Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2022)Volume 11, Issue 6
Objective: The study assessed magnitude of Nutritional practice and its determinants among pregnant women attending antenatal care unit in Malga District, Southern Ethiopia. Method: A facility based cross-sectional study was conducted from March 1 to April 2, 2020 among 392 pregnant women sampled with systematic sampling technique. Data were collected by trained data collectors using structured interviewed administered questionnaire. A descriptive statistics for different variables was done and summarized as numbers and percentages. Bi-variable and multi variable logistic regressions were performed to identify determinant factors associated with nutritional practice of pregnant women. The strength of statistical association was measured by adjusted odds ratios (AOR) and 95% confidence intervals. Results: Among the interviewed 392 pregnant women only 34.7% (95%CI: 30.1%, 39.3%) of them have good practice on maternal nutrition during their pregnancy. women’s educational status (AOR= 3.43, 95%CI: 1.173,10.027), family size (AOR= 0.116, 95%CI: 0.037,0.36), house hold monthly income (AOR= 2.875, 95%CI: 1.077,7.676), husband’s educational status (AOR= 5.97, 95%CI:1.551,23.033) and having nutrition information (AOR= 3.096, 95%CI: 1.213,7.902) were determinants significantly associated with nutritional practice of pregnant women. Conclusion: Nutritional practices of pregnant women’s were relatively low in this study. Women’s educational status, household monthly income, family size, husband’s educational status and having nutrition information were significant determinants of maternal nutritional practice. The concerned bodies should strengthen nutrition education on importance of maternal nutrition and sustain household income through providing income generation activities.
Nutritional practice, Pregnant women, Antenatal care, Malga District, Southern Ethiopia
Nutrition plays a major role in maternal and child health and it is widely recognized that optimum nutrition in early life is the foundation for long term health. Pregnancy represents a unique time in life with considerable potential to influence not only maternal health but also the health of the next generation [1].
Extra needs for energy, macronutrients and micronutrients are required throughout the pregnancy period to provide the needed nutrients to the growing fetus and to ensure health and wellbeing of the mother. During pregnancy, Women in developing countries face a higher risk of malnutrition and nutritional deficits resulting in negative pregnancy outcomes such as delay in fetal growth and development, pre-term delivery, low birth weight and maternal anemia [2].
In Ethiopia Malnutrition is among the most serious health problem affecting mothers and their children. Undernourished mothers face high risks during pregnancy and childbirth, and their children go through a risky developmental path, both physically and mentally [3].
As a result of dietary habits and patterns in pregnancy, dietary inadequacies are higher during pregnancy than at any other stage of the life cycle [4]. Restriction of food intake and inappropriate nutritional practices in combination with environmental and socioeconomic factor is common causes of maternal mortality, low birth weight, and intergrowth retardation [5]. In developing countries poor nutritional status in pregnancy accounts for 14% of fetuses with intra uterine growth restriction (IUGR) [6]. It has been estimated that 41.8% of pregnant women worldwide are anemic & 57.1% of pregnant in Africa were anemic where as in Ethiopia 62.7% of pregnant women were suffering from anemia, and it is a severe public health problem [7].
According to Ethiopian Demographic and Health Survey (EDHS) 2016 report rural areas have a higher percentage of thin women (25%) than urban areas (15% and also women living in rural areas are more likely to be anemic (25%) than those living in urban areas (17%) [8]. Maternal malnutrition contributes to low birth weight and as a result low birth weight contributes to neonatal mortality. According to United Nations International Children’s Emergency Fund (UNICEF) nearly 4 million newborns die within 28 days of birth. Intervening on maternal nutrition particularly on pregnant mothers can play great role in reducing both maternal and neonatal mortality [9,10].
The low status of women, poor maternal nutrition, inadequate prenatal care and the disproportionate burden of physical labor borne by mothers are some of the greatest impediments to improving nutritional practice as well as nutritional status [11].
The government of Ethiopia has prioritized strengthening interventions to reduce malnutrition among the most vulnerable group; infants, under five children and pregnant and lactating women [12]. Among the five strategic objectives sated and envisioned at the end of 2020 by Ethiopian national nutrition program was improving the nutritional status of women (15-49 years) and adolescent girls (10-19 years) [13]. Pregnant mother’s nutritional status at the time of conception is a key factor for development and fetal growth, so a healthy, balanced diet is essential both before and during pregnancy. During pregnancy, the mother’s diet provides energy and nutrients to both herself and the fetus growth and for future lactation [14].
Adequate knowledge regarding various aspects of feeding practices during pregnancy is very essential [15]. Appropriate nutritional practice during pregnancy is crucial in reducing maternal and infant mortality as well as under nutrition. Any nutritional education and/or intervention policy that aims to improve women’s habits during the pregnancy period requires knowledge of the habitual nutritional patterns in this stage of life but most studies focus on nutritional status of pregnant women’s. Even though few studies are carried out on nutritional practice of pregnant mothers, they are concerned primarily on urban areas. In our country researches focused on nutritional practice of pregnant mothers particularly in rural setups are rare and there is no study conducted regarding the problem in the study area. Therefore; this study was aimed to assess Nutritional practice and its determinants among pregnant mothers attending antenatal care unit in Malga District, Southern Ethiopia.
Study design, period and setting
A facility-based cross-sectional study was conducted from March 1 to April 2/2020 in Malga District, Southern Ethiopia. Malga District is one of the 23 districts in Sidama zone, South Nations Nationalities and Peoples region (SNNPR). The District is located 301 kilometers from Addis Ababa (capital city of Ethiopia) and 26 kilometers from Hawassa (capital city of SNNPR) [16].
Population
All pregnant women who attended ANC in Malga District health facilities were the source population whereas all randomly selected pregnant women who attended ANC in randomly selected health facilities during the study period were the study population for the study.
Sample size determination
The sample size was calculated using single population proportion formula (n= (Z α ⁄2) 2 p (1-p)/d2) by considering the following assumption: 95% level of confidence= 1.96, proportion (p) of 39.3% good nutritional practice among pregnant women’s in North West Ethiopia [17], margin of error (5%) and nonrespondent rate of 10%. Accordingly, the estimated final sample size for this study was 402.
Sampling procedure
In Malga District there are 26 health posts, 4 health centers and 1 primary hospital. The calculated sample size was proportionally allocated to the randomly selected health posts, health centers and primary hospital based on the number of clients attending antenatal care (ANC) in the previous one month before the study period. To select study subjects from each antenatal care unit systematic sampling technique was applied by using client’s registration order to get ANC care during the data collection period. Then every 2 women, as they registered, were included in the study at each antenatal care unit until the desired sample size was attained
Data Collection Procedures
A structured interviewer administered questionnaire was used to gather important information from each study respondent. The questionnaire was developed by reviewing different related literatures with modification according to the objective of this specific study. The tool was prepared in English and then translated to Amharic and local language (Sidaamu Afoo) [18-22]. The questionnaire included Socio demographic and economic factors, maternal obstetric factors, maternal health service related factors and access to nutrition information.
The structured questionnaire was pretested on 5% of the total sample size in nearby health center (Haro Health Center). Data collectors and principal investigator was participated during the pretest. Then the questionnaire was assessed for its clarity, logical flow, length and completeness and the necessary correction was made before the actual data collection. We used six diploma holder health professionals for conducting the interview and one degree holder nurse for supervising the data collection process after giving two days training regarding the objective of the study, relevance of the study, informed consent and techniques of interview. Data were collected using face to face exit interviews during government working hours.
Nutritional practice of pregnant women: To determine nutritional practice level of the respondents, using the structured interviewer administered questionnaire scores were computed for the 7 nutritional practice questions (Table 3). One point was allocated to a correct response which is favorable for optimal maternal nutrition & 0 for incorrect response. For each question of nutritional practice the correct answers were summed together (the sum of the total scores for nutrition practices were varied from (0 up to points of 7 maximum score) and the mean score was computed for the total respondents response. Those who were scored above (>) the mean score were considered as having good nutritional practice where as those who were scored below (<) the mean score were considered as having poor nutritional practice [18].
Data management and analysis
The data were checked, cleaned and entered using Epi-info version 7 and exported to stastical package for social sciences (SPSS) version 23 for analysis. The descriptive analysis such as frequency distribution, percentages, mean and standard deviation (SD) were used.
Both bi variable and multi variable logistic regression models were fitted to identify determinant factors associated with nutritional practice of pregnant mothers. To identify determinant factors associated with the outcome variable, a bi- variable logistic regression analysis was performed for each independent variable and crude odds ratio (COR) with 95% confidence intervals was obtained. Those variables that have p-value less than 0.2 on bivariable analysis were considered for multi-variable analysis. The presence and strength of statistical association was measured by adjusted odds ratios (AOR) and 95% confidence intervals. In all cases P-value, less than 0.05 was considered as statistically significant. The multivariable model was tested for goodness of fit with the Hosmer Lemeshow test and it is non-significant. Finally the results were presented using tables, graphs and charts [17,22].
Socio-Demographic Characteristics of Respondents
A total of 392 (97.5%) pregnant women’s were included in the study. The mean age (+/-standard deviation) of the respondents was 26.8 years (+/-3.86 years), while the age range was 18-36.About ten in seven 277(70.7%) of the respondents were found in the age group 25 to 34 years. Majority of the respondents 345(88%) were Sidama by ethnicity and 332(84.7%) of them were Protestant by religion. All of the study participants (100%) were married with average (+SD) family size of 4.43(+1.799) and nine in ten 354 (90.3%) reside in rural areas.
As far as educational status and occupational status of study population is concerned, more than half 215 (54.8%) of the study participants did not receive any formal education and nearly seven in ten 276(70.4%) were house wife’s. One hundred eighteen eight (48%) respondent husbands did not receive any formal education and about 261(66.6%) were farmers in their occupation. Regarding household monthly income greater than half 247(63.0%) of the study participants have estimated monthly income of less than 1000 ETH birr (1$=36 Ethiopian birr). (Table 1)
| Variables | Frequency | Percent |
|---|---|---|
| Age in years(n=392) | ||
| 15-24 | 101 | 25.8 |
| 25-34 | 277 | 70.7 |
| >35 | 14 | 3.6 |
| Residence(n=392) | ||
| Rural | 354 | 90.3 |
| Urban | 38 | 9.7 |
| Ethnicity(n=392) | ||
| Sidama | 345 | 88 |
| Oromo | 32 | 8.2 |
| Amhara | 15 | 3.8 |
| Religion(n=392) | ||
| Protestant | 332 | 84.7 |
| Muslim | 36 | 9.2 |
| Orthodox | 15 | 3.8 |
| Catholic | 9 | 2.3 |
| Educational status(n=392) | ||
| No formal education | 215 | 54.8 |
| Primary(1-8) | 115 | 29.3 |
| Secondary and above | 62 | 15.8 |
| Occupational status(n=392) | ||
| House wife | 276 | 70.4 |
| Employed | 41 | 10.5 |
| Daily labourer | 38 | 9.7 |
| Merchant | 37 | 9.4 |
| Respondents husband educational status(n=392) | ||
| No formal education | 188 | 48 |
| Primary(1-8) | 127 | 32.4 |
| Secondary and above | 77 | 19.6 |
| Respondents husband occupational status(n=392) | ||
| Farmer | 261 | 66.6 |
| Employed | 49 | 12.5 |
| Daily labourer | 31 | 7.9 |
| Merchant | 51 | 13 |
| Estimated household monthly income in ETH birr (n=392) | ||
| <999 | 247 | 63 |
| 1000-1999 | 81 | 20.7 |
| >2000 | 64 | 16.3 |
| House hold family size (n=392) | ||
| 1-4 | 174 | 44.4 |
| 5-7 | 167 | 42.6 |
| >7 | 51 | 13 |
1$=36 Ethiopian birr
Table 1: Socio demographic characteristics of study participants, malga district, 2020.
Maternal Obstetric and Health Service Related Characteristics of Respondents
Out of the total study subjects 221(56.4 %) were in third trimester of pregnancy. Two hundred fifty two (64.3%) of the study participants were multi gravida. Among multi gravidas and grand multi gravidas 226(68.3 %) had attended ANC for their previous pregnancy. Facility types used for previous ANC were health center, health post and hospital constituting 125(55.3 %), 68 (30.1 %) and 33 (14.6 %) respectively. Ante natal care attendant for current pregnancy was 110(28.1%) for first ANC visit and 44 (11.2%) for fourth ANC visit. Concerning the gap between the previous and current pregnancy, around 182 (55%) of the participants currently become pregnant between 1- 2 years of the previous pregnancy while 149(45%) of them become pregnant after staying for greater than 2 years from the previous pregnancy. Regarding access to nutrition information more than half 230(58.7%) of the pregnant mothers had no nutrition information. (Table 2)
| Variables | Frequency | Percent |
|---|---|---|
| Gestational age for current pregnancy (n=392) | ||
| First trimester | 19 | 4.8 |
| Second trimester | 152 | 38.8 |
| Third trimester | 221 | 56.4 |
| Gravidity(n=392) | ||
| Primi gravida | 61 | 15.6 |
| Multi gravida | 252 | 64.3 |
| Grandmulti gravida | 79 | 20.2 |
| ANC for previous pregnancy(n=331) | ||
| Yes | 226 | 68.3 |
| No | 105 | 31.7 |
| Facility used for previous ANC (n=226) | ||
| health centre | 125 | 55.3 |
| health post | 68 | 30.1 |
| Hospital | 33 | 14.6 |
| ANC visit for current pregnancy(n=392) | ||
| 1st | 110 | 28.1 |
| 2nd | 142 | 36.2 |
| 3rd | 96 | 24.5 |
| 4th | 44 | 11.2 |
| Gap between current and previous pregnancy(n=331) | ||
| 2-Jan | 182 | 55 |
| >2 | 149 | 45 |
| Nutrition information (n=392) | ||
| Yes | 162 | 41.3 |
| No | 230 | 58.7 |
Table 2: Maternal obstetric and health service related characteristics of the respondents, Malga District, public health facilities, 2020.
Nutritional Practice of Pregnant Women’s
From the total majority of the study participants 262(66.8 %) consumed a meal three and less times a day before the interview. More than half 219( 55.9%) of the respondents eaten any special food that is different from their routine feeding during their pregnancy because they consider it as important for their pregnancy and 170(43.4 %) were taken any additional meal during pregnancy in addition to meals in their non-pregnancy state.
Regarding eating snack between meals only 169(43.1%) of the study subjects ate snack between meals. Among the interviewed pregnant women’s around 133(33.9 %) increased their food intake frequency at least four times and more per day during their pregnancy. from the total respondents without change in their frequency of meal intake (less than 4 times per day) during their pregnancy; 214(82.6%) of them take 3 times and 45(17.4%) of them take only 2 times. (Figure 1)
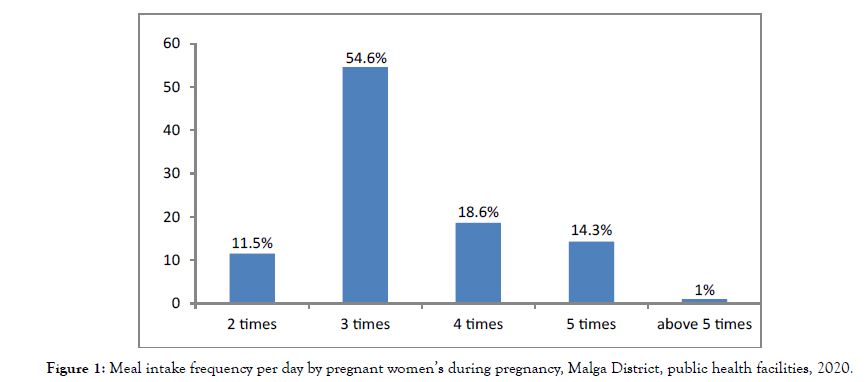
Figure 1:Meal intake frequency per day by pregnant women’s during pregnancy, Malga District, public health facilities, 2020.
On the other hand about 215(54.8%) of the participants avoid certain food items during their pregnancy. from the major food items avoided by the respondents during pregnancy state; milk and milk products and egg and meat accounts for 78(36.3%) and 105(48.8%) respectively. The major reasons behind avoidance of some of the food stuffs by the pregnant mothers was their belief on tradition/culture 171(79.5%) and religion 12(5.6%). Seventy two (33.5%) and twenty two (10.3%) of the respondents mentioned the fear that the fetus grows bigger; eventually causes difficulty in labor and harm to the fetus as a consequence if the avoidable food items are consumed. On the other way out of the total study participants only 129(32.9%) of them can decide by themselves what to eat during pregnancy. (Table 3)
| Variables | Frequency | Percent |
|---|---|---|
| Yesterday day and night food intake frequency (n=392) | ||
| 1-3 times per day | 262 | 66.8 |
| 4 and above times per day | 130 | 33.2 |
| Eat any special food during pregnancy (n=392) | ||
| Yes | 219 | 55.9 |
| No | 173 | 44.1 |
| Increase meal frequency during pregnancy than usual (n=392) | ||
| Yes | 170 | 43.4 |
| No | 222 | 56.6 |
| Eat snacks between meals during pregnancy (n=392) | ||
| Yes | 169 | 43.1 |
| No | 223 | 56.9 |
| Food intake frequency during pregnancy (n=392) | ||
| 1-3 times per day | 259 | 66.1 |
| 4 and above times per day | 133 | 33.9 |
| Avoids any food item during pregnancy (n=392) | ||
| Yes | 215 | 54.8 |
| No | 177 | 45.2 |
| Food items avoided by pregnant women during pregnancy(n=215) | ||
| Milk and milk products | 78 | 36.3 |
| Egg and meat | 105 | 48.8 |
| Butter and oil | 30 | 14 |
| Fruits (avocado, mango, papaya) | 16 | 7.4 |
| Cereals (barley, wheat, maize, sorghum, teff) | 5 | 2.3 |
| Reasons mentioned for avoidance of certain food items during pregnancy (n=215) | ||
| Cultural(traditional) belief and customary rumours | 171 | 79.5 |
| Religious belief | 12 | 5.6 |
| Others* | 32 | 14.9 |
| Consequences mentioned if these avoidable food items are consumed(n=215) | ||
| Fetus grows bigger and can result in difficult labor | 72 | 33.5 |
| These foods may plaster on fetus | 64 | 29.7 |
| These foods may harm the fetus | 22 | 10.3 |
| Can cause abortion and still birth | 8 | 3.7 |
| Not necessary for pregnant | 9 | 4.2 |
| Others** | 40 | 18.6 |
| Decide what to eat during pregnancy(n=392) | ||
| Yes | 129 | 32.9 |
| No | 263 | 67.1 |
*=dislike, less appetite, fear of illness and unable to afford, **= gastric upset & discomfort and sin
Table 3: Nutritional practices of pregnant women, Malga District public health facilities, 2020.
Generally based on the nutritional practice assessing questions the result in this study revealed that only 136(34.7%) (95%CI: 30.1%, 39.3%) of the respondents had good nutritional practice by correctly scoring above the mean score. (Figure 2)
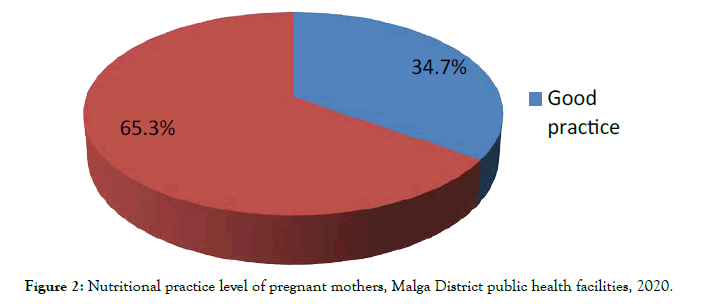
Figure 2:Nutritional practice level of pregnant mothers, Malga District public health facilities, 2020.
Determinants of Nutritional Practice of Pregnant Women’s
In bi variable analysis, variables with p- value less than 0.2 were considered as a candidate variable for multi variable analysis. Age, educational status, occupational status, respondents husband educational status, respondents husband occupational status, estimated household monthly income, family size, gravidity, ANC for previous pregnancy, type of facility used for previous ANC, ANC visit for current pregnancy and having nutrition information were identified as a candidate variable for multi variable analysis by yielding P value <0.2. After multi variable analysis was preformed five variables (respondents educational status, having nutrition information, respondents husband educational status, household monthly income and family size) showed significance association with nutritional practice with a p value of <0.05.
Educational status has a significant association with nutritional practice of pregnant mothers. Women’s with primary education had 3.4 times more odds of good nutritional practice as compared to women’s with no formal education (AOR= 3.4,95% CI:1.17,10.03). The odds of good nutritional practice was about 3 times higher for those mothers who had information about nutrition during pregnancy than those mothers who had no information about nutrition during pregnancy (AOR= 3,95% CI:1.21,7.9).
The odds of good nutritional practice among study subjects whose husbands education status of secondary and above were 6 times higher than that of study subjects whose husbands with no formal education (AOR= 6, 95% CI:1.55,23.03). Similarly, pregnant mothers with an estimated monthly house hold income of 1000- 1999 ET birr (1$=36 Ethiopian birr) had 2.875 times more odds of good nutritional practice as compared with those having <1000 ET birr (AOR= 2.875, 95% CI: 1.08, 7.68)
Relative to pregnant mothers with family size of 1-4, mothers with family size of > 7 had 88.4% less likely of nutrition practices during pregnancy (AOR = 0.116, 95%CI: 0.04, 0.36). (Table 4)
| Variables | Nutritional Practice | 95% CI | ||
|---|---|---|---|---|
| Good | Poor | COR(95% CI) | AOR(95% CI) | |
| Educational status | ||||
| No formal education | 29(21.3) | 186(72.7) | 1 | 1 |
| Primary(1-8) | 53(39.0) | 62(24.2) | 5.483(3.207-9.373)*** | 3.43(1.173-10.027)* |
| Secondary and above | 54(39.7) | 8(3.1) | 43.293(18.703-100.213)*** | 5.14(1.172-22.54)* |
| Husband educational status | ||||
| No formal education | 16(11.8) | 172(67.2) | 1 | 1 |
| Primary(1-8) | 66(48.5) | 61(23.8) | 11.631(6.261-21.608)*** | 3.065(1.097-8.563)* |
| Secondary and above | 54(39.7) | 23(9.0) | 25.239(12.439-51.209)*** | 5.97(1.551-23.033)** |
| House hold monthly income in ET birr | ||||
| <999 | 46(33.8) | 201(78.5) | 1 | 1 |
| 1000-1999 | 44(32.4) | 37(14.5) | 5.196(3.022-8.935)*** | 2.875(1.077-7.676)* |
| >2000 | 46(33.8) | 18(7.0) | 11.167(5.935-21.011)*** | 6.954(1.610-30.04)** |
| Family size | ||||
| 1-4 | 74(54.4) | 100(39.1) | 1 | 1 |
| 5-7 | 49(36.0) | 118(46.1) | 0.561(0.358-0.879)* | 0.116(0.037-0.36)*** |
| >7 | 13(9.6) | 38(14.8) | 0.462(0.230-0.929)* | 0.186(0.036-0.972)* |
| Ever had nutrition information | ||||
| Yes | 100(73.5) | 62(24.2) | 8.692(5.398-13.995)*** | 3.096(1.213-7.902)* |
| No | 36(26.5) | 194(75.8) | 1 | 1 |
*=p<0.05, **=p<0.01 ***=p<0.001; COR=Crude odds ratio, AOR=Adjusted odds ratio, CI=Confidence interval, ET birr=Ethiopian birr (1$=36 Ethiopian birr), 1=Reference category.
Table 4: Determinants of nutritional practice of pregnant mothers in Malga District, Southern Ethiopia, 2020.
It is known that improving maternal nutrition practices during pregnancy is essential to save lives and improve health outcomes for both mothers and babies. In our study; only 34.7% ( 95%CI: 30.1%, 39.3%) of pregnant women are found to have good nutritional practice during their pregnancy which is consistent with research findings from East Wollega (33.9%), Addis Ababa (34.5%) and in line with that of Gondar (40.1%) [18,19,22].
The result of the present study also showed lower nutritional practice of pregnant mothers compared to studies conducted in Malaysia and Pakistan in that the score for good nutritional practice were 65.5% and 74% respectively [23,24]. The low nutritional practice in the current study may emanate from relatively high family size, low monthly income, low educational status and lack of nutrition information as compared to the previous studies [25].
Even though it is recommended for a pregnant woman to take 4 and above meals per day during pregnancy in order to support the ongoing demand of her developing fetus, only 33.9% of study participants had meal frequency of 4 times and above during their pregnancy which is in agreement with a study from Ghana (37.7%) and it is also comparable with a report from Odeda, Nigeria (28%) [26,27].
Finding from this study revealed that around 43.1% of the respondents practiced the habit of eating snacks between meals during their pregnancy which is consistent with a study conducted in east wollega and in contrast with a study result from Bahirdar town,Gondar town,Accra and rural Pakistan in which in this studies higher proportion of respondents shows increment of frequency of snack consumption during pregnancy [28].
Concerning food aversion during pregnancy 54.8% of study participants reported that they avoid certain food items during pregnancy which is consistent with study findings from Shashemene district (49.8%), Saudi Arabia (47.4%) and comparable with report from Borno state, Nigeria (61.22%) [29,30]. On the other way it is higher than from that of East Wollega (35.8%), Bahirdar (33%), Gondar (39.9), Wondo genet (20.9%) and lower than from results in semi urban Ogun state, Nigeria (82.2%) [17,18,22,31]. These variations may be attributed to differences in sample size, geographical location, socio economic and socio-cultural differences.
The finding of our study identified that respondent’s educational status have positive significant association with nutritional practice of pregnant mothers during pregnancy in which women’s with primary education & higher education (secondary and above) are more likely to practice good nutritional practice than mothers with no formal education. Similar finding was observed in a study done in Gondar town and Brazil [32-34]. However studies from Pakistan and East wollega contradicts with this finding indicating that literacy level had no significance influence on nutritional practice of pregnant mothers [18,24].
Similarly this study demonstrated that information about nutrition during pregnancy has statistically significance association with nutritional practice of pregnant mothers. Relative to mothers who had no information about maternal nutrition during pregnancy mothers who had information were 3 times more likely to practice good nutrition during pregnancy. This finding is supported by the study conducted in Guita Guida district and Gondar town [18,22]. This is expressed by the fact that women’s who have information on maternal nutrition during pregnancy can acquire knowledge and can be motivated on good nutritional practice.
Study participants whose husband education status of primary and secondary & above had higher chance of good nutritional practice than that of mothers whose husbands with no formal education which is in agreement with a study from Addis Ababa [19].
Our study also identified that house hold monthly income had positive statistical association with mother’s nutritional practice. Pregnant mothers with an estimated monthly house hold income of 1000-1999 and >2000 ET birr were more likely to have good nutritional practice compared with mothers having <1000 ET birr. Similar findings had been reported from a study in Brazil and Swaziland. This might be due to the fact that income can influence availability of resources which in turn improve access to a diversified diet and thus improve nutrition practice.
Moreover family size showed significance association with nutritional practice of pregnant women’s. Comparing women with family size of 5-7 &>7 to that of women with 1-4 family size, women with higher family size (5-7 &>7) were less likely to practice good maternal nutrition. This finding is similar with results from East wollega and Ghana [18,26]. This result can be explained by the fact that higher family size can lead to insecure distribution of food within the house hold and put uneven share for the mother; in turn which may lead to sub optimal nutritional practice. In contrary to the present study, report from a study in Gondar town implied that family size had no influence on nutritional practice of pregnant mothers [22]. This variation may arise from difference in sample size and study setting since the present study conducted in rural setting. Since this study did not explore qualitative aspects further researches on this study area should incorporate mixed designs.
Limitation of the study
The study was not complemented with a qualitative aspect to investigate in depth information.
This study may prone to recall bias because of the reason that the respondents may not correctly remember all previous moments.
Depending up on the finding of this study we can conclude that majority of pregnant women’s had a poor nutritional practice; only 34.7% of the respondents were found to have good nutritional practice during their pregnancy. The present study also showed that educational status of respondents, household monthly income, family size, respondent’s husband educational status and having nutrition information were significant determinants of nutritional practice of pregnant mothers.
In order to overcome the problems there should be strengthen over all education with focus on girl’s involvement. Increasing household income through providing income generation activities on behalf of the government should be created. Health care providers should provide nutrition information (education) on importance of maternal nutrition to all women of reproductive age starting from preconception through pregnancy and postpartum.
Ethical Consideration
Ethical clearance was obtained from Hawassa University College of medicine and health science Institutional Review Board (Ref. no: IRB 036/11). Permission letter from the health facilities were obtained to undertake the study. Informed verbal consent was taken from each study participant before interview administration. Honesty and confidentiality were maintained with the right not to participate in the study.
Availability of data and materials
Data is not available for online access, however, readers who wish to gain access to the data can write to the corresponding author Habtamu Eskendir at habtisheske@gmail.com
Competing interests
The authors declare that they have no competing interests
Funding
The authors received no specific funding for this study.
Acknowledgments
We would like to thank Hawassa University College of medicine and health science for allowing the conduct of this study. We would like to express our heartfelt thanks to Malga District Health Office for their kind support and collaboration. Our deepest gratitude also extends to study participants, data collectors and supervisor for their willingness and great contribution.
List of Abbreviations
ANC: Antenatal Care, AOR: Adjusted Odds Ratio, CI: Confidence Interval, EDHS: Ethiopian Demographic and Health survey, IFA: Iron and Folic Acid, IUGR: Intra Uterine Growth Restriction, OR: Odds Ratio, SNNPR: South Nation Nationalities People Region, SPSS: Stastical Package for Social Sciences, UNICEF: United Nations International Children’s Emergency Fund, WHO: World Health Organization
Consent to Publish
Not applicable
Authors’ contributions
HEZ, BMH and DTH participated in planning the study, writing proposal, monitoring data collection process and analyzing the data, writing the result and the manuscript. All authors agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Zewdie HE (2022) Nutritional Practice and its Determinant's among Pregnant Women in Public Health Facilities of Malga District, Southern Ethiopia. J Women's Health Care 11(6):586
Received: 06-Apr-2022, Manuscript No. JWH-22-16604; Editor assigned: 08-Apr-2022, Pre QC No. JWH-22-16604(PQ); Reviewed: 22-Apr-2022, QC No. JWH-22-16604; Revised: 24-May-2022, Manuscript No. JWH-22-16604(R); Published: 09-Jun-2022 , DOI: 10.35248/2167-0420.22.11.586
Copyright: © 2022 Zewdie HE, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.