Manuscript No. IGOA-23-23278; Editor assigned: 07-Apr-2023, Pre QC No. IGOA-23-23278 (PQ); Reviewed: 21-Apr-2023, QC No. IGOA-23-23278; Revised: 23-Apr-2024, Manuscript No. IGOA-23-23278 (R); Published: 30-Apr-2024 , DOI: 10.35248/IGOA.24.9.228
Copyright: © 2024 Shen L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.<