Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2024)Volume 12, Issue 7
The article's topic is devoted to the surgical treatment of aneurysms of the infrarenal aorta, the achievements we have achieved in the perioperative period, and the prevention of possible complications that may arise in the postoperative period. For this purpose, clinical materials from 125 patients were analysed. The average diameter of the abdominal aorta was 6.3 cm. Indications for OSR were an aneurysm neck <4 mm (23.8%), unilateral iliac artery aneurysms (11.5%), bilateral iliac artery aneurysms (9.3%), iliac artery tortuosity >40° of angulation (13.1%), extensive aortic thrombus (16.4%), and aortic neck angulation >45° (13.7%), patient preference (12.2%). Surgery “Repair of the aneurysm using a tube graft” in 34 patients; “Aorto-biilac graft” in 50 patients, "Aortobifemoral bypass” was performed on 41 patients. In patients, the surgery was performed using general anesthesia combined with epidural anesthesia. The duration of the operation was 293.0 ± 11.87 minutes. The Cell Saver apparatus was used for autotransfusion. The average volume of blood loss was 3252.5 ± 219.12 ml. Mortality in the postoperative period occurred in 3.2% of patients. Causes of death; major bleeding in 1 patient; 1 patient had intestinal obstruction and 2 patients had acute myocardial infarction.
Aortic aneurysm; Myocardial infarction; Aneurysm prosthesis; Vascular synthetic prostheses; Autotransfusion
Aortic aneurysms are the 13th leading cause of death in the United States of America. Although aneurysms can occur along the entire length of the aorta, the infrarenal location is considered one of the most common and dangerous vascular diseases [1]. In 80%, the aneurysm is usually located infrarenal [2]. The main difference is that it is more common in men. The most dangerous condition of Abdominal Aortic Aneurysms (AAA) is its rupture. The prevalence of pathology has increased significantly with age, bad habits, and as a complication of heart disease. The frequency of AAA for men younger than 50 years old is 6%, for 60 years and above 18%, for 70 years 12% [3].
The purpose of the study is to develop measures for the surgical treatment of aneurysms of the infrarenal abdominal aorta, our achievements in the perioperative period, and the prevention of possible complications that may arise in the postoperative period. Co-authors were permitted by the Ethics Committee to write articles based on patient histories and laboratory test statistics while maintaining patient anonymity. We are aware of decision No. 137 dated December 29, 2011, of the Ministry of Health of the Republic of Azerbaijan on the rules of ethical behavior of doctors.
In 2020-2024, we analyzed the clinical materials of 125 patients who applied to the Department of Vascular Surgery of Academician M. Topchubashov Medical Center with a diagnosis of "Infrarenal Aneurysm of the Abdominal Aorta" (IAAA). 123 (98.4%) of the patients were men, 2 (1.6%) were women. In history, all male patients smoked 30-50 cigarettes per day for many years. The age of the patients was 59.1 ± 2.05, height 166.9 ± 5.01 cm, and weight 70.51 ± 1.81 kg. The patients complained of abdominal pain, lower limb pain, constipation, urinary retention, and hypertension, and it is shown in Figure 1. 11 (8.8%) patients did not have any complaints, and by chance, the presence of an aneurysm in the infrarenal abdominal aorta was discovered during USM of the abdominal cavity.
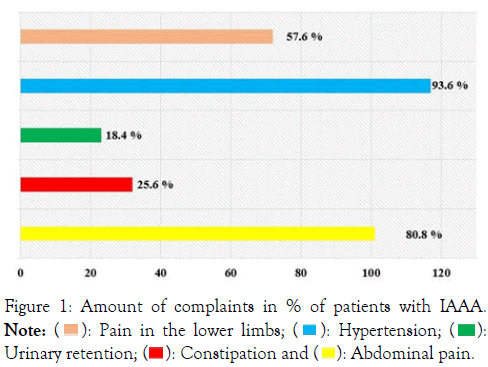
Figure 1:Figure 1: Amount of complaints in % of patients with IAAA.
Note: ( ): Pain in the lower limbs; (
): Pain in the lower limbs; ( ): Hypertension; (
): Hypertension; ( ): Urinary retention; (
): Urinary retention; ( ): Constipation and (
): Constipation and ( ): Abdominal pain.
): Abdominal pain.
All patients underwent appropriate examinations in the preoperative period: Chest X-ray, Doppler ultrasound, computed tomography, ECG, and echocardiography. The Ejection Fraction (EF) was 44.45 ± 2.06%. In 23 (18.4%) of the patients who underwent echocardiography, the presence of areas of hypokinesia on the back wall of the myocardium was found. 96 of the patients had antiaggregant and anticoagulant (dabigatran, THROMBASS, ASPIRIN CARDIO, clopidogrel), 117 hypotensive (onsart, triplixan, noliprel), 11 antiarrhythmic (concor, cardarone), 33 hypolipidemic (rosvax) drugs in their history received per Operating system (Figure 2).
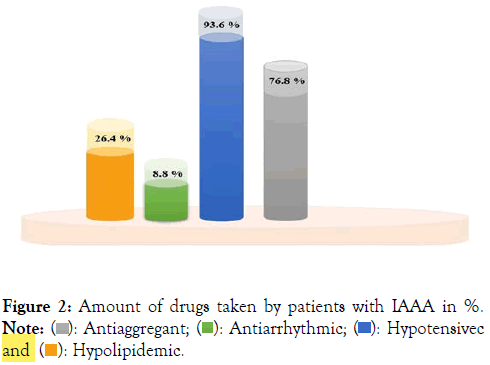
Figure 2: Amount of drugs taken by patients with IAAA in %.
Note: ( ): Antiaggregant; (
): Antiaggregant; ( ): Antiarrhythmic; (
): Antiarrhythmic; ( ): Hypotensivec and (
): Hypotensivec and ( ): Hypolipidemic.
): Hypolipidemic.
All patients were found to have 2 or more comorbidities. In addition, 32 patients were not dependent on insulin; 28 patients with insulin-dependent diabetes; hypertension in 117 patients; chronic ischemic heart disease, post-infarction cardiosclerosis, and heart failure in 47 patients (PCI in 13); Condition after CABG in 18 patients; Chronic obstructive pulmonary disease in 81 patients; BPH in 11 patients; atrial fibrillation in 31 patients; syphilis in 2 patients; hepatitis C in 8 patients; 71 patients had superficial erosions and ulcers of the stomach and duodenum and are shown in Table 1. In the preoperative period, all patients underwent a planned upper GI endoscopy examination, 23 (18.4%) patients had duodenal ulcers and 48 (38.4%) patients had gastritis, which is shown in Table 1.
| Associated diseases | % | |
|---|---|---|
| Diabetes | non-insulin-dependent | 25.6 |
| insulin-dependent | 22.4 | |
| Hypertension disease | 93.6 | |
| CHD, Postinfarction cardiosclerosis, heart failure | 37.6 | |
| Status post CABG | 14.4 | |
| Chronic obstructive pulmonary disease | 64.8 | |
| BPH | 8.8 | |
| Syphilis | 1.6 | |
| Atrial fibrillation | 24.8 | |
| Duodenal ulcer | 18.4 | |
| Gastritis | 38.4 | |
| Hepatitis C | 6.4 | |
Table 1: Percentage of comorbidities in patients with IAAA.
Patients were divided into 3 groups. Group I “Repair of the aneurysm using a tube graft” in 34 patients, group 2 “Aortobiilac graft” in 50 patients, group 3 “Aortobifemoral bypass” was performed on 41 patients (Figure 3).
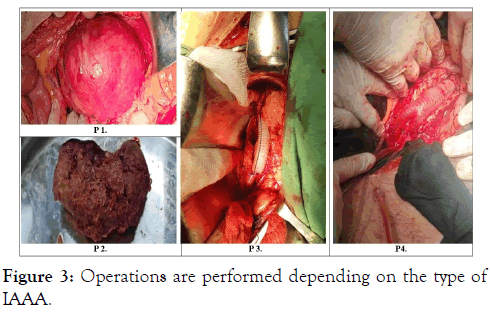
Figure 3: Operations are performed depending on the type of IAAA.
The duration of the operation was 293.0 ± 11.87 minutes. A Cell-Saver device was used to reinfuse blood collected from the surgical wound (Figure 4). The average volume of blood loss was 3252.5 ± 219.12 ml. After the operation, the condition of the vascular anastomoses was monitored by Doppler ultrasound, and there were no complications related to the prosthesis.
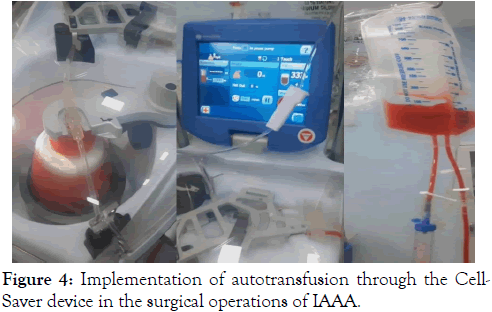
Figure 4: Implementation of autotransfusion through the Cell- Saver device in the surgical operations of IAAA.
The results of treatment in patients were studied in the early postoperative periods. In the early postoperative periods, the evaluation criteria included the restoration of blood flow in the lower limbs, the adequacy of blood circulation in the damaged areas, the function of vital organs during the operation, the results of blood and urine tests, the restoration of intestinal motility, and recovery. In patients, the operation was performed with the application of combined epidural intubation anesthesia. In the preoperative period, the central veins were catheterized in all patients, a catheter was inserted 3-5 cm from the epidural space at LII-LIII level and 0.75% ropivicaine solution was used. At the same time, in the preoperative period, general and biochemical analyses of blood, and coagulogram indicators were determined, and the concentration of troponins, gas content of blood, and acid-alkaline balance were also studied. Patients with high concentrations of troponins were transferred to the intensive care ward in the pre-operative phase and were under the supervision of a cardiologist. Intravenous nitroglycerin 10 mg infusion, detoxification therapy was performed, and cardioprotectors and drugs that improve rheology and antioxidants were administered. Patients with no positive dynamics were examined by coronary angiography. 15 of the patients underwent stenting of the coronary arteries of the myocardium, and synthetic prosthesis surgery was performed on the patients in later periods. Before applying a clamp to the aorta, anesthesia was deepened, nitroglycerin 0.2-0.4 mcg/kg min was infused if necessary, and heparin 5000 IU was injected. When hypotension develops, norepinephrine 0.1-0.3; dopamine was infused at 3-5 μg/kg min. During infusion therapy, Ringer, HES, aprotinin 50,000 units, erythrocyte mass, and fresh frozen plasma were transferred; blood acid-alkaline balance was determined, and 4% sodium bicarbonate solution was used to compensate for metabolic acidosis. Mortality was noted in 4 patients (3.2%) in the postoperative period. The cause of death was "Thrombohemorrhagic syndrome, polyorqan failure" developed as a result of internal bleeding in 1 patient; In 1 patient, there was "impassability developed as a result of acute ischemia of the left half of the large intestine and deep homeostasis disorders developed against this background, polyorqan failure", and in 2 patients, polyorqan failure developed as a result of acute myocardial infarction and reperfusion syndrome: Lung-heart-kidney failure. 1 patient (0.8%) developed acute renal failure in the postoperative period, so the patient received 3 sessions of temporary hemodialysis, and improvement in his condition was noted. The patients' inhospital bed days were 5-8 days. On the 4th -5th day of the operation, the patients were activated and fed.
Studies conducted by several scientists show that the development of various complications affects the results of surgical treatment of AAIA. Thus, complications such as kidney failure, myocardial infarction, and branch thrombosis in the early postoperative period in patients who were taken to the emergency operating table in hemorrhagic shock as a result of ruptured aneurysms delay recovery and lead to the development of lethality [1]. Linda and co-authors, note in their study that ischemia of the left half of the colon was found in 2 patients. As a result, this situation was aggravated by gangrene and peritonitis and caused death [3]. To prevent ischemic complications of the colon after reconstructive surgery, the authors developed a method of preventing the blood circulation of the colon in the basin of the inferior mesenteric artery. The method was based on intraoperative measurement of retrograde pressure in the inferior mesenteric artery before and after compression of the internal iliac arteries. Since the scientists determined the participation of the iliac arteries in the collateral blood supply of the left half of the colon, they reimplanted the mesenteric arteries to the branches of the aortofemoral prosthesis to prevent intestinal ischemia. We researchers also agree and support the opinion of these scientists. Among the complications after AAA resection, cerebrovascular complications are 0.5-1.0%, and lethality is 30-40% [4]. According to Kuivaniemi et al. [2], the most common complication after surgical intervention of the abdominal aorta and its branches is intestinal ischemia. The frequency of this complication is 15%. Thus, they claim that ischemic colitis is detected in 4.5-8.9% of cases after planned operations and in 15-60% of cases after interventions during abdominal aortic aneurysm rupture [2]. Thus, according to our results, to prevent reperfusion syndrome and kidney failure in the early postoperative period, special attention should be paid to the restoration of macro and microcirculation, and acid-alkaline balance should be corrected in time and correctly [5]. To prevent cardiac complications in the postoperative period, we consider it appropriate to detect patients with abdominal aortic aneurysms early before the main stage of the operation, to perform angiography of the coronary vessels of the heart in time, and if necessary, to perform stenting. At the same time, continuous infusion of nitroglycerin and the use of anticoagulants are advisable in the early stages of the operation. To prevent the development of ischemic processes in the large intestine, it is important to control the pressure in these vessels during surgery, as the internal iliac arteries participate in the collateral blood supply of the left half of the large intestine [6]. To correct possible disorders in the blood coagulation system during the postoperative period, we consider it necessary to transfer aprotinin and fresh frozen plasma at the end of the operation.
The main cause of death in the early postoperative period: "Thrombohemorrhagic syndrome" developed as a result of internal bleeding in 1 patient; 1 patient had intestinal obstruction, polyorqan failure, and 2 patients had an acute myocardial infarction. To prevent cardiac complications in the postoperative period, early detection of patients with abdominal aortic aneurysms before the main stage of the operation and timely coronary angiography and stenting of patients with high concentrations of troponins in the preoperative period are considered appropriate. In the postoperative period, to correct the disorders that may occur in the blood coagulation system, we consider it necessary to transfer aprotinin and fresh frozen plasma at the end of the operation.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ilgar N, Kamala N, Fuad H, Nizami M, Rasim G, Azer A, et al. (2024). Open Surgical Treatment of Aneurysm of the Infrarenal Abdominal Aorta: Still Valuable in an Endovascular Era. Angiol Open Access. 12:476.
Received: 10-Jul-2024, Manuscript No. AOA-24-32845; Editor assigned: 12-Jul-2024, Pre QC No. AOA-24-32845 (PQ); Reviewed: 26-Jul-2024, QC No. AOA-24-32845; Revised: 02-Aug-2024, Manuscript No. AOA-24-32845 (R); Published: 09-Aug-2024 , DOI: 10.35841/2329-9495.24.12.476
Copyright: © 2024 Ilgar N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.