Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2024)Volume 12, Issue 12
Objective: Systematic evaluation of the effect of neuromuscular electrical stimulation in the prevention of deep vein thrombosis in patients, providing evidence-based medicine for clinical prevention of venous thrombosis.
Methods: A computerized search of PubMed, The Cochrane Library, Web of Science, and Embase was performed to collect published literature on the prevention of the development of Deep Vein Thrombosis (DVT) in patients with Neuromuscular Electrical Stimulation (NMES), with a timeframe of from the time of library construction to August 2024. Literature screening, data extraction, and quality assessment were performed independently by two investigators according to the inclusion and exclusion criteria, and then Meta-analysis was performed using RevMan 5.4 software.
Results: A total of 11 papers with 1040 study subjects were included. Meta-analysis showed that NMES could reduce the incidence of DVT (Risk Ratio (RR)=0.55, 95% Confident Interval (CI): (0.43, 0.70), p<0.00001), accelerate venous blood flow in the lower extremities Mean Difference (MD=6.27, 95% CI (2.64, 9.91), p=0.0007), however, there is insufficient evidence of improvement in D-dimer (DD) levels.
Conclusion: Neuromuscular electrical stimulation can prevent DVT in patients, but the quality level of the literature is not high, and high quality clinical studies are still needed to further validate and analyze its efficacy.
Deep vein thrombosis; Meta-analysis; Neuromuscular electrical stimulation; Venous thrombosis
DVT is an abnormal clotting of blood in the deep veins due to various reasons, which in turn affects the venous blood return obstacle disease, mostly in the lower limbs [1]. Thrombus dislodgement to the lungs can cause Pulmonary Embolism (PE), DVT and PE are collectively known as Venous Thromboembolism (VTE), which are two manifestations of the same disease in different locations and at different times, it is the third most common cardiovascular disease after myocardial infarction and stroke, it is also one of the leading preventable causes of death in hospitalized patients [2-5]. The main adverse consequences of DVT are PE and post-thrombotic syndrome, which can severely reduce patients' quality of life and even cause severe organ dysfunction and death. VTE has a high morbidity and lethality rate among hospitalized patients, prevention is particularly important, and active and effective prevention is an important line of defense in safeguarding the lives of patients [6].
At present, DVT prevention is mainly carried out in three aspects, namely, basic prevention, drug prevention and mechanical prevention. Basic prevention includes encouraging patients to do exercises such as ankle pump exercise and straight leg raising exercise, paying attention to diet, and keeping stools usually, etc. However, these preventive activities are difficult to attract patients' attention, and surveys show that patients' adherence to or implementation of such preventive methods is relatively low; drug prevention, although it has a better preventive effect, needs to be taken into consideration.
Although drug prevention has a better preventive effect, it needs to take into account the risk of bleeding, which leads to a part of patients to reduce the dosage of medication or the existence of contraindications to the use of medication, thus failing to achieve the preventive effect, which leads to the existence of certain limitations of drug prevention; Mechanical prophylaxis, which has an exact VTE prevention effect and does not increase the risk of bleeding in patients, plays a pivotal role in clinical practice, such as Intermittent Pneumatic Compression (IPC), Gradient Compression Stockings (GCS), and Plantar Phlebotomy Pumps (VFP) have been recommended by domestic and international guidelines, and in recent years, Neuromuscular Electrical Stimulation (NMES) has entered the public eye as a new type of mechanical prophylaxis with high safety, patient acceptance and compliance [7]. NMES has entered the public eye in recent years as a new type of mechanical prophylaxis with high safety, patient acceptance, and compliance, and has entered clinical use at home and abroad. However, there is a lack of systematic evaluation of the effect of NMES in venous thrombosis prevention, and this study provides an in-depth analysis and comparison of the effect of NMES to provide an evidence-based medical basis for clinical prevention of venous thrombosis.
Study selection
Studies included were Randomized Controlled Trials (RCTs) published in English or Chinese. Participants were adults aged 18 or older, without a history of VTE, and excluding those with hemodynamic instability or severe organ dysfunction. The experimental group received NMES or NMES combined with a control program, while the control group received routine care or other nursing treatments. The primary outcome was the incidence of DVT, and secondary outcomes included venous blood flow velocity and D-dimer levels.
Inclusion criteria: 1: Study type: publicly published RCT, language limited to Chinese and English; 2) Study subjects: patients aged ≥ 18 years and without VTE, excluding hemodynamic instability and severe organ dysfunction; 3) Intervention: NMES or NMES combined with control group program was adopted in the experimental group, and routine care or other nursing treatment was adopted in the control group; 4) Outcome indicators: the primary outcome indicator was the incidence of DVT, and the secondary outcome indicators included venous blood flow velocity and DD.
Exclusion criteria: 1) Repeatedly published literature; 2) Review, case reports; 3) Literature for which the full text was not available or the above outcome indicators were not reported.
Data sources and search strategy
Computerized searches were conducted in PubMed, The Cochrane Library, Web of Science, and Embase, with a timeframe of 2024. Subject and free word searches were conducted with the search terms “Electric Stimulation/ Electrical Stimulation/ neuromuscular electrical stimulation/NMES” “Thrombosis/Thromboses/Thrombus/Venous Thrombosis/ Venous Thromboses/ Phlebothrombosis/ Phlebothromboses/ Deep Vein Thrombosis / Deep Vein Thromboses/ Deep Venous Thrombosis/ Deep Venous Thromboses/DVT”. Taking PubMed as an example, the specific search strategy is shown in Figure 1.
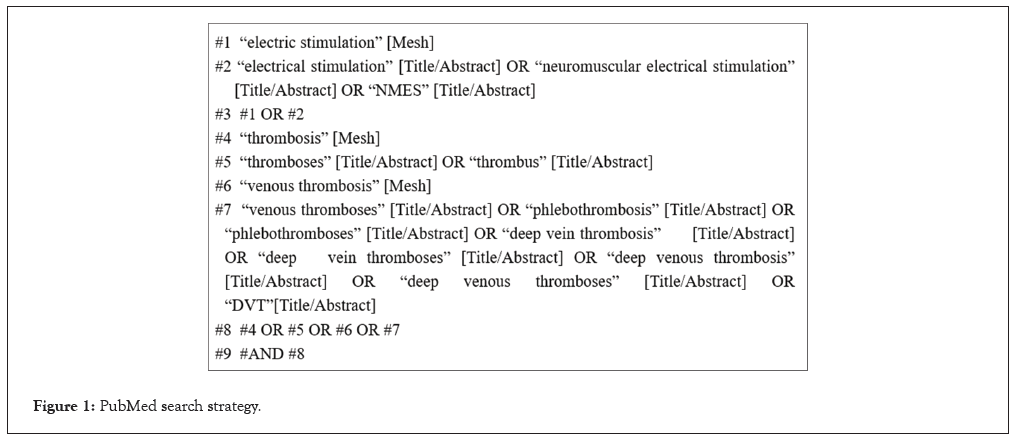
Figure 1: PubMed search strategy.
Literature screening and data extraction
All the literature was imported into NoteExpress software, and according to the inclusion and exclusion criteria, two researchers read the title and abstract respectively for initial screening, and then read the full text of the eligible literature for re-screening, and if there was any disagreement, it could be judged through discussion or the assistance of the third researcher.
Data extraction: 1) Basic information: first author, time of publication; 2) Basic characteristics of the study population: grouping method, sample size, age, gender, and intervention; 3) Outcome indexes of interest: The primary outcome index was the incidence of DVT, and the secondary outcome indexes included venous blood flow velocity and DD. After data extraction was completed, cross-checking was performed by two researchers.
Literature quality assessment and risk of bias
The methodological quality of the included studies was evaluated independently by two investigators, with discussion or a third investigator assisting in judgment when there was disagreement in the evaluation. The Cochrane Handbook 5.1.0 was used for quality evaluation of randomized controlled studies.
Statistical analysis
Meta-analysis was performed using RevMan 5.4 software. Relative Risk (RR) was used as the effect analysis statistic for count data and its 95% CI was provided; MD or Standard Mean Difference (SMD) and 95% CI were used as the statistical effect measures for continuous data. When testing for heterogeneity, if there was no significant heterogeneity between the results of each study (p ≥ 0.05, I²<50%), a fixed-effects model was used for Meta; if there was significant heterogeneity between the results of each study (p<0.05, I² ≥ 50%), a random-effects model was used for Meta-analysis. Obvious clinical heterogeneity was analyzed using subgroup analysis or descriptive analysis only. Funnel plots were used to evaluate the presence of publication bias.
Literature screening process and results
A total of 1608 relevant literatures were searched. After initial screening, elimination of duplicates, and re-screening, 11 pieces of literature were finally included. The literature screening process is shown in Figure 2.
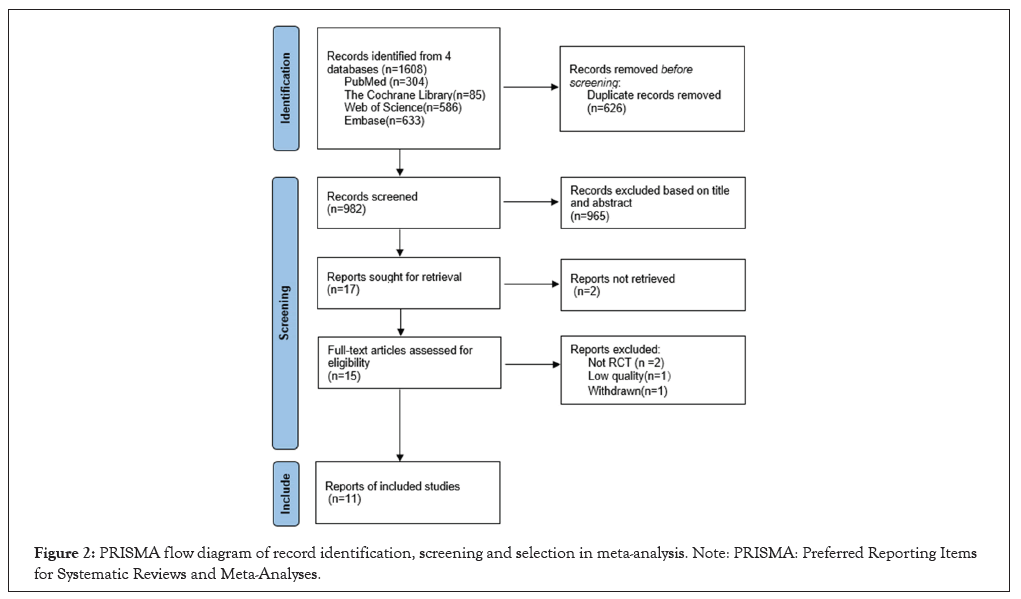
Figure 2: PRISMA flow diagram of record identification, screening and selection in meta-analysis. Note: PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Basic characteristics of included studies and results of risk of bias evaluation
The basic characteristics of the included studies are shown in Table 1, and the results of the risk of bias evaluation are shown in Figure 3.
| Study | Design | Sample T/C | Age | Gender(M/F) | Intervention | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | ||||
| Calbiyik et al. [8] | RCT | 32/32 | 62.0 ± 14.2 | 61.5 ± 12.4 | 15/17 | 16/16 | NMES+LMWH | NMES+ressure bandage | 2,3 |
| Chen et al. [9] | RCT | 29/29 | - | - | - | - | NMES+IPC | IPC | 1,2,3 |
| Xiao-qi et al. [10] | RCT | 38/38 | 58.39 ± 12.29 | 58.79 ± 12.11 | 21/17 | 23/15 | NMES+general nursing | general nursing | 1,3 |
| Wainwright et al. [11] | RCT | 14/11 | 68.50 ± 8.97 | 66.82 ± 10.03 | 5/9 | 4/7 | NMES | GCS | 1 |
| Yilmaz et al. [12] | RCT | 15/15 | 63.4 ± 5.91 | 63.86 ± 7.47 | 9/7 | 8/7 | NMES+LMWH+GCS | LMWH+GCS | 1,2 |
| Velmahos et al. [13] | RCT | 26/21 | 32 ± 15 | 45 ± 21 | 21/5 | 16/5 | NMES+general nursing | general nursing | 1 |
| Prevot et al. [14] | RCT | 75/75 | - | - | - | - | NMES+ general nursing | general nursing | 1 |
| Boström et al. [15] | RCT | 40/49 | 59 ± 1 | 60 ± 1 | 24/22 | 32/26 | NMES+Dextran | LMWH | 1 |
| Lindström et al. [16] | RCT | 37/40 | 63.7 | 66.5 | - | - | NMES+general nursing | general nursing | 1 |
| Rosenberg et al. [17] | RCT | 50/89 | - | - | - | - | NMES+general nursing | general nursing | 1 |
| Moloney et al. [18] | RCT | 113/172 | - | - | - | - | NMES+general nursing | general nursing | 1 |
Note: RCT: Randomized Clinical Trails; T: Test group; C: Control group; NMES: Neuromuscular Electrical Stimulation; LMWH: Low Molecular Weight Heparin; IPC: Intermittent Pneumatic Compression; GCS: Graduated Compression Stockings; 1: DVT incidence; 2: Peak femoral vein blood velocity; 3: D-Dimer
Table 1: Basic characteristics of included studies (n=11).
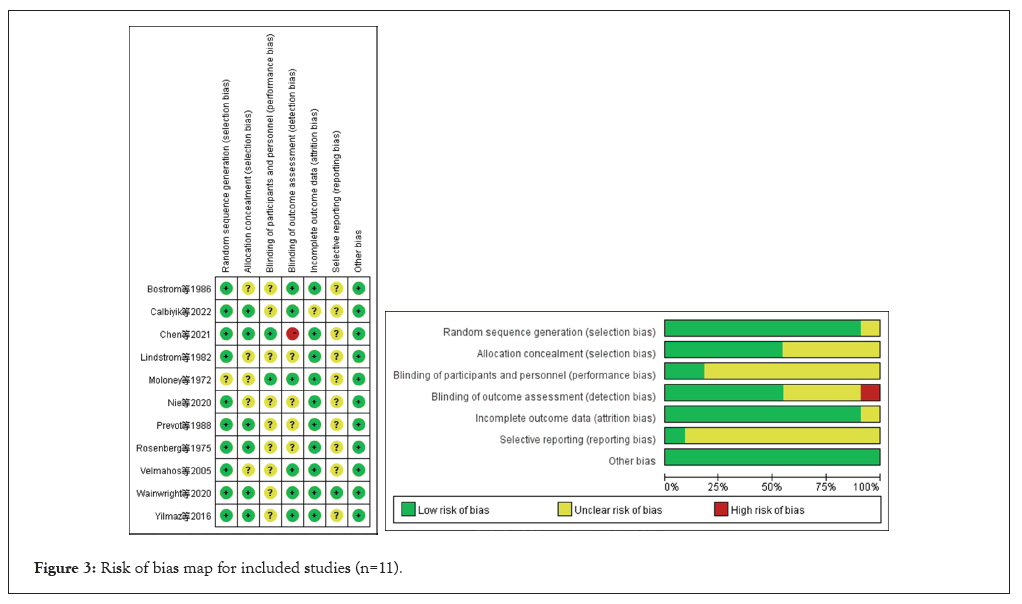
Figure 3: Risk of bias map for included studies (n=11).
Sensitivity analysis and publication bias
Mete analysis revealed high inter-study heterogeneity, and sensitivity analysis using the method of excluding single studies one by one revealed that there was still significant heterogeneity; therefore, this study explored the source of heterogeneity by conducting subgroup analysis based on different intervention protocols in the trial group. Because this study involved fewer than 10 articles, the risk of publication bias was not assessed.
Meta-analysis results
Incidence of DVT: Eleven studies used DVT incidence as an outcome indicator, with no significant heterogeneity among studies (I²=23%, p=0.24), and Meta-analysis using a fixed-effects model, with a statistically significant difference in the results of the combined effect sizes (RR=0.57, 95% CI (0.44, 0.74), p<0.0001), as shown in Figure 4.
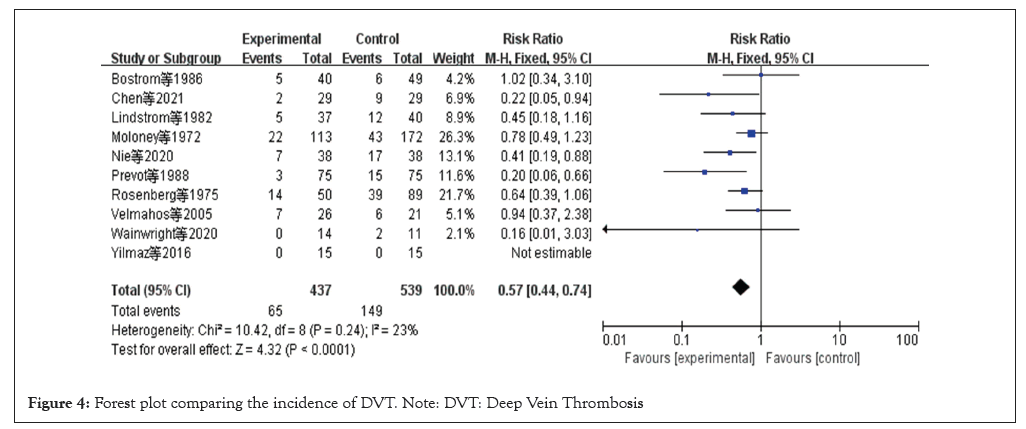
Figure 4: Forest plot comparing the incidence of DVT. Note: DVT: Deep Vein Thrombosis
Venous blood flow rate of the lower limbs: Three studies used venous blood flow rate as an outcome indicator, and there was significant heterogeneity among the studies (I²=89%, p=0.0001), adopting a random-effects model, as shown in Figure 5. Heterogeneity disappeared after the exclusion of Chen's study (I²=0%, p=0.39), and the possible reason analyzed was that the methods of blood flow rate measurement were different.
D-Dimer: Three studies used DD as an outcome indicator, with significant heterogeneity across studies (I²=99%, p<0.00001), and a random-effects model was adopted, with subgroup analyses grouped according to the different intervention protocols in the experimental group, as shown in Figure 6. The results show that only one study was included in each group, and only descriptive analyses were performed.
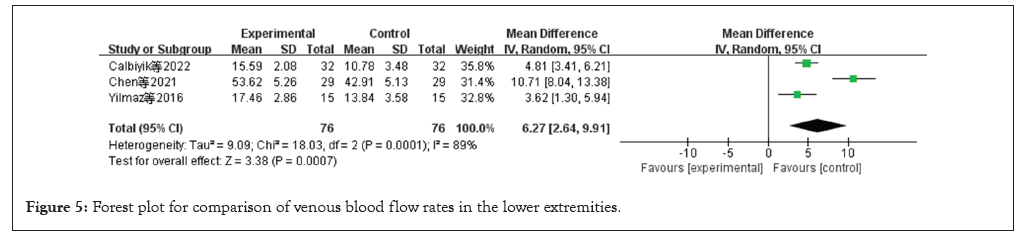
Figure 5: Forest plot for comparison of venous blood flow rates in the lower extremities.
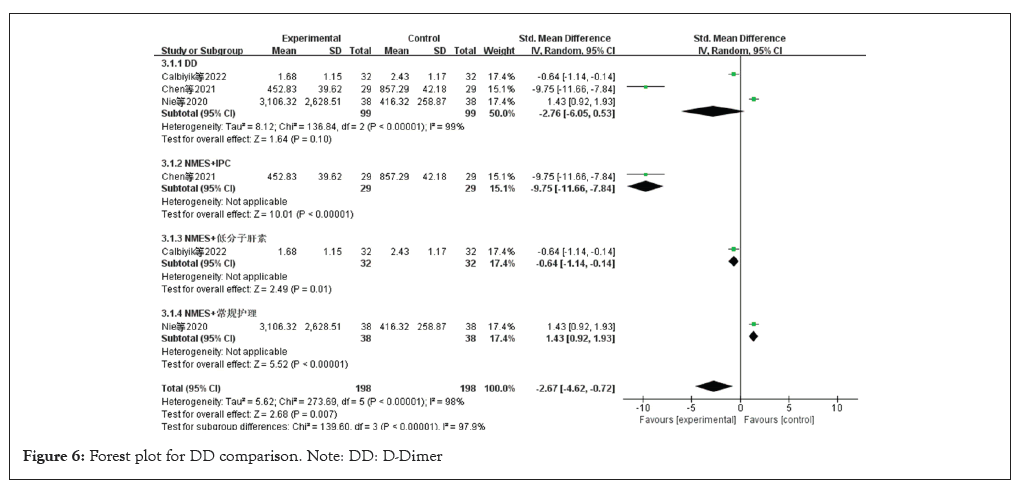
Figure 6: Forest plot for DD comparison. Note: DD: D-Dimer
Methodological quality of included studies
Eleven studies with 1040 patients were included. The interventions in the control group were intermittent pneumatic compression therapy and anticoagulant medication, and the interventions in the trial group were NMES or NMES combined with other prophylactic measures. The outcome indicators included DVT incidence, lower extremity venous blood flow rate D-dimer. The main conclusion was that NMES is effective in preventing lower extremity venous thrombosis in hospitalized patients. The quality of the literature was reviewed using the Cochrane Handbook tool and the results showed moderate quality. Patient baseline information was comparable in all studies (p>0.05).Five studies performed allocation concealment and ten studies used random number tables, computerized randomization. Some studies did not report the randomization method, allocation concealment and blinding in detail, which may have some bias.
Analysis of the effect of NMES on the prevention of lower extremity DVT in patients
The results of this Meta-analysis show that NMES can prevent the occurrence of DVT, accelerate the blood flow in the lower limbs and improve the coagulation function. Bedridden patients, especially critically ill patients, have increased the occurrence of DVT due to braking, trauma, surgery, invasive operations that affect blood flow in the lower limbs, causing endothelial damage and their own diseases that lead to blood in a hypercoagulable state. NMES works by utilizing the electrical excitability of the nerve cells, stimulating the nerves with pulsed current to cause the corresponding muscle contraction, increasing the venous blood flow rate [19]. At the same time, it can improve the coagulation function, D-dimer mainly reflects the function of fibrinolysis, high sensitivity, and its elevation indicates that there may be hypercoagulable state in the body, and the normal can basically exclude the VTE. The results of the present study show that NMES reduces the incidence of DVT, and significantly speeds up the femoral vein blood flow rate; as for D-dimer, only three studies reported DD results and there was significant heterogeneity, in both studies by Calbiyik et al., and Nie et al., NMES was found to be increased after intervention compared to pre-intervention and both were higher than normal, Chen's study showed that although there was a decrease in the NMES group and the NMES combined with IPC group after intervention compared to pre-intervention, the NMES group was still higher than the normal range. We found that, unlike the results of some existing studies, there is doubt and insufficient evidence that NMES reduces D-dimer, and more high-quality studies are needed [8,9].
NMES has a preventive effect on lower limb DVT in patients, and the clinical studies on NMES prevention of DVT in patients have been gradually increasing and gaining attention in recent years. The quality of the literature included in this study is moderate, and in the future, the study design can be continuously improved to reduce the risk of bias and further explore the mechanism of action of NMES in preventing DVT in patients and related therapeutic parameters.
This study's outcome metrics of lower extremity venous blood flow rate and DD are involved in a small body of literature.
Based on the findings of this study, Hospitals can introduce neuromuscular electrical stimulation devices for use in patients who need to prevent deep vein thrombosis in the lower extremities, providing a better option for DVT prevention.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Li Y, Ye L, Xu Z, Zhang S (2024). Neuromuscular Electrical Stimulation for the Prevention of Deep Vein Thrombosis in Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Angiol Open Access. 12:531.
Received: 25-Nov-2024, Manuscript No. AOA-24-35400; Editor assigned: 28-Dec-2024, Pre QC No. AOA-24-35400 (PQ); Reviewed: 12-Dec-2024, QC No. AOA-24-35400; Revised: 19-Dec-2024, Manuscript No. AOA-24-35400 (R); Published: 26-Dec-2024 , DOI: 10.35841/2329-9495.24.12.531
Copyright: © 2024 Li Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.