Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 1
In this series of cases it can be shown that the age group with the greatest number of complications was those from 1 month to 24 months. Impetiginization was the most frequent type of complication, oxacillin was the most used antibiotic and systemic corticoid was indicated in 30% of the cases.
Oral ivermectin, the only drug for systemic use, was indicated alone or in combination in 73% of the cases. From these cases, 57% were between 1 to 12 months old, without evidence of side effects. It could be considered as a first line treatment for impetiginized scabies in this group age
Scabies; Pediatric; Ivermectin
The scabies is found worldwide and affects an estimated of 100 to 300 million people each year [1]. In 2013, it was the fifteenth cause of outpatient consultation. In 2017 it became the second cause in the outpatient Dermatology offices at INSN [2]. The prevalence is high in regions of the Pacific and Latin America, it is more frequent in children than in adolescents and adults [3]. It is a parasitic disease caused by the mite Sarcoptes scabiei Variety hominis and is exclusively human. It is transmitted by person-to-person contact and requires only twenty minutes of an upcoming contact for a successful transmission [3]. The clinical presentation differs especially in children under the age of 2, with pruritic lesions that involve palms, soles, face and scalp [4].
According to substantial epidemiological evidence, in tropical regions, scabies can be complicated with pyodermitis, renal and cardiovascular diseases. Due to the invasion of bacteria such as Staphyphylococcus aureus and Streptococcus pyogenes of Group A [5]. The diagnosis is difficult because the symptoms and signs may resemble other skin disease, up to today there is no molecular or blood test to corroborate the clinical diagnosis [5]. There is no international consensus regarding treatment schemes, especially for the pediatric population. Up to day the permethrin is considered a safe medication for children over two months, but there is much controversy in the use of oral ivermectin in children under the age of 5, and 15 kilograms. There is no medication until now that in addition to its scabicide effect, it can prevent relapse, inflammatory reactions and associated skin infections [6]. Therefore, we consider that the report of the experience of management of this disease, in particular of complicated cases, may be of interest and would contribute to the development of a treatment scheme for this population.
Thirty cases of complicated scabies were hospitalized in the Dermatology department (Table 1). 26 corresponded to impetiginized scabies (Figure 1), which represents 86.7%. The distribution by sex was equal: 15 patients for each group. The average age was 23.5 months, 1 month was the minimum age and 12 years 9 months, the maximum. 24 (80%) patients were under 1 year old and of these, 16 (53%) from 1 to 3 months (Figure 2). According to the treatment (Figure 3), 12 received Ivermectin, 8 received Permethrin, and 9 received combined treatment with Ivermectin plus permethrin. This means that 22 (73%) received Ivermectin, and of these 17 (57%) were younger than 12 months. No side effects were reported during the treatment received. The parenteral antibiotic most used was oxacillin 22 (73%), which was rotated orally to Cephalexin 22 (73%) of the cases. 5 patients (17%) received topical corticoid and 10 (33%). systemic treatment.
| AGE CHART | |||||||
| 1-3 months | 4-12 months | >12 months | |||||
| n | % | n | % | n | % | ||
| Admission diagnosis | Impetiginized scabies | 14 | 46.70% | 7 | 23.30% | 5 | 16.70% |
| Eczematized scabies | 1 | 3.30% | 0 | 0.00% | 0 | 0.00% | |
| Norway Scabiosis | 0 | 0.00% | 1 | 3.30% | 0 | 0.00% | |
| Scabies+Cellulitis | 1 | 3.30% | 0 | 0.00% | 1 | 3.30% | |
| Etiological treatment | Permethrin | 4 | 13.30% | 3 | 10.00% | 1 | 3.30% |
| Ivermectin | 7 | 23.30% | 3 | 10.00% | 2 | 6.70% | |
| Permethrin+Ivermectin | 4 | 13.30% | 2 | 6.70% | 3 | 10.00% | |
| Ivermectin+Lindano 1%+Triancinolone | 1 | 3.30% | 0 | 0.00% | 0 | 0.00% | |
| Side effect | None | 16 | 53.30% | 8 | 26.70% | 6 | 20.00% |
| Tx Antibiotic EV | Oxacillin | 10 | 33.30% | 6 | 20.00% | 6 | 20.00% |
| Clindamycin | 3 | 10.00% | 1 | 3.30% | 0 | 0.00% | |
| Oxacillin+Clindamycin | 1 | 3.30% | 0 | 0.00% | 0 | 0.00% | |
| Not indicated | 2 | 6.70% | 1 | 3.30% | 0 | 0.00% | |
| Tx Antibiotic Oral | Cephalexin | 10 | 33.30% | 7 | 23.30% | 5 | 16.70% |
| Amoxicillin Ac. Clavulanic | 3 | 10.00% | 0 | 0.00% | 0 | 0.00% | |
| Not indicated | 3 | 10.00% | 1 | 3.30% | 1 | 3.30% | |
| Tx topical corticosteroid | Hydrocortisone | 2 | 6.70% | 0 | 0.00% | 0 | 0.00% |
| Mometasona | 0 | 0.00% | 0 | 0.00% | 1 | 3.30% | |
| Fluticasona | 1 | 3.30% | 0 | 0.00% | 0 | 0.00% | |
| Desonide+Prednisone | 1 | 3.30% | 0 | 0.00% | 0 | 0.00% | |
| Tx Systemic Corticoid | Prednisone or Prednisolone | 5 | 16.70% | 4 | 13.30% | 0 | 0.00% |
| Not indicated | 7 | 23.30% | 4 | 13.30% | 5 | 16.70% | |
| Tx: Treatment; EV: Intravenous | |||||||
Table 1: Distribution by age and characteristics of the patients.

Figure 1: Impetiginized Scabies.
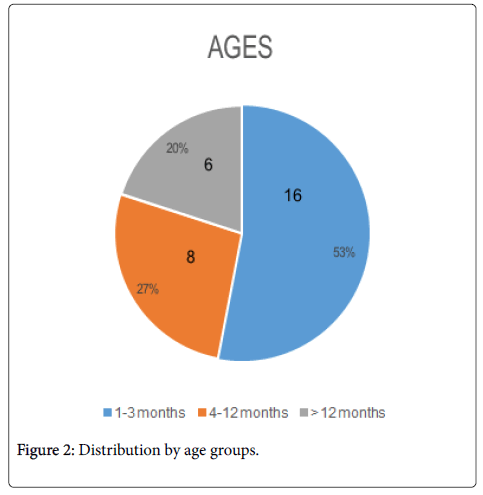
Figure 2: Distribution by age groups.
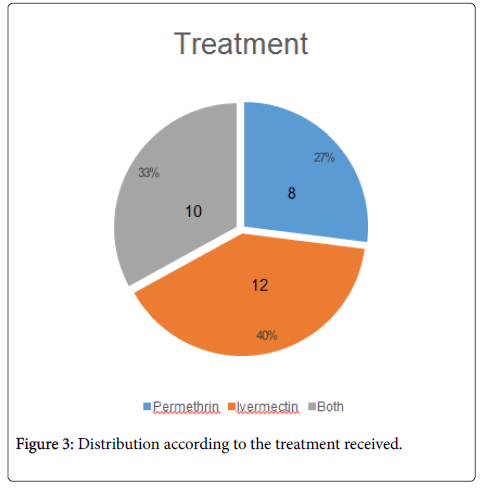
Figure 3: Distribution according to the treatment received.
The management of patients who suffer from complicated scabies’ is difficult; this complication develops on the skin as scorched, pustular and exudative lesions. However, the topical use of sulfur, benzyl benzoate and permethrin can be an alternative treatment for children under two years. Nonetheless, some of them are cosmetically unacceptable because they could increase the inflammatory process causing more damage to the skin. This complication is also treated with antibiotics until it improves and continues with the subsequent topical treatment. The disadvantage is that the risk of contagion is maintained in family members and health personnel.
Furthermore, some studies indicate that both Sarcoptes scabiei and Streptococcus pyogenes produce multiple complement inhibitors in order to overcome the host's innate defense mechanisms. Therefore, the treatment of both pathogens, at the same time, could be the most recommended in order to avoid major complications such as sepsis due to Streptococcus pyogenes. Even though the recommendation for the use of ivermectin oral is only for children over the age two, others believe this treatment should be administered for children over five, whose weight is 15 kilograms. Moreover, 15 years ago doctors recommended its use if the patient was one year old or weighed 10 kilograms [7,8]. In this series of cases, ivermectin was administered in 73% of patients, and 57% of them were between one to twelve months old.
The adverse events of the central nervous system have only been reported in some people with high blood counts of Loa Loa microfilaria, shortly after receiving treatment with ivermectin [9]. Other effects are related to the agent that is treated as pruritus, rash, urticaria, vomiting when it has been used for filariasis and strongyloidiasis. The major risks would be related to the simultaneous use of drugs that affect or are affected by the transport of P. glycoprotein such as: cotrimazole, phenothiazine, rifampicin or inhibitors such as clarithromycin, erythromycin and itraconazole. The use of drugs with GABA potential activity like barbiturates, benzodiacipins and valproic acid are also related to risks. In addition, the patients reported did not have these risk factors; this could explain the absence of side effects. However, it is advisable to be alert to neurological manifestations that could be unseen in this group of patients [10].
Oral ivermectin could be considered as a first-line treatment for cases of impetiginized scabies in patients older than 1 month and younger than 12 months. The application of scabicide creams on these patients could increase the inflammatory process. For that reason, these data has to be contrasted with randomized trials that can evaluate the treatment of oral ivermectin of patients over one-month old, and younger than 12 years old.
JPMF carried out the conception, design of the article and data collection. CGS made the drafting, review and approval of the final version.
Citation:
Flores JPM and Saravia CG (2019) Oral Ivermectin in Complicated Scabies on Hospitalized Patients at the National Institute of ChildHealth. J Clin Exp Dermatol Res 10: 482. doi: 10.4172/2155-9554.10.482
Received: 28-Nov-2018 Accepted: 10-Jan-2019 Published: 17-Jan-2019
Copyright:
© 2019 Flores JPM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original author and source are credited.