Virology & Mycology
Open Access
ISSN: 2161-0517
ISSN: 2161-0517
Case Report - (2022)Volume 11, Issue 2
Mycobacterial spindle cell pseudotumor is a rare entity occurring in immuno-compromised patients mostly with acquired immunodeficiency syndrome, organ transplant and immuno-suppressive therapy. It occurs in various body sites and most commonly non-tuberculous mycobacteria are the causative agent followed by Mycobacterium tuberculosis. It is characterized by proliferation of spindle shaped histiocytes with acid fast bacilli. It histologically mimics spindle cell neoplasms including Kaposi’s sarcoma. We present a case of Mycobacterial spindle cell pseudotumor in an immuno-compromised patient with peritoneal mass and discuss the characteristic findings.
Mycobacteria; Histocytes; Spindle cell tumor
MSP: Mycobacterial Spindle cell Pseudotumor; HIV: Human Immunodeficiency Virus; NTM: Non- Tuberculous Mycobacteria; AFB: Acid Fast Bacilli; ATT: Antituberculosis Therapy; LFTs: Liver Function Tests; GGT: Gamma Glutamyl Transferase; SGPT: Serum Glutamic-Pyruvic Transaminase; ICU: Intensive Care Unit; HCT: Hematocrit; MCV: Mean Corpuscular Volume; WBC: White Blood Cell; ZN: Ziehl-Neelson; AIDS: Acquired Immunodeficiency Syndrome; KS: Kaposi Sarcoma
Mycobacterial Spindle cell Pseudotumor (MSP) is characterized by localized proliferation of spindle shaped histiocytes colonized by acid fast mycobacteria [1]. It most commonly involves lymph nodes, but, extranodal sites including skin, lungs, brain and other visceral organs are on record [2,3]. It occurs in immunocompromised states mostly in Human Immunodeficiency Virus (HIV) infection but non-HIV related immunocompromised states also predispose to this condition [1-5]. MSP clinically and pathologically resembles mesenchymal tumors especially Kaposi Sarcoma [2,4-7]. Both Non-Tuberculous Mycobacteria (NTM) and tuberculous mycobacteria are responsible for this condition [1]. Most common pathogen is Mycobacterium avium intracellulare complex followed by tuberculous mycobacteria [4-6]. We present a case of MSP in peritoneum due to tuberculous mycobacteria in an immunocompromised patient. Histopathologically the lesions were composed of spindle and epithelioid histiocytes, small foci of necrosis, and numerous Acid-Fast Bacilli (AFB) consistent with mycobacterial spindle cell tumor.
Ethical review
The individual case report does not require approval from institutional review board of ethical committee hence ethical review was not obtained. The consent from the patient’s guardian was obtained for the complete anonymity of his identity.
A male patient 22 years old presented in emergency in June 2021 with complaints of generalized weakness, lethargy, vomiting, weight loss about 25-35 Kilograms, irritability and aggressive behavior for last four months. He was diagnosed on presumed grounds from other hospital as abdominal Tuberculosis two months ago before presenting to our hospital. Anti-Tuberculous Therapy (ATT) 3 drug regimen was started. He took ATT for two months. Later the patient came with drug induced toxicity as shown on deranged LFTs (Total bilirubin 5.10 mg/dl, direct bilirubin 4 mg/dl, GGT 90 U/L, SGPT 62 U/L). He was unable to take orally and was drowsy so he was admitted in medical ICU. On examination he was cachectic and severely malnourished. Vitally he was stable and blood pressure was 100/68 mmHg, temperature was 37oC , pulse was 98/ minute and respiratory rate was 24/minute. At the time of admission his complete blood count showed hemoglobin 9.2 gm/dl, HCT: 26.6%, MCV: 84 fL, WBC: 4.3 × 103/µl. Differential leukocyte count showed neutrophils 83.1%, lymphocytes 6.3%, monocytes 4.9%, eosinophil’s 4.1% and basophils 1.6%. His CD4 count was 153 cells/µL (normal 430-1740 cells/µL); serum potassium was 1.5 mEq/L. He was started on second line ATT and was managed conservatively and remained admitted in hospital for ten days. After 12 days he again came to ER with severe abdominal pain, altered sensorium and lethargy. Examination was suggestive of tender distended abdomen. General surgery team was taken on board and he underwent complex laparotomy. There were multiple and complex adhesions between grossly diseased bowel loops and omentum. Tissue from peritoneal nodule was sent for histopathological examination. Samples from peritoneal pus were also sent for GeneXpert and microscopy. GeneXpert showed Mycobacterium tuberculosis and AFB smear from peritoneal pus showed 20 AFB on fluorescent staining. Patient also tested positive for COVID 19 and later the patient died on next day of admission. Histopathologically the lesions were composed of spindle and epithelioid histiocytes admixed with lymphoplasmacytic infiltrate as shown in Figure 1 ill-defined granulomas in Figure 2, small foci of necrosis in Figure 3. Immunohistochemical stains ASMA (Alpha Smooth Muscle Actin) and desmin were focally positive and CD68 highlighted sheets of histiocytes. Ziehl Neelson (ZN) stain and modified Ziehl Neelson (ZN) stain revealed numerous acid fast bacilli were showed in Figures 4 and 5. It was diagnosed as mycobacterial spindle cell pseudotumor.
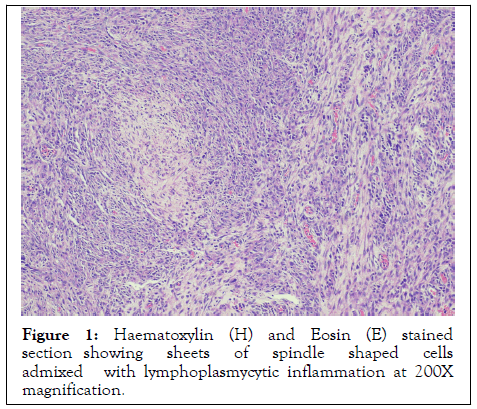
Figure 1: Haematoxylin (H) and Eosin (E) stained section showing sheets of spindle shaped cells admixed with lymphoplasmycytic inflammation at 200X magnification.
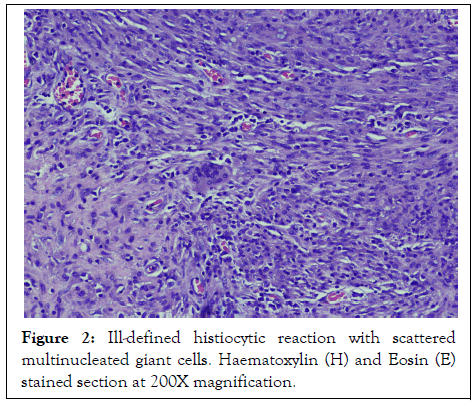
Figure 2: Ill-defined histiocytic reaction with scattered multinucleated giant cells. Haematoxylin (H) and Eosin (E) stained section at 200X magnification.
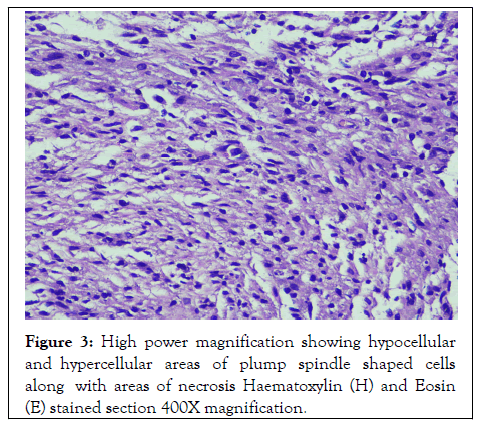
Figure 3: High power magnification showing hypocellular and hypercellular areas of plump spindle shaped cells along with areas of necrosis Haematoxylin (H) and Eosin (E) stained section 400X magnification.
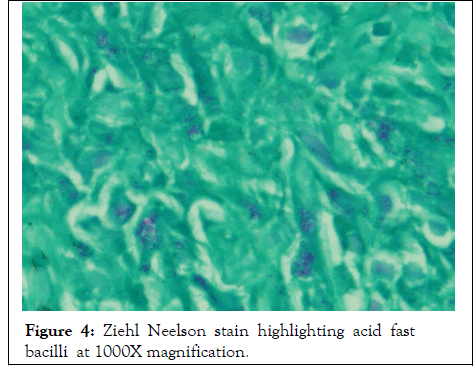
Figure 4: Ziehl Neelson stain highlighting acid fast bacilli at 1000X magnification.
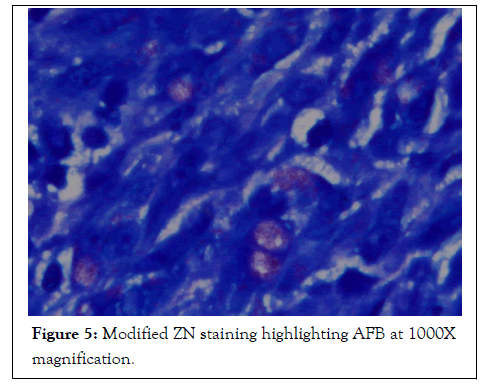
Figure 5: Modified ZN staining highlighting AFB at 1000X magnification.
MSP is a rare condition and benign reactive lesion caused by both tuberculous mycobacetria and Non-Tuberculous Mycobacteria (NTM) [1]. Different case reports have been reported in literature in various sites of the body which includes both nodal and extranodal sites. Among the reported sites for MSP includes skin, lymph nodes, spleen, appendix, bone marrow and brain. It mostly occurs in immunocompromised states which include HIV, diabetes mellitus, solid organ transplants, bone marrow transplant and immunosuppressive therapy. The first patient of MSP reported in literature presented with progressive swelling in hand in 1985 that underwent a cardiac transplant. Mycobacterium avium intracellulare complex was the causative pathogen identified in this case [7].
We present a case of a young male, who was suspected of having immunocompromised disease so HIV screening and CD 4 cell count was done. HIV was non-reactive on screening serological test but CD 4 cell count was significantly low. He also had persistently low lymphocyte count. In current case report, the causative agent identified was Mycobacterium tuberculosis which is a rare cause of MSP. Previously tubercular MSP has been reported in an Acquired Immunodeficiency Syndrome (AIDS) patient who presented with generalized lymphadenopathy. Biopsy of the lymph node showed spindle shaped histiocytes with numerous acid fast bacilli [4]. Another case of MSP caused by Mycobacterium tuberculosis has been reported in renal transplant patient who was on immunosuppressive therapy and cutaneous MSP was diagnosed in this patient [3]. Xiaoyan et al. reported MSP caused by Mycobacterium tuberculosis in lymph node of 45 years old male patient newly diagnosed with AIDS8. It is mainly characterized by spindle shaped proliferation of histiocytes [6].
MSP closely resembles mesenchymal tumors particularly Kaposi Sarcoma (KS), other differential diagnoses include nodular fasciitis, benign fibrous histiocytoma, inflammatory myofibroblastic tumor, inflammatory pseudotumor, follicular dendritic cell sarcoma, spindle cell melanoma, myogenic or neural proliferations and neuroendocrine tumors [9,10].
Therefore it has to be distinguished as all these pathologic conditions have different clinical courses, treatment and outcomes1. Acid fast stain can reliably distinguish between these conditions and MSP [10]. The main features present in KS include more compact and larger fascicles which have slit like spaces present in between the cells, spindle cell proliferation, nuclear pleomorphism and increased number of mitosis [9]. Extravasated RBCs are also associated with KS. In contrast, MSP is characterized by loose storiform pattern of plump spindle shaped histiocytes having eosinophilic to granular cytoplasm. Granulomatous inflammation may or may not be present. Immunohistochemical stains can also help to distinguish between these conditions. CD68 and S100 are positive in histiocytes in MSP2, however S100 has variable staining and it can be negative. Spindle cells in MSP also express smooth muscle actin and variable desmin. KS cells stain positive with CD34 and CD31 markers. Douglas et al. reported a case of MSP in abdominal wall where patient was on continuous steroid therapy due to stem cell transplant and causative agent was Mycobacterium abscessus [9]. Another case of MSP in appendix has been reported where patient was immunocompromised due to AIDS and the exact species of mycobacteria could not be determined in this case as the patient died of AIDS complications however numerous AFB were seen on ZN staining [2].
In conclusion the MSP should not be missed and one should list this in differential diagnosis along with other tumors of mesenchymal cells in patients who have the conditions which affect their immune status4. MSP should be differentiated from other histologic mimics by special stains and immunohistochemical studies on tissue biopsy. MSP is a treatable non-neoplastic entity; it should be included in the differential diagnosis of spindle cell tumors especially in immunosuppressed patients.
Citation: Zafar A, Yaqoob N, Naveed H, Shah R, Jamal S (2022) Mycobacterial Spindle Cell Pseudotumor Presenting as Peritoneal Masses in a Suspected Case of Human Immunodeficiency Virus. Virol Mycol. 11:226.
Received: 25-Feb-2022, Manuscript No. VMID-22-16380; Editor assigned: 01-Mar-2022, Pre QC No. VMID-22-16380 (PQ); Reviewed: 15-Mar-2022, QC No. VMID-22-16380; Revised: 22-Mar-2022, Manuscript No. VMID-22-16380 (R); Published: 29-Mar-2022 , DOI: 35248/2161-0517.22.11.225
Copyright: © 2022 Zafar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.