
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2023)Volume 14, Issue 6
Introduction: Measurement of ONSD by ultrasonography is a surrogate measure of ICP in laparoscopic surgeries. This study aimed to evaluate the change in ONSD with changes in IAP and EtCO2 in patients undergoing laparoscopic cholecystectomy.
Methods: After approval from IEC and BOS, 60 adult patients undergoing elective surgery were selected for the study. Optic nerve aligned directly opposite the 6 MHz-13 MHz linear probe of USG machine of Hitachi Aloka F31 and ONSD measured 3 mm behind the globe perpendicular to axis of the scanning plane at T0, T1, T2, T3 i.e. after intubation, at IAP of 10 mm Hg, 15 mm Hg and after desufflation. Further, the changes in ONSD corresponding to changes in IAP were measured after standardizing EtCO2 to normal level (35 mm Hg-40 mm Hg).
Result: There was significant variation in ONSD (p<0.001) with reference to IAP. EtCO2 went beyond 40 mm Hg in 30% of cases and the increase in ONSD was significantly more (p<0.001) as compared to the patients in whom EtCO2 was within the normal range.
Conclusion: ONSD is a non-invasive, easily performed approach and varies significantly with IAP. Therefore we can imply that increase in IAP can indirectly lead to increase in ICP in clinical scenarios of acute elevations of IAP. A rise in EtCO2>40 mm Hg can also be used as an individual evidence of a rise in ICP in cases where ONSD cannot be measured.
Intraabdominal pressure; Optic nerve sheath diameter; Intra cranial pressure; End-tidal CO2; Ultrasonography
Studies have proved that acute elevation of Intra-Abdominal Pressure (IAP) increases Intra Cranial Pressure (ICP) [1,2]. Invasive method such as ventriculostomy proves to be the most accurate at measuring ICP but may not be ideal in many resource limiting settings and is prone to various complications. In recent years, non-invasive techniques such as measurement of Optic Nerve Sheath Diameter (ONSD) by Ultrasonography (USG) have been developed and suggested as a possible indicator of intracranial hypertension [3].
The optic nerve sheath is contiguous with the dura mater, and its contents are contiguous with the subarachnoid space. The intra-orbital part of the sheath, and particularly its retro-bulbar segment, can distend when ICP is elevated. Thus, raised ICP leads to an increase in the ONSD [4].
Dip F, et al., observed that the acute elevation in IAP during laparoscopy significantly increased the ICP. The changes in the ONSD reflected a temporary and reversible increase in the ICP due to the acute elevation of IAP. Dinsmore M, et al., in their study demonstrated that the ONSD changes rapidly with increase in EtCO2 i.e. hypercapnia (>5.3 kPa) and returns to baseline when normocapnia is restored [5,6].
Based on the previous studies we know that increase in IAP leads to an increase in ONSD and changes in EtCO2 also bring about a change in ONSD [4,5]. ONSD acts as a surrogate marker to predict raised ICP, the cut-off value being a matter of discussion over the last decade. Therefore, we conducted a study with a primary aim to quantitatively evaluate the exact change in ONSD caused by changes in IAP and EtCO2, in patients undergoing laparoscopic surgery. The secondary aim of our study was to evaluate an optimal cut-off value for ONSD with change in IAP, which can predict raised ICP and also to identify which is a more sensitive parameter between EtCO2 and ONSD, to reflect changes in IAP.
After obtaining approval from institutional ethical clearance committee, board of studies and clinical trials registry India (CTRI/2021/02/031333), sixty adult patients (aged 18 years-60 years) belonging to ASA physical status I and II, undergoing laparoscopic cholecystectomy under general anaesthesia with endotracheal intubation were enrolled after written, informed consent. Patients having features of increased ICP due to any cause (tumor, malignancy, injury, or surgery), known cases of hyperthyroidism, and pregnant/lactating females were not included in the study. A standard anaesthesia technique for premedication, induction, and relaxation were used with a uniform monitor for intraoperative monitoring in all the patients.
Bedside USG was done by an experienced anesthesiologist trained in sonography techniques. One eye was scanned through closed eyelids in the supine position in a transverse plane using a high-resolution 6 MHz-13 MHz linear array transducer with USG machine of Hitachi Aloka (F31) after applying tegaderm. An ample amount of USG gel was used to prevent direct physical contact of the transducer with the eyelid. Optic nerve was aligned directly opposite the probe and ONSD measured 3 mm behind the globe perpendicular to axis of the scanning plane (Figure 1). Average of 3 readings from one eye was taken. The changes in ONSD were measured with the corresponding changes in IAP and EtCO2 at:
T0: Just after tracheal intubation.
T1: 5 mins after stabilisation of IAP of 10 mm of Hg.
T2: 5 mins after stabilisation of IAP of 15 mm of Hg.
T3: 10 mins after desufflation of gas.
Further, the changes in ONSD corresponding to changes in IAP were measured after standardizing EtCO2 to normal level (35 mm Hg-40 mm Hg).
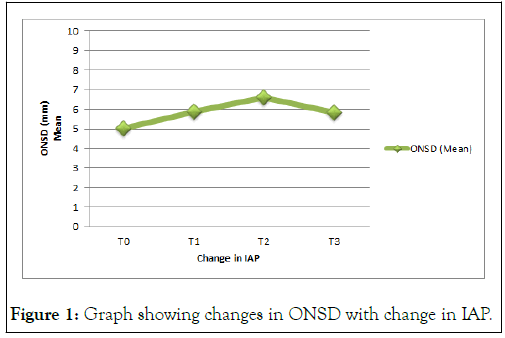
Figure 1: Graph showing changes in ONSD with change in IAP.
Statistical analysis
Direct comparisons of ICP with ONSD have been studied before. We confronted an approach where each patient was considered his/her own control. Data were analyzed using Microsoft Excel Statistical Package for Social Sciences (SPSS) software version 23.0. A power analysis suggested that a minimum sample size of 60 patients would be required to detect a mean 0.5 mm difference (SD: 0.58 mm) in the ONSD between T0 and T2 with a power of 90% at a significance of P<0.05. The results were presented in number, percentage, mean and standard deviation as appropriate. Time changing quantitative parameters like EtCO2 and ONSD were analysed with change in IAP using one way ANOVA test. Data for ONSD were compared between the two groups having EtCO2>40 mm Hg and EtCO2 within normal range using student’s t-test. The cut-off value, sensitivity, specificity, and accuracy for ONSD and EtCO2 with change in IAP were evaluated using Receiver Operating Characteristic (ROC) Curve. A P-value less than 0.05 were considered statistically significant.
The demographic and surgical profile of the patients in the study, including age, gender, weight distribution, type of surgery, and duration of surgery are depicted in Table 1.
| Mean age | 42.8 years ± 9.12 years | |
| Sex ratio | Male | 24 (40%) |
| Female | 36 (60%) | |
| Mean weight | 62.2 kgs ± 8.04 kgs | |
| Mean duration of surgery | 54.50 mins ± 17.68 mins | |
| Type of surgery | Laparoscopic cholecystectomy | |
Table 1: Demographic and surgical profile of the studied patients.
In our study ONSD above 6.55 mm was used as a cut-off value after applying the ROC curve. There could be a simultaneous rise in ICP with the increase in ONSD above 6.55 mm since it acts as a surrogate marker of ICP. However, we did not co-relate this finding by measuring ICP with the invasive method since it was not within the purview of our study design. Our finding was in accordance with the previous studies conducted by del Saz-Saucedo P, et al.; Kishk NA, et al. Steinborn M, et al., and Padayachy LC, et al. [7-10].
The change in ONSD with reference to changes in IAP was statistically significant (p<0.001) as depicted in Figure 2.
Figure 2: Graph showing changes in ONSD with change in EtCO2 at IAP of 15 mm Hg.
Increase in EtCO2 lead to increase in ONSD. There was a significant (p<0.001) increase in ONSD in 30% (18/60) of the patients where EtCO2 went beyond 40 mm Hg as compared to those where it was within normal limits i.e. <40 mm Hg when IAP was stabilized to 15 mm Hg. In this subset (30%) of patients, after hyperventilation when the EtCO2 was normalized between 35 mm Hg-40 mm Hg there was a simultaneous decrease in ONSD to 6.51 mm ± 0.29 mm. This decrease in ONSD was statistically significant (p<0.001) (Figure 3).
Figure 3: Graphical representation of changes in EtCO2 and ONSD with change in IAP from 10 mm Hg to 15 mm Hg.
The changes in EtCO2 and ONSD with reference to IAP change from 10 mm Hg to 15 mm Hg were statistically significant (p<0.001) (Figure 4). ROC curve was plotted which depicted that EtCO2 concentration more than 42.6 mm Hg can be used as cut off value with area under the curve 0.732 with sensitivity 80.0%, specificity 46.7% and accuracy 73.2% with increase in IAP. While ONSD more than 6.55 mm can be used as cut off value with area under the curve 0.815 with sensitivity 71.7%, specificity 90.0% and accuracy 81.5% with increase in IAP.
Figure 4: ROC curve showing sensitivity, specificity and accuracy of EtCO2 and ONSD with increase in IAP.
McNemar’s Chi-squared statistic test was applied which showed that the difference between sensitivity and specificity of EtCO2 and ONSD with change in IAP were statistically significant (p<0.001).
Out of a total of 60 patients in our study, 60% were female which was in accordance with the study conducted by Kara D, et al., and Shah SB, et al. This could be probably because our study was based on laparoscopic cholecystectomy which is predominantly in female patients. On the contrary, the male population was predominant in the study conducted by Whiteley JR, et al., and Kapoor I, et al. because they selected patients undergoing radical prostatectomy and brachial plexus injury which were predominantly in males [11-15].
The ONSD increased significantly (p<0.001) with an increase in IAP and returned close to baseline after deflation of pneumoperitoneum in all patients in our study.
Our findings were similar to the study conducted by Dip F, et al., who observed changes in ONSD with gradual creation of pneumoperitoneum at 14 mm Hg. However, they measured ONSD at different intervals, 15 mins and 30 mins where it increased significantly and finally returned close to baseline after deflation of pneumoperitoneum. Also, Kara D, et al. In their study observed significant (p<0.001) change in the ONSD from baseline, in the group where IAP was 15 mm Hg as compared to IAP of 10 mm Hg. This increase in ONSD in response to pneumoperitoneum can be attributed to increased pressure in the parenchymal, vascular, osseous, and CSF compartment of the brain which further leads to distension of dura mater and increase in diameter of ONSD.
It was observed that at IAP of 15 mm Hg, the rise in EtCO2 was beyond 40 mm Hg in 30% of cases. In this subset of patients the increase in ONSD was significantly more (p<0.001) as compared to the patients in whom EtCO2 was within the normal range. This indicates that with the increase in EtCO2 above 40 mm Hg the ONSD also increased. This finding in the small (30%) group of patients can be attributed to the late physiological effects of pneumoperitoneum leading to an increase in PaCO2, which further increases ONSD [16].
Cullen LK, et al., were of the opinion that a minimum of 10 min-15 min is required for PaCO2 elevation after pneumoperitoneum in laparoscopic procedures [17]. In the late stage of pneumoperitoneum, the diffusion of CO2 from the peritoneum results in reflex arterial vasodilation in the CNS, thus further increasing ICP. Compression of the lower lobes of the lungs creates a ventilation/perfusion mismatch, further increasing PaCO2. However, our finding was not in accordance with the study conducted by Park CG, et al., where no significant difference was observed in the ONSD between the hypercapnia and normocapnia groups. This result may be associated with the propofol based TIVA used for general anaesthesia in their study as propofol can attenuate the effect of hypercapnia on cerebral autoregulation compared to inhalational agents [18,19].
In our study, we also observed the effect of hyperventilation on ONSD. There was a significant (p<0.001) decrease in ONSD when EtCO2 was normalized to <40 mm Hg, in patients where it went beyond 40 mm Hg. This finding further strengthened the parallel relation established between EtCO2 and ONSD and it was similar to studies conducted by Kim JY, et al; Dinsmore M, et al.; Bala R, et al. [20,21].
Based on the findings of ROC curve, EtCO2 was more sensitive and ONSD was more specific to reflect the change in IAP, while the accuracy of both the parameters was nearly comparable. This difference was statistically significant (p value<0.001) on applying McNemar’s Chi-squared statistic test. This could probably be due to the lower cut-off value for EtCO2 and higher cut-off value for ONSD as lower cut-off value results in increased sensitivity and decreased specificity and vice versa.
Every study has some element of bias and hence, we tried to eliminate as much as possible from our study by taking certain aspects into consideration. The ONSD was measured by an experienced anesthesiologist who was unaware of the IAP and EtCO2 at different time intervals when measurements were taken, thus eliminating the observer bias. All the measurements of ONSD were done in the supine position to avoid the additional effect of the position of the patient on ONSD.
This study had some limitations as well. It was limited to only a particular type of surgery and small sample size. The measurement of ONSD was done only during supine position as per the study design. However, as per the reported literature, ONSD is affected in trendelenburg and reverse trendelenburg positions also [22-24].
Therefore, we conclude that the use of bedside ocular USG in measuring ONSD has the advantage of being a non-invasive, portable, and easily performed method for ICP evaluation in clinical scenarios of increased IAP. A rise in EtCO2>40 mm Hg may act as an individual evidence of a rise in ICP in cases where ONSD cannot be measured. The patients in our study did not experience any symptoms, detrimental effects, or signs of increased ICP after their surgeries probably because of the shorter duration of surgery. However, a further study may be conducted with a larger sample size to rule out the limitations.
This study was approved by the institutional research ethics committee Jawaharlal Nehru medical college and hospital, faculty of medicine, Aligarh Muslim university, Aligarh in a meeting held on October 23, 2010, as recorded in act number 61/FM/IEC.
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the code of ethics of the world medical association (declaration of helsinki).
The authors declare that they have followed the protocols of their work centre on the publication of patient data.
The authors declare that no patient data appear in this article. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Anjali Kumari: Study planning, data collection, interpretation of results, and initial writing of the manuscript.
Syed Moeid Ahmed: Conception of the original project, study planning, interpretation of results, final writing and approval of the manuscript.
None.
None.
None.
ISACON 2021.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kumari A, Ahmed SM (2023) Optic Nerve Sheath Diameter Changes with Changing Intra-abdominal Pressure and End-Tidal CO2 in Laparoscopic Surgery: A Prospective, Observational Study. J Anesth Clin Res.14:1121.
Received: 21-May-2023, Manuscript No. JACR-23-24311; Editor assigned: 23-May-2023, Pre QC No. JACR-23-24311 (PQ); Reviewed: 06-Jun-2023, QC No. JACR-23-24311; Revised: 26-Jul-2023, Manuscript No. JACR-23-24311 (R); Published: 28-Dec-2023 , DOI: 10.35248/2155-6148.23.14.1121
Copyright: © 2023 Kumari A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.