
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Research Article - (2023)Volume 13, Issue 5
Introduction: Due to the abundance of drugs and chemicals, poisoning has become a common medical emergency that affects people worldwide. Even though it has been identified that this issue is a serious community health concern in Ethiopia, the exact extent of this problem has not yet been correctly surveyed.
Objective: This study aimed to analyze the factors that influence the outcome of adult patients with poisoning at a tertiary care center.
Materials and methods: A 5-year institution-based cross-sectional study was done. Data were gathered by retrospective chart review using structured questionnaires. The data were entered into version 26 of the SPSS software program after coding and cleaning for further analysis. Descriptive statistics, multivariate analysis, and bivariate analysis were performed to evaluate the effects of various factors on the outcome of the study. The odd ratio was used to estimate the relative risk of poisoning. P values below 0.05 were considered significant.
Results: The study revealed that the death and discharge rates were 13.7% and 86.3%, respectively. Among the various factors that were analyzed, being from an urban area was associated with the likelihood of being discharged (p=0.024). Intubated patients were also less likely to be discharged, which means the need for intubation was a strong predictor of death (p=0.033).
Conclusion: This study revealed that the death rate in our study was very extreme when brought into comparison with the results of previous studies. Urban origin and the need for intubation were independent determinants of the outcome.
Poisoning; Determinants; Outcome; Triage; Intubation; Rural; Urban
The majority of pharmaceuticals and synthetic essences are now widely available in society as a result of scientific and societal advancements. Due to their negative effects, these synthetic entities constitute a real threat [1]. The term "poisoning" refers to the potential of a chemical having a harmful effect on the body. A substance is considered poisonous if it has the potential to cause harm or bodily malfunction when it is ingested, inhaled, absorbed, or injected. The exposure's evolving characteristics could be local or generalized, more topical or systemic [1,2]. Poisoning is a real emergency, and it is a common reason for emergency room visits and medical care. Its associated mortality and morbidity are major community health problems in many nations [3].
The most frequent causes of the incidence are pesticides and drugs. In developing nations, agrochemical pesticides pose a serious public health problem. The most commonly used medications for self-harm in cities in the developing world are those that act on the central nervous system. Barbiturates were a very common cause of self-poisoning during the 1970s, and considerable series exist from this time. Nevertheless, there are few case series of antiepileptic, benzodiazepine, or antidepressant drugs [4,5]. Some Asian and African communities have serious issues with household items such as kerosene used for illumination, cleaning agents such as bleach, and powerful acids used for drain cleaning [6]. In most incidents of self-poisoning, organophosphate insecticides were responsible for the majority of deaths, specifically in patients from rural districts [7].
More than 1 million illnesses are thought to occur annually throughout the world as a direct or indirect result of specific poisons. The precise number of incidences, however, could be substantially higher [8]. According to the World Health Organization’s (WHO) estimation, there are between 2 and 3 million accidental poisonings worldwide each year, of which 1 million result in severe poisonings, while the estimated number of intentional poisonings each year is around 2 million, which kills 200,000 people [9,10]. Numerous studies also revealed that severe poisoning has been noted as a significant contributor to mortality and morbidity in underdeveloped nations. Poisoning is the fourth-most common cause of mortality in India, with a death rate ranging from 15 to 30% [11]. Acute poisoning is one of the top ten causes of hospital deaths in Sri Lanka, where the reported fatality rate is 10% [12]. Acute poisoning accounts for 7% of morbidity in Botswana and is the third most common injury that necessitates hospitalization [3,13].
Studies on the prevalence of acute poisonings in Ethiopia are scarce. The few institution-based studies that have been conducted to date have shown that the death rate ranges from 1.5% to 8.6%. The lack of poison control centers and toxicological experts among health professionals may enhance the likelihood of adverse health effects from acute poisoning for the general population, despite the chemical compound's rapidly rising prevalence in the nation [14-16]. This study attempted to identify gaps and potential intervention areas in terms of management practice, outcome, and other acute poisoning characteristics. This study would serve as a baseline for upcoming multicenter investigations.
Participants, setting, and study design
This institutional-based cross-sectional study was conducted from 2016 to 2021 at Tikur Anbessa Specialized Hospital, the biggest tertiary care facility in the country. The hospital has many clinical departments, including emergency and critical care medicine, internal medicine, pediatrics, gynecology and obstetrics, general surgery, family medicine, psychiatry, ophthalmology, ENT (Ear, Nose, and Throat), dentistry, neurology, and other specialty and subspecialty departments. The Department of Emergency (ED) was established as a separate department in 2008, and at the moment it contains five distinct operating areas. Red (where critical patients are stabilized and monitored), orange, yellow, and green (where stabilized patients from the red area and stable patients from triage are kept, managed, and observed), and the triage area (where patients are classified based on their clinical condition and given a triage card). Sixty-five residents, 60 nurses, and 14 consultants are currently employed in the ED [17]. All adult cases (age 13 or older) with a diagnosis of poisoning during the study period were contained. Over the designated study period, 183 patients’ charts had complete data and were included in this study.
Study variables
By using a pretested data collection format, trained data collectors gathered information on age category, sex, place of residence, referral source, triage classification, name of toxic agents involved, the situation of poisoning, predisposing factors, way of exposure, the average period from exposure to hospitalization, clinical manifestations on arrival, pre-hospital intervention by caretakers, type of management given, and an outcome that was measured as a binary outcome (whether the patients were discharged or died).
Data sources/measures
By using the registration number, database officers initially selected patients who had a poisoning diagnosis from the card office. After choosing the cards, trained data collectors filled out the prescribed formats, and the Principal Investigator (PI) verified the data every day to make sure it was accurate and consistent. The data-gathering tool had a pre-test, and changes were made as needed based on the results. To prevent double counting, the patient record numbers of those admitted from the emergency department to the medical intensive care unit were cross-checked.
Sample size and sampling technique
The sample size was estimated based on the following assumptions: The proportion of discharge rates was 61.2%, which was obtained from a study done at Jimma University Specialized Hospital [18]. A 5% marginal error and a 95% CI (1.96) were utilized. The calculated sample size was 382 using a single population proportion formula and a 5% non-response rate. However, as there were 218 poisoning cases during the study period, which was less than the estimated sample size, all data during the study period were included by utilizing a nonprobability convenience sampling method. Out of 218 charts, 183 contained all the data necessary for this study, making them eligible.
Statistical analysis
The SPSS version 26 software was used to code, clean, and create the registry on the computer for further study. The variables were described using basic descriptive statistics such as frequencies and percentages. To assess the association and statistical significance, an odds ratio with a 95% confidence interval was computed. Those variables that were found to be significant in bivariate analysis were retained for further multivariate analysis. To control confounding variables and forecast independent predictors of poisoning outcome, a multivariable logistic regression analysis was next performed. Statistical significance was defined as a p-value of 0.05 or lower.
Operational definitions
The outcome of acute poisoning: In this study, the outcome of acute poisoning was either discharge with improvement or inhospital mortality.
Rural: place of residence for cases that were admitted from areas surrounding Addis Ababa or outside Addis Ababa.
Adult: In this study, an adult was defined as a patient whose age was 13 years or older, according to our hospital protocol.
Urban: place of residence for patients who came from Addis Ababa.
Ethical approval
The study was carried out following approval by the departmental research review board and receipt of an ethical authorization report from the Addis Ababa University Department of Emergency and Critical Care Medicine with approval reference number (EM/SM/153/2021). Documents and information gathered during each course of study were kept confidential.
Participants and descriptive data concerning poisoning
In this study, 92 (50.3%) of the 183 patients were women and 91 (49.7%) were men. The median age of the patients was 27 years (interquartile range: 22-35 years; maximum age: 57 years). Most of them (75, or 41%) were aged 21 to 30 years. With regard to the place of residence, 158 patients (86.3%) were from urban areas and the remaining 25 (13.7%) were from rural areas (country districts). Most patients were self-referred, accounting for 146 (79.8%) (Table 1).
| Characteristics | Outcomes | ||
|---|---|---|---|
| Discharge (%) | Death (%) | ||
| Age | 13-20 | 32 (84.2) | 6 (15.8) |
| 21-30 | 61 (81.3) | 14 (18.7) | |
| 31-40 | 37 (90.2) | 4 (9.8) | |
| 41-50 | 15 (100) | 0 | |
| ≥ 51 | 13 (92.9) | 1 (7.1) | |
| Sex | Females | 74 (80.4) | 18 (19.6) |
| Males | 84 (92.3) | 7 (7.7) | |
| Place of residence | Urban | 147 (93) | 11 (7) |
| Rural | 11 (44) | 14 (56) | |
| Source of referral | Self | 135 (92.5) | 11 (7.5) |
| Government hospital | 14 (66.7) | 7 (33.3) | |
| Health center | 5 (45.5) | 6 (54.5) | |
| Private hospital | 4 (80) | 1 (20) | |
Table 1: Socio-demographic data on poisoning cases, according to outcomes at an Ethiopian tertiary care center from 2016 to 2021.
Triage classification
The majority of patients were triaged as red, which accounted for 95 (51.9%) cases, followed by orange, yellow, and green, which accounted for 38 (20.8%), 26 (14.2%), and 24 (13.1%) cases, respectively. All deaths (n=25) are shown in red (Figure 1).
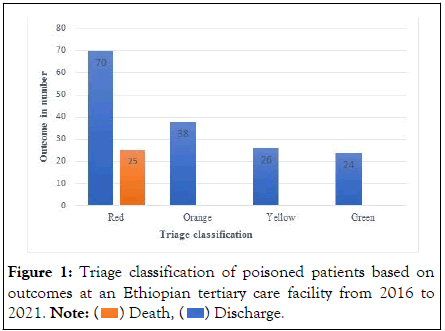
Figure 1: Triage classification of poisoned patients based on
outcomes at an Ethiopian tertiary care facility from 2016 to
2021.
Note: ( ) Death, (
) Death, ( ) Discharge.
) Discharge.
Name of toxic agents involved
Sodium hypochlorite was the most common poison identified and was ingested by 40 patients (21.9%), of whom 57.5% were male and 42.5% were female. This was followed in decreasing order by alcohol, rodenticides (aluminum phosphide and zinc phosphide), barbiturates, organophosphates (malathion), and carbon monoxide (18%, 12%, 11.5%, 10.9%, and 6%, respectively). Metformin (4.4%), acetaminophen (4.4%), opioids (3.8%), antidepressants (2.7%), and hydrocarbons (2.2%) were among the less frequent poisons. A specific toxin was not identified in four patients (2.2%). Rodenticides (n=10) were the most prevalent cause of mortality, followed by barbiturates (n=8) and organophosphates (n=5). Antidepressants (n=1) and opioids (n=1) were the two other less common causes of mortality (Table 2).
| Toxic agents | Sex | Outc`omes | Total (%) | ||
|---|---|---|---|---|---|
| Male (%) | Female (%) | Death (%) | Discharge (%) | ||
| Sodium hypochlorite | 23 (57.5) | 17 (42.5) | 0 | 40 (25.3) | 40 (21.9) |
| Alcohol | 28 (84.8) | 5 (15.2) | 0 | 33 (20.9) | 33 (18) |
| Rodenticides | 7 (31.8) | 15 (68.2) | 10 (40) | 12 (7.6) | 22 (12) |
| Barbiturates | 5 (23.8) | 16 (76.2) | 8 (32) | 13 (8.2) | 21 (11.5) |
| Organophosphates | 11 (55) | 9 (45) | 5 (20) | 15 (9.5) | 20 (10.9) |
| Carbon monoxide | 2 (18.2) | 9 (81.8) | 0 | 11 (7) | 11 (6) |
| Metformin | 4 (50) | 4 (50) | 0 | 8 (5.1) | 8 (4.4) |
| Acetaminophen | 3 (37.5) | 5 (62.5) | 0 | 8 (5.1) | 8 (4.4) |
| Opioids | 2 (28.6) | 5 (71.4) | 1 (4) | 6 (3.8) | 7 (3.8) |
| Antidepressants | 3 (60) | 2 (40) | 1 (4) | 4 (2.5) | 5 (2.7) |
| Hydrocarbons | 1 (25) | 3 (75) | 0 | 4 (2.5) | 4 (2.2) |
| Unspecified | 2 (50) | 2 (50) | 0 | 4 (2.5) | 4 (2.2) |
| Total | 91 (49.7) | 92 (50.3) | 25 (13.7) | 158 (86.3) | 183 (100) |
Table 2: Name of toxic agents involved according to outcomes with sex distribution at an Ethiopian tertiary care center from 2016 to 2021.
Situation of poisonings
Overall, 92.3% of intentional poisonings were reported, and the remaining 6% were unintentional. For three patients (1.7%), the situation was not recorded. Men (52.1%) attempted suicide more frequently than women (47.9%). All deaths (n=25) were caused by intentional poisoning.
Predisposing determinants or fundamental reasons for poisoning
One hundred and forty-six patients (79.8%) gave their reasons for poisoning. Family disputes accounted for 40.4%, followed by decreasing orders due to drug misuse (16.4%), epileptic seizures (10.4%), psychiatric illnesses (7.1%), and poor academic performance (5.5%). Family disputes (n=10) were the most common fundamental reason for those whose outcome was death, followed in decreasing order by epileptic seizures (n=8), psychiatric illness (n=2), poor academic performance (n=1), and drug misuse (n=1) (Table 3).
| Fundamental reason | Deaths (%) | Discharges (%) | Total (%) |
|---|---|---|---|
| Family dispute | 10 (13.5) | 64 (86.5) | 74 (40.4) |
| Drug misuse | 1 (3.3) | 29 (96.7) | 30 (16.4) |
| Epileptic seizure | 8 (42) | 11 (58) | 19 (10.4) |
| Psychiatric illness | 2 (15.4) | 11 (84.6) | 13 (7.1) |
| Poor academic performance | 1 (10) | 9 (90) | 10 (5.5) |
| Unidentified | 3 (8.1) | 34 (91.9) | 37 (20.2) |
| Cumulative | 25 (13.7) | 158 (86.3) | 183 (100) |
Table 3: Fundamental reasons for poisoning according to the outcome at an Ethiopian tertiary care center from 2016 to 2021.
Way of exposure
In this study, there were two methods of exposure. In 94% of the patients, the exposure was through ingestion, and in the remaining 6%, it was via inhalation. The cause of death (n=25) was ingestion.
The average period from exposure to hospitalization
The average time from poison exposure to arrival (which was grouped considering possible interventions within that time frame) at the emergency room was two hours (interquartile range, 30 minutes-96 hours). A total of 106 patients (57.9%) arrived in the emergency room within 24 hours, 33.9% within an hour, and 8.2% after 24 hours. The majority of deaths (n=11) occurred in patients who came after 24 hours.
Clinical manifestations on arrival
Prevalent manifestations were altered mentation (36.6%), of which 74.6% were discharged and 25.4% died; epigastric burning, fecal incontinence, and vomiting together (16.4%); fecal incontinence and vomiting alone (14.2%); and epigastric burning alone (10.9%) (Table 4).
| Main manifestations | Outcomes | ||
|---|---|---|---|
| Death (%) | Discharge (%) | Frequency(%) | |
| Altered mentation | 17 (25.4) | 50 (74.6) | 67 (36.6%) |
| Epigastric burning, fecal incontinence and vomiting | 1 (3.3) | 29 (96.7) | 30 (16.4) |
| Fecal incontinence and vomiting | 0 | 26 (100) | 26 (14.2) |
| Epigastric burning | 3 (15) | 17 (85) | 20 (10.9) |
| Altered mentation, epigastric burning, fecal incontinence and vomiting | 3 (18.75) | 13 (81.25) | 16 (8.8) |
| Altered mentation and headache | 0 | 7 (100) | 7 (3.8) |
| Headache | 0 | 5 (100) | 5 (2.8) |
| Fecal incontinence, vomiting, hypersalivation and urinary incontinence | 0 | 4 (100) | 4 (2.2) |
| Trouble breathes | 1 (50) | 1 (50) | 2 (1.1) |
| Shock | 0 | 2 (100) | 2 (1.1) |
| Epistaxis | 0 | 2 (100) | 2 (1.1) |
| Fecal incontinence, vomiting and headache | 0 | 1 (100) | 1 (0.5) |
| Hypersalivation, sweating, and urinary incontinence | 0 | 1 (100) | 1 (0.5) |
Table 4: Distribution of poisoning cases' main clinical manifestations according to outcomes at an Ethiopian tertiary care center from 2016 to 2021.
Prehospital intervention by caretakers
Eighteen patients (9.8%) received prehospital care, leaving 135 (90.2%) without family prehospital assistance. There were 25 fatalities, and none of them had received prehospital interventions.
Type of management given
Most patients were managed with fluid therapy and anti-acid therapy (46.4%), and 15 patients (8.2%) received particular reversals as the main treatment. All the patients who were both dialyzed and intubated died (Table 5).
| Types of management given | Outcomes | ||
|---|---|---|---|
| Death (%) | Discharge (%) | Frequency (%) | |
| Fluid therapy and anti-acid | 4 (4.7) | 81 (95.3) | 85 (46.4) |
| Fluid therapy | 1 (5.3) | 18 (94.7) | 19 (10.4) |
| Reversals (phytonadione, naloxone, and atropine) | 5 (33.3) | 10 (66.7) | 15 (8.2) |
| Oxygen | 0 | 11 (100) | 11 (6.0) |
| Analgesics and anti-acid | 0 | 10 (100) | 10 (5.5) |
| Gastric lavage and particular reversals | 1 (11.1) | 8 (88.9) | 9 (4.9) |
| Dialysis | 1 (11.1) | 8 (88.9) | 9 (4.9) |
| Intubation | 6 (66.7) | 3 (33.3) | 9 (4.9) |
| Gastric lavage | 0 | 9 (100) | 9 (4.9) |
| Dialysis and intubation | 7 (100) | 0 | 7 (3.8) |
Table 5: Distribution of the major managements given for poisoned patients with their outcomes at an Ethiopian tertiary care center from 2016 to 2021.
The outcome of poisoning
Most patients (n=144) were discharged from the ED, of whom 49 were linked to a psychiatry clinic and six were linked to a neurology unit. The ED recorded 17 deaths with a mortality rate of 10.56%. Eight of the 22 patients admitted to the Medical Intensive Care Unit (MICU) died, while 14 improved and were discharged, giving the MICU death rate of 36.36%. Overall, 86.3% of the patients were discharged, and 13.7% died (Table 6).
| Deaths (%) | Discharges (%) | Cumulative (%) | |
|---|---|---|---|
| Emergency department | 17 (10.56) | 144 (89.44) | 161 (88) |
| Medical-ICU | 8 (36.36) | 14 (63.64) | 22 (12) |
| Cumulative (%) | 25 (13.7) | 158 (86.3) | 183 (100) |
Table 6: Distribution of poisoning case outcomes by the frequency at an Ethiopian tertiary care facility from 2016 to 2021.
Determinant factors in the outcome of poisoning
Initially, different variables were considered for the bivariate analysis. In the bivariate analysis, the following variables showed a statistically significant association with the outcome: Male sex (OR=2.919, 95% CI=1.155-7.378), being from an urban place of residence (OR=17.008, 95% CI= 6.260-46.209), arriving within an hour (OR=31.350, 95% CI=7.247-135.624), arriving within 24 hours (OR=29.639, 95% CI=7.818-112.366), having epileptic seizures as the fundamental reason (OR=0.121, 95% CI=0.027-0.539), and management accompanying intubation (OR=16.0, 95% CI=1.315-194.623, p=0.030). These variables were combined and analyzed using a multivariate logistic regression model. After controlling for the effects of potentially confounding factors using a multivariate logistic regression model, being from an urban place of residence and management accompanying intubation were found to be statistically significant predictors of the outcome. Relative to rural areas, being from an urban place of residence was strongly associated with discharge (Adjusted Odds Ratio (AOR)=6.384, 95%confidence interval (CI)=1.270–32.098, p=0.024). Relative to the other main management options, the need for intubation was associated with a lower chance of discharge (AOR=0.045, 95% CI=0.003-0.776, p=0.033) (Table 7).
| Variables | Outcome | COR (95% CI) | AOR (95%CI) | p-value | ||
|---|---|---|---|---|---|---|
| Discharge (%) | Death (%) | |||||
| Sex | Males | 84 (92.3%) | 7 (7.7%) | 2.919 (1.155-7.378) | 0.557 (0.115-2.702) | 0.467 |
| Females | 74 (80.4%) | 18 (19.6%) | 1 | |||
| Place of residence | Rural | 11 (44%) | 14 (56%) | 1 | ||
| Urban | 147 (93%) | 11 (7%) | 17.008 (6.260-46.209) | 6.384 (1.270-32.098) | 0.024* | |
| Average period to arrival | <1 hr | 57 (91.9%) | 5 (8.1%) | 31.350 (7.247-135.624) | 3.016 (0.199-45.791 | 0.426 |
| 1-24 hr | 97 (91.5%) | 9 (8.5%) | 29.639 (7.818-112.366) | 12.833 (0.925-177.932) | 0.057 | |
| >24 hrs | 4 (26.7%) | 11 (73.3%) | 1 | |||
| The fundamental reason for poisoning | Psychiatric illness | 11 (84.6%) | 2 (15.4%) | 0.485(0.072-3.290) | 0.339(0.025-4.547) | 0.414 |
| Drug misuse | 29 (96.7%) | 1 (3.3%) | 2.559(0.252-25.954) | 2.195(0.127-37.859) | 0.588 | |
| Epileptic seizure | 11 (57.9%) | 8 (42.1%) | 0.121(0.027-0.539) | 1.706(0.106-27.552) | 0.706 | |
| Family dispute | 64 (86.5%) | 10 13.5%) | 0.565(0.146-2.191) | 1.214(0.172-8.581) | 0.846 | |
| Poor academic performance | 9 (90%) | 1 (10%) | 0.794(0.074-8.576) | 5.104(0.149-174.584) | 0.366 | |
| Unidentified | 34 (91.9%) | 3 (8.1%) | 1 | |||
| Type of management | Reversals | 10 (66.7%) | 5(33.3%) | 4.000(0.385-41.511) | 0.299(0.025-3.582) | 0.34 |
| Fluid therapy | 18 (94.7%) | 1 (5.3%) | 0.444(0.025-8.031) | 1.528(0.074-31.651) | 0.784 | |
| Intubation | 3 (33.3%) | 6(66.7%) | 16.000(1.315-194.623) | 0.045(0.003-0.776) | 0.033* | |
| Dialysis | 8 (88.9%) | 1 (11.1%) | 1.000(0.053-18.915) | 4.035(0.092-176.596) | 0.469 | |
| Fluid therapy and anti-acid | 81(95.3%) | 4(4.7%) | 0.395(0.039-3.974) | 1.875(0.173-20.287) | 0.605 | |
| Gastric lavage and reversals | 8 (88.9%) | 1 (11.1%) | 1 | |||
Note: COR=Crude Odds Ratio; AOR= Adjusted Odds Ratio, *p-value ≤ 0.05 is statistically significant.
Table 7: Association of determinant factors with the outcome at an Ethiopian tertiary care center from 2016 to 2021.
In this study, the overall fatalities were 13.7%, which was greater than those reported in a previous study in a similar study area (8.6%) [15], Jimma University Specialized Hospital (5.8%) [18], Ambo Town (1.5%) [16], Adama Hospital (1.37%) [19], Tanzania (0.9%) [20], South Africa (2.4%) [3], and China (1.3%) [21].
This difference might be due to an increase in the referral of critical patients from the periphery, differences in the specific causes of poisoning, and differences in the study area and setup. The overall discharge rate in this study was 86.3%, which was higher than that reported in a study conducted at JUSH (61.2%) [18].
Most patients were female (50.3%), which was similar to a study conducted in South Africa (57.8%) [3], Jimma University Specialized Hospital (52.4%) [18], and a previous study conducted in the same study setting (64.6%) [15]. Most patients were from urban residences (86.3%), which was similar to a previous study in a similar study setting (89.6%) [15]. Family disputes were the most common reason for poisoning (40.4%), which was higher than a study done at Ambo (35.9%) [16] but lower than that of a study conducted at Jimma University Specialized Hospital (75.9%) [18], and a previous study from a similar setting (57%) [15]. Most of the patients (57.9%) arrived within 24 hours, which showed that there was a delay in arrival as compared to a study done at a Jimma University specialized hospital in which 54.2% arrived within an hour [18], Ambo Town (every patient arrived within 5 hours) [16], and a previous study in a similar study setting (94.3% arrived within 12 hours) [15]. This difference may be due to an increase in referrals from the periphery and traffic overcrowding in the city.
The majority of patients (46.4%) were treated with fluid therapy and anti-acids. Only 4.9% of patients were managed with gastric lavage, which was lower than that reported in studies conducted in Adama (56.6%) [19], Jimma University Specialized Hospital (78.6%) [18], and China (72.5%) [21]. In contrast to our study, in which no patients received activated charcoal for GI decontamination, a study conducted in China indicated that 64.8% of patients received it [21]. The lower performance of GI decontamination in our study may be due to the delayed arrival of patients and the unavailability of activated charcoal. Particular reversals were administered to 8.2% of patients, which was lower than the 12.6% and 37.8% of patients treated with reversals in research conducted at the Jimma University Specialized Hospital [18] and Adama [19], respectively. The difference in the use of specific reversals might be due to differences in the specific types of poisoning and the availability of antidotes. Oxygen was used as the main management option in 6% of patients, which was higher than that reported by Adama (1.7%) [19]. This difference might be due to the number of patients who were poisoned by CO relative to the sample size. Hemodialysis was performed for 4.9% of patients, which was lower compared to a study in China (7.7%) [21]. This difference may be due to the specific causes that require hemodialysis and the availability of hemodialysis services.
This study found that relative to rural areas, being from an urban place of residence was strongly associated with discharge, or patients who came from rural areas were more likely to die than those who were from urban residences. This could be because patients who live in urban areas can easily access the hospital and get treatment early, whereas patients who come from rural areas might be more critical.
Relative to other main management options, patients who required intubation were less likely to be discharged and intubation was strongly associated with death. This might be because patients who had an indication for intubation might be more critical and have a lower chance of survival as compared to those who did not require intubation. The other reason might be due to poor close follow-up and care in the MICU for intubated patients.
In this study, the overall case fatality rate was 13.7%, which was very high compared with the findings of other studies. The most common cause of poisoning in this study was a household cleansing agent (sodium hypochlorite). The most common causes of death were ingestion of rodenticides, barbiturates, and organophosphates. Gastric lavage and administration of specific reversals were performed in only a few patients. Most deaths occurred in patients who arrived after 24 hours. The independent predictors of outcomes were the need for intubation and being from an urban place of residence.
This was a hospital-based single cross-sectional study with a retrospective chart review that may not have established trends or causality between outcomes and potential risk factors. The retrospective nature of the study prevented us from collecting detailed clinical and laboratory data to determine the severity of the cases and to calculate the Poisoning Severity Index (PSI) as a determinant of outcome. The patients’ medical records lacked completeness and uniformity, which made the study variables incomplete.
The authors appreciate the invaluable work put in by the central data management team during the data collection procedure. We also thank Dr. Natnael Moges for his assistance with manuscript editing. We appreciate the opportunity to conduct research provided by the Department of Emergency and Critical Care Medicine as well as the assistance of Addis Ababa University.
The corresponding author can provide the data used to support the study's conclusions upon request.
Belayneh Dessie Kassa is responsible for the work's idea, design, data collection, analysis, and interpretation. The study's and the manuscript's core intellectual substance were drafted by Sofia Kebede and Berhanu Tesfaye, or critically revised by them.
The writers claimed there was no potential conflict of interest. All authors gave their approval for the final draft to be published and agreed to be held accountable for all facets of the work.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kassa BD, Tesfaye B (2023) Outcome and Determinants of Adult Poisoning at an Ethiopian Tertiary Care Center: A Five-Year Retrospective Data Analysis. J Clin Toxicol. 13:543.
Received: 16-Jun-2023, Manuscript No. JCT-23-25163; Editor assigned: 19-Jun-2023, Pre QC No. JCT-23-25163 (PQ); Reviewed: 03-Jul-2023, QC No. JCT-23-25163; Revised: 10-Jul-2023, Manuscript No. JCT-23-25163 (R); Published: 17-Jul-2023 , DOI: 10.35248/2161-0495.23.13.543
Copyright: © 2023 Kassa BD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.