Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Review Article - (2016) Volume 6, Issue 3
Intravenous nitrates are widely used in the management of acute heart failure syndrome (AHFS), yet with lack of robust evidence to support their use. We therefore sought to analyse all randomised studies that evaluated the effects of nitrates on clinical outcomes in patients with AHFS. In total, fifteen relevant trials comparing nitrates and alternative interventions in 1824 patients were identified. All but three were conducted before 1998. No trials demonstrated a beneficial effect on mortality, apart from one trial reporting a reduction in mortality, which was related to the time of treatment. Retrospective review suggests that there is a lack of data to draw any firm conclusions concerning the use of nitrates in patients with AHFS, which is surprising given the widespread use of nitrates. More studies are needed to evaluate the safety and efficacy of these agents in the modern era of guideline-directed use of heart failure therapy.
Keywords: Acute heart failure syndrome, Nitrates, Vasodilator therapy, Morbidity, Mortality
ACEI: Angiotensin Onverting Enzyme Inhibitors; ADHF: Acute Decompensated Heart Failure; AHFS: Acute Heart Failure Syndrome; ARB: Angiotensin Receptor Blockers; BB: Beta Adrenoceptor Antagonists; IHD: Ischaemic Heart Disease;ISDN: Isosorbide Dinitrate; ISMN: Isosorbide Mononitrate; MRA: Mineralocorticoid Receptor Antagonists; N: Nitrates; NYHA: New York Heart Association
Heart failure is a chronic, progressive clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood causing symptoms and signs of pulmonary congestion [1]. Acute heart failure syndrome (AHFS) is defined as the sudden change or the rapid deterioration of symptoms and signs of heart failure, often in response to certain precipitating factors (for example, myocardial ischaemia, cardiac arrhythmia, septicaemia and non-compliance with either drug, or diet therapy, or both), which require urgent medical attention [2]. Over the last 25 years, despite advances in heart failure diagnosis and management, it remains a common yet complex syndrome associated with high rates of morbidity and mortality. Indeed, heart failure continues to represent a major and growing burden on public health worldwide, both in terms of its magnitude and poor prognosis. This is, at least in part, because the contemporary medications that are received by heart failure patients have been proven insufficient to fully prevent hospitalisations [3]. Also, there has been a little research in the management of AHFS, with many treatment strategies based on clinical experience rather than on evidence from high quality studies.
Historical drug treatments for heart failure syndromes included only diuretics and digitalis, mainly for the relief of symptoms of congestion rather than for a mortality benefit [4]. This had prompted further search into evaluating other agents as potential treatments, especially in patients with advanced heart failure. In the early 1970s, initial vasodilator studies in heart failure showed some added haemodynamic benefits with the use of nitrates, mainly by reducing preload [5,6]. Interest in nitrate therapy has increased further as a result of the widespread use of intravenous nitrates in the emergency management of AHFS. Observational studies suggested that the addition of the nitric oxide donor isosorbide dinitrate (ISDN) in acute decompensated heart failure (ADHF) was associated with lower allcause mortality and favourable long-term clinical outcomes, but without reduction in rehospitalisation rate [7,8].
Standard guideline-directed therapy for heart failure has changed dramatically over the last 25 years [9]. The beneficial effects of nitrates may or may not have been masked by newer heart failure treatments. Moreover, it is unclear whether nitrates can significantly improve symptoms of heart failure, although it is widely believed that they do. It is also uncertain whether the effect of these agents confers a different effect on different heart failure phenotypes (for example, heart failure with preserved systolic function, heart failure with reduced systolic function, ischaemic heart disease, valve disease, etc). Previous reviews that studied nitrates in acute heart failure have been small, and included only few studies [10,11]. Perhaps, this is due, in part, to the fact that most prior studies are considered old with inaccurate methods, which might have shaped final results. Recently, a study of home monitoring using a pulmonary artery pressure monitoring device demonstrated a substantial reduction in rehospitalisation rate with similar trends for death in patients with symptomatic heart failure [12]. Apart from diuretics, nitrates were the main agents used to reduce pulmonary pressures, which appeared to be the main mechanism by which the benefit was achieved. We therefore sought to analyse all randomised studies that evaluated the effects of nitrates on clinical outcomes in patients with AHFS.
Many nitrates (e.g. nitroglycerine, isosorbide mononitrate and isosorbide dinitrate) exert their effects in the human body by being converted to nitric oxide (NO). NO is recognized as the most important cellular signalling molecule involved in many physiological and pathological cardiovascular processes [13]. There has been a growing body of evidence to suggest that NO production, as a potent natural vasodilator and a major biological regulator of cardiovascular function, is impaired in patients with heart failure, thus indicating a potential significant beneficial effect of NO enhancing therapy with nitrates [14,15].
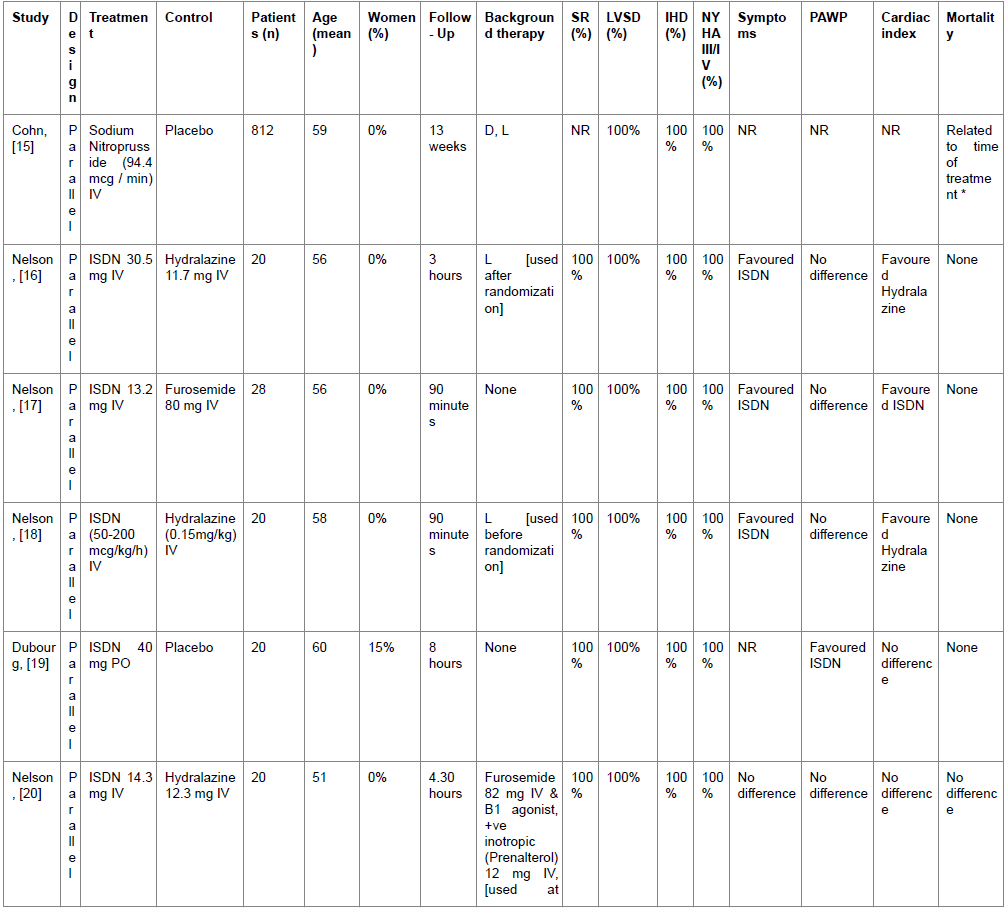
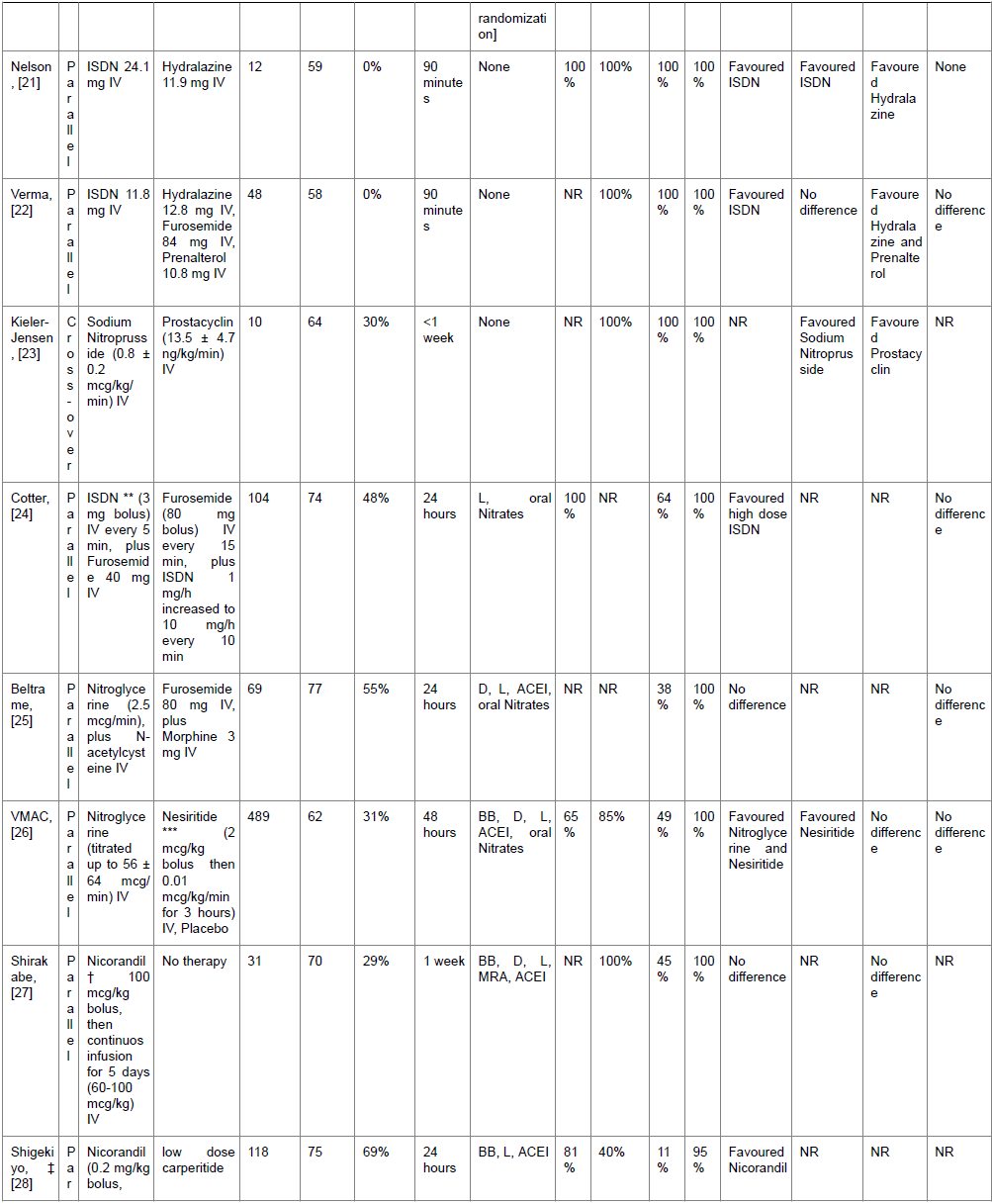
Fifteen randomised studies including 1824 AHFS patients and reporting clinical outcomes were identified. Two small studies including 35 patients with a mean age of 51±8 years studied a combination therapy of nitrates and hydralazine. Of which, one study compared the combination to either drug used alone and the other one compared the combination to captopril and prazosin. For nitrates alone, 14 studies were identified, of which 13 studies included 1714 patients with a mean age of 62 ± 8 years and 17% were women, compared nitrates to alternative interventions, and one study compared a high dose nitrate to a low dose nitrate (Table 1). The majority of studies assessed the effects in men with acute decompensated heart failure (ADHF) due predominantly to left ventricular systolic dysfunction (LVSD). The aetiology of heart failure was ischaemic heart disease (IHD) in about 76% of patients among all studies.
In a study by Nelson et al. [16], when isosorbide dinitrate and hydralazine combination (H-ISDN) was used, by intravenous administration (the average dose of H was 11.6 mg and of ISDN was 13.4 mg over 90 minutes) in 18 men in sinus rhythm with ADHF secondary to IHD, it resulted in a composite haemodynamic profile, which was superior to either drug used alone. There was a significant reduction in left ventricular filling pressures, systolic and diastolic blood pressures and systemic vascular resistance, accompanied by a significant increase in stroke volume, cardiac output and heart rate, compared to either drug used alone. Given that the combination resulted in a powerful preload and afterload reduction, it was concluded that combination therapy may be of greater benefit as long as the fall in mean arterial pressure does not compromise peripheral perfusion, as it appears that the large fall in mean arterial blood pressure was not fully compensated by the reflex increase in heart rate and cardiac output. In another study by Adigun et al. [17], 17 Nigerian patients with hypertensive ADHF (35% were women and all patients were in sinus rhythm) were given H-ISDN combination therapy (intravenous H 30 mg and oral ISDN 30 mg), as compared to captopril 50 mg and prazosin 1 mg given orally in a single-blind parallel group fashion on a background therapy of standard treatments of acute pulmonary oedema including furosemide diuretic. The neurohormonal inhibitors captopril and prazosin exerted the same haemodynamic effects of combination therapy (i.e. reduced left ventricular filling pressures, systolic and diastolic blood pressures and systemic vascular resistance) over 24 hours, yet without causing tachycardia, suggesting that there may be a favourable haemodynamic profile associated with these agents in ADHF.
In comparison with furosemide, ISDN showed no effect on pulmonary artery pressures, suggesting no real major haemodynamic differences between the two agents when given over 90 minutes, mainly in men with ADHF secondary to IHD [18,19]. In a landmark study, Cotter et al. reported that high dose ISDN given as repeated intravenous boluses after low dose intravenous furosemide is beneficial in controlling severe pulmonary oedema in 104 patients with a mean age of 74 ± 9 years (48% were women), compared to low dose ISDN given after high dose intravenous furosemide (20). The high dose ISDN significantly decreased the need for mechanical ventilation and the frequency of myocardial infarction. In that study, all patients were in sinus rhythm and the aetiology of heart failure was IHD in about 64% of patients. The mean dose of ISDN administered during treatment was 11.4 ± 6.8 mg in the high dose group and 1.4 ± 0.6 mg in the low dose group. The mean furosemide doses were 56 ± 28 mg and 200 ± 65 mg, respectively. Although Cotter et al. study has positively influenced clinical practice until date; it is arguable that the results are difficult to interpret because of using a nitrate in both arms of the study [11].
The VMAC study compared nitroglycerine infusion, nesiritide infusion and placebo in 489 patients with ADHF [21]. It was concluded that nitroglycerine and nesiritide significantly reduced symptoms of heart failure, but only nesiritide significantly reduced pulmonary artery pressures compared to placebo. In another study, Cohn et al. reported that short-term (48 hours) sodium nitroprusside infusion may cause a decrease in mortality if only used more than 9 hours after establishment of left ventricular failure following acute myocardial infarction [22]. Interestingly, this study from 1982 is considered the only randomised study to show any reduction in mortality with nitrates use in the setting of heart failure. In comparison with hydralazine, ISDN reduced filling pressures, and improved symptoms of heart failure [16,19,23,24]. However, ISDN was inferior to hydralazine in optimizing cardiac output [16,19,23,24].
Organic nitrates have been commonly prescribed to patients with heart failure mainly for the relief of concomitant angina symptoms, with excellent clinical results. However, their long-term use has been partly limited by tolerance in those patients. For long time, it has been known that the early development of nitrate tolerance with frequent administration of oral preparations or continuous administration of intravenous preparations or long-acting topical preparations, leads to significant attenuation of the drug effects [25]. The mechanisms underlying this phenomenon are still poorly understood. Since the increasing awareness of this problem, extensive research has been conducted to understand the underlying mechanisms in order to prevent nitrate tolerance. Consequently, few approaches have been introduced into clinical practice, including the application of a nitratefree interval or the administration of concomitant drugs that have been suggested to reduce or prevent nitrate tolerance. Only a few randomised studies assessed nitrate tolerance with respect to the haemodynamic and anti-ischaemic effects in heart failure. Some of these studies reported conflicting results. There is some evidence to suggest that long-term oral administration of ISDN and isosorbide mononitrate (ISMN) is associated with sustained haemodynamic effects in patients with chronic congestive heart failure [26,27]. Nacetylcysteine was suggested to be associated with ISDN potentiation of haemodynamic effects in patients with chronic stable heart failure [28]. The concomitant use of oral hydralazine with intravenous nitroglycerine was found to prevent the early development of nitrate tolerance [25]. However, with respect to glyceryltrinitrate therapy [29,30], or sodium nitroprusside [30], no benefit from adding hydralazine was observed. Wada et al. suggested that ACEI or angiotensin receptor blockers (ARB) may prevent the development of nitrate tolerance [31]. Intravenous nicorandil remained haemodynamically effective during the first 24-hour infusion in patients with congestive heart failure [32,33], partly due to its action as a potassium channel opener [32]. This was further suggested to represent a clinical advantage of nicorandil in the short-term treatment of patients with ADHF. However, more studies are needed to support this hypothesis [34].
The review including available randomised studies suggests that there is no clear significant difference in the effect on all-cause mortality between nitrates and alternative interventions in the management of ADHF. Current evidence suggests that nitrates may have some benefit, as an add-on therapy, to relieve symptoms of heart failure in male patients predominantly in sinus rhythm, and having ADHF secondary to IHD (Table 1). This is not surprising given the fact that in a recent UK survey, IHD was responsible for almost 50% of all cases hospitalised with a diagnosis of heart failure [3]. There is insufficient data concerning the use of nitrates in female patients, patients with ADHF who have atrial fibrillation, preserved left ventricular systolic function, or non-ischaemic aetiology of heart failure.
AHFS is a very common presentation to general hospitals, with sizeable human and economic burden. Contemporary medical treatment with angiotensin converting enzyme inhibitors (ACEI), beta adrenoceptor antagonists (BB) and mineralocorticoid receptor antagonists (MRA), now approximately doubles life expectancy of patients with stable heart failure [2]. However, mortality rates remain high, particularly in the first year after a hospitalisation for heart failure [3]. Despite decades of progress, it is estimated that around 800,000 people in the UK currently suffer from heart failure, with this being responsible for about 5% of all emergency hospital admissions [35]. In the United States, there are around 5.1 million people with heart failure, with many people hospitalised ADHF every year [36]. According to the 2012/13 UK National Heart Failure Audit [35], most people admitted to hospital with a diagnosis of acute heart failure are aged over 75 years, with 66% aged between 75 years and 84 years and 30% are over 85 years. Men and women seem to be equally affected, but the majority of patients up to 85 years were men, and for those aged more than 85 years, most were women. Given the advanced age of patients in the recent years, it is possible that heart failure survival rate has improved as a result of more effective healthcare strategies, including the proper management of coronary disease.
Acute heart failure patients are generally classified into two major categories; those who present with heart failure for the first time, and those who have worsening chronic heart failure. In fact, all practicing physicians are familiar with ADHF initial management, which includes oxygen, morphine, diuretics and nitrates, as described by standard textbooks [37]. Current guidelines from the European Society of Cardiology, American College of Cardiology and American Heart Association advocate the additional use of inotropic agents (e.g. dopamine, dobutamine and nor-adrenaline) only if previous treatments provide inadequate improvement. This is mainly due to the long-standing concern that these agents may increase mortality. It is surprising that, to date, there are only a few randomised studies to validate the optimal management of AHFS. Indeed, it may well be that developing AHFS management has been neglected, with no new agents approved for use, for almost a quarter-century.
The haemodynamic hallmark of AHFS includes an elevated left ventricular filling pressure, raised vascular resistance and a normal or diminished cardiac output. The main goal of initial management used to be haemodynamic stabilization and symptom improvement. Contemporary management continues to focus on improving haemodynamics and symptoms by relieving congestion, which may be considered an appropriate strategy to a certain extent [38]. Conventional treatment with acute diuretic therapy (i.e. intravenous furosemide; the most commonly used loop diuretic in clinical practice) may have the disadvantage of causing a large fall in cardiac output leading temporarily to acute pump dysfunction in occasional patients with left ventricular failure [39,40]. This has led to the search for newer agents with effects not only to improve haemodynamics and symptoms, but also to improve clinical outcomes (for example, mortality and hospitalisation). Vasodilator therapy with nitrates, particularly with isosorbide dinitrate, nitroglycerine and nesiritide, has provided some promising results in clinical practice, as suggested by large observational studies [41,42]. However, loop diuretics have remained the mainstay of AHFS management. This is mainly because the decision to use vasodilators is sometimes complex. Vasodilators should probably be avoided in patients presenting with ADHF associated with hypotension or severe mitral or aortic stenosis, for the fear of increased mortality [2].
Available studies are have been limited by the small number of patients and the different dosing regimens and clinical outcomes. None of the included studies have reported medical costs as an outcome measure or made any cost-effectiveness analysis. Further high-quality studies are needed to improve our understanding in the growing acute heart failure patient population.
There is little evidence to support the use of nitrates in AHFS, which is surprising given the widespread use of nitrates. Further large randomised trials are needed to evaluate the safety and efficacy of these agents in the modern era of guideline-directed use of heart failure therapy.