International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Review Article - (2021)Volume 9, Issue 1
Background: Attention-deficit hyperactivity disorder is identified as a neurobehavioral disorder characterizing inattention, hyperactivity, impulsivity and functional impairment. Motor impairments are rarely part of assessments and typically not treated in ADHD. The outcome measures used for motor impairments lack consensus, limiting a uniform approach to rehabilitation. Therefore, a review of the literature to underline and verify outcome measures for motor impairments in ADHD in the pediatric population is needed.
Methodology: A scoping review was conducted following the PRISMA-Sr guidelines to assess and categorize outcome measures used for motor impairments in the pediatric ADHD population. Pubmed Central, Embase, and the Cochrane Library were searched for publications between 2009-2019 that reported on Motor impairments in pediatric ADHD and mentioned related outcome measures. The data are presented using a ‘narrative review’ or descriptive analysis of the contextual or process-oriented data and simple quantitative analysis using descriptive statistics.
Results: 22 studies were included: 4 randomized controlled trials, 11 observational studies, and 7 experimental studies. The outcome measures found in the studies showed a divided application with no uniformity in their use as a prognostic or diagnostic measure.
Conclusion: This review highlights the lack of uniformity in the outcome measures used for motor impairments in pediatric ADHD.
Pediatric; ADHD; Motor impairments; Outcome measures; Scoping review
Attention-deficit hyperactivity disorder (ADHD) is a commonly identified neurobehavioral disorder characterized by inattention, hyperactivity, impulsivity, and related functional impairment [1]. According to the Centers for Disease Control and Prevention (CDC), 5 million children (9%) between 3 and 17 years of age have been diagnosed with ADHD in the last decade. On a worldwide scale, ADHD prevalence increased from 5.29% in 2007 to 5.9%- 7.1% in 2012, with the latest meta-analysis estimating it at 7.2% [2]. The disorder is highly comorbid: 40% to 65% children also meet the criteria for disruptive behaviour disorder [3]. If left untreated, these children are likely to have impairments that persist into adulthood altering their educational, occupation and personal outcomes [4]. ADHD has a multidimensional effect on daily functioning, incurring significant costs, attributable to greater health care needs and lost productivity.
Motor skills can be described as synergistic actions between the central nervous system, peripheral systems and muscles [5]. They are functions that involve the precise movements of muscles with the intent to perform specific actions. They are categorised into two groups: gross motor skills and fine motor skills. Gross motor skills are involved in movement and coordination of the arms and legs and actions such as running, crawling and swimming [5]. Fine motor skills are required in smaller movements that occur in the wrists, hands, fingers, feet and toes and include more precise actions such as picking up objects between the thumb and finger and writing carefully [6]. Poor fine motor skills can make cognitive learning and performance more difficult because of the involvement of fine motor skills in cognitive activities [7]. Children with ADHD who experience motor difficulties often display deficits in tasks requiring coordination of complex movements, such as handwriting. Such children often appear clumsy and uncoordinated.
The prevalence of motor problems in children with ADHD ranges from 30% to 52%, depending on the method of measurement [8,9]. A study by Pitcher et al. [10] found that 58% of children with ADHD (predominantly inattentive subtype), 49% with ADHD combined and 47% with ADHD hyperactivity and impulsiveness had motor problems. In clinics, less attention is paid to the motor component of ADHD as compared to the attention for psychiatric comorbidities like depression, autism, oppositional defiant disorder and conduct disorder [11].
Kadesjo and Gillberg [12] and Piek et al. [13] conclude that inattentive symptoms relate mostly to motor coordination problems, though a relationship between hyperactive and impulsive symptoms and motor coordination problems has also been reported. Motor problems lead to difficulties in everyday living, including academic performance, sport, play and selfesteem. Motor problems severely affect children’s daily lives and are an active predictor of a child’s popularity and self-esteem [14]. These deficits may have an intense effect on child’s development, leading to difficulty with written communication, inhibited social interaction and poor performance in sports activities.
Motor problems are not usually part of assessments for ADHD and are not included in intervention programmes despite the estimate that 30%–50% of children with ADHD exhibit motor problems [15]. The goal of ADHD treatment is the improvement of quality of life of the child; and gaps in treatment strategies for motor deficits in paediatric ADHD care have been established in the literature.
An outcome measure, endpoint, effect measure or measure of effect is a measure which is used to assess the effect, both positive and negative, of an intervention or treatment [16,17]. It is a tool used to assess a patient’s current status [18]. Outcome measures often provide a score, an interpretation of results and at times, a risk categorization of the patient. With the move towards Evidence Based Practice (EBP) in health care, outcome measures provide credible and reliable justification for treatment on an individual patient level [18]. Outcome measures in physical therapy practice prove important to assess the effectiveness of treatment interventions, providing accountability and addressing quality of physical therapy programs. The validity and reliability i.e. the psychometric properties of an outcome measure help to establish the universality of the test and help in maintaining uniformity in assessment and treatment measures.
Along with scarcity of studies investigating motor impairments in ADHD; very rarely we are able to see a consensus regarding use of outcome measures to assess and measure improvement of this aspect. The determination of improvement in functional impairment remains a clinical decision and no standardized assessments or measures are applied in practice. This exposes a lack of uniformity and objectivity in diagnosing and treating motor impairments in ADHD causing a conflict in assessment and treatment options.
As seen in the above-mentioned studies, there has been an increasing trend in diagnosis of ADHD in the pediatric population all over the world, with motor impairments posing a challenge to be dealt with [19]; however, the extent of available literature remains unclear. This poses a query for understanding if there is sufficient evidence available to develop practice recommendations, whether or not a systematic review is feasible to conduct and if there is a gap in knowledge, where that gap exists.
A scoping review is a relatively new and developing methodology for systematically analysing existing literature [20]. As such, there are a number of definitions of and approaches to conducting a scoping review [20]. Scoping reviews help to systematically chart or map the literature available on a topic, identifying key concepts, theories, sources of evidence and gaps in the research. When there are a variety of sources and types of available evidence, scoping reviews can be used to describe key concepts within a specific research area, enabling identification of strengths and weaknesses within the literature, as well as emerging conceptual observations across a broad range of available evidence.
The purpose of this project was to conduct a comprehensive, scoping review to identify and chart the breadth of literature related to outcome measures used to diagnose and assess motor impairments in ADHD in the paediatric population.
A scoping review was conducted according to the PRISMA-ScR [20] statement where applicable. This scoping review involved five steps: (1) formulating a research question; (2) establishing an inclusion criteria to identify and include studies; (3) identification of relevant studies across a broad range of potential evidence; (4) independent and objective screening and selection of studies for inclusion; (5) extraction and charting of the data according to key concepts identified; and (5) and summarization of the findings for clinical relevance and future research.
Inclusion criteria
To be included in the review, studies met the following criteria:
Publication type: There were no restrictions on type of study; however, only papers published in peer reviewed journals published between 2009 and 2019 were included.
Participant characteristics: Participants were in the pediatric or adolescence-age group of 4-17 years of age diagnosed with Attention deficit hyper-activity disorder.
Outcome measures: The studies containing data on the relationship between Pediatric ADHD and motor impairments
Language: The studies written in English.
Information sources: Studies were identified by searching the following electronic databases: Google Scholar, Cochrane, Pubmed, EBSCO, and CINAHL. The search was conducted over a period of 4 months.
In addition, reference lists of the included studies were screened for potentially eligible studies.
Search strategy: The search strategy was to include the study population using terms and keywords prior decided:
The following MESH terms were used for the search: ADHD, Pediatric, Motor impairment/functions/skills, Outcome measures, Children.
Study selection: Study selection was initially performed by the first author and then checked by the second author. First, the titles and abstracts of the publications retrieved by electronic searching were screened. Second, potentially eligible studies were retrieved full text before definitive inclusion. In the case of disagreement between the two authors, the last author was consulted to decide whether a study should be included.
Data collection process: Using a standardized form, two reviewers extracted the data independently. A third reviewer independently checked the data for consistency and clarity.
Data extraction: Data was extracted from the studies by the first author and then checked by the second author. The extracted data was discussed until consensus was reached. Assent of the third author was taken. No specific form was used for data extraction; however, the outcomes to be extracted were defined prior.
The following information was extracted from each study: Author and Year of publication, Study design,Outcome measures used for, Diagnosis purpose, Assessment purpose, Physiotherapy intervention given for motor impairments
Analysis: The data were presented using a ‘narrative review’ of the process-oriented data and simple quantitative analysis using descriptive statistics.
Risk of bias in individual studies: Risk of bias for each included trial was independently assessed by the same initial reviewers. The third reviewer mediated in situations of disagreement.
The initial search revealed 177 articles including 25 articles found through additional sources. Of which 114 were duplicates resulting in 63 distinct potential articles. The articles were then screened by two reviewers; 16 articles were excluded. The article titles, abstracts and full text of the 47 remaining articles were then reviewed. Of the 47, 35 articles could be retrieved as full texts and were screened. 22 articles met the inclusion criteria and were reviewed for the final review. The primary reasons for excluding articles were that those were duplicate articles, full text of the articles could not be retrieved or that the articles did not meet the inclusion criteria (Figure 1).
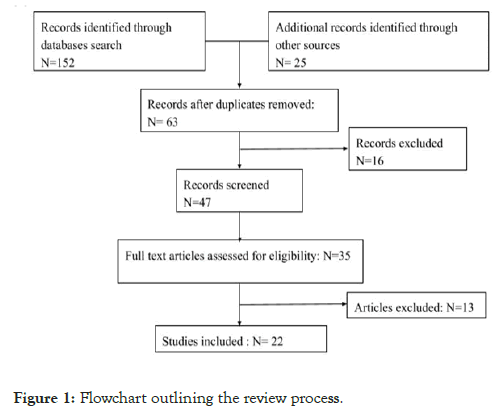
Figure 1: Flowchart outlining the review process.
Types of research
The selected studies were published between 2009 and 2019. Out of the 22 studies included; four were randomized control trials with two of them having Physiotherapy interventions as an adjunct to psychological and pharmacological interventions [21,22]. Seven articles were experimental studies and 11 were observational studies. Five of the seven experimental studies had Physiotherapy being given to the participants. The interventions used were: Virtual gaming protocol, High intensity interval training, Balance training, Strengthening protocols, Hippo therapy [23-29].
Types of motor impairments
Studies that were reviewed had participants who were diagnosed as ADHD and had motor impairments as well [30-35]. The motor impairments targeted were: Balance, Handwriting, Manual dexterity, Ball skills (catching and throwing balls), Overall, the fine motor skills were targeted and not the gross motor skills.
Outcome measures used
Multiple outcome measures were used in all the studies as a measure of diagnosis, assessment or as a prognostic measure. Outcome measures were also used as a measure of severity. However, it was found out that no two studies used the same outcome measure in the same way while being used for assessing motor impairments. The participants studied ranged from the age group of 4 years to 17 years and were school going. The outcome measures were classified according to their purpose in the study:
• Used for Assessment of motor impairments
• Used for diagnostic purpose/prognostic purpose
• Administered by a physiotherapist/other personnel
It was found out that DSM-IV and SNAP IV were used in six of the studies administered by parents or teachers to diagnose the children as ADHD. The rest of the studies had pre-diagnosed cases of ADHD in them.
There were four studies that had the parent administered child behavior checklist (CBCL) as an outcome measure to clinically assess the psychological and physical impact of ADHD on children. Pediatric Quality of life scale (PedQol) and ADHD Rating scale were used to ascertain the severity of ADHD in the child’s life. These two scales were administered by teachers, by parents and by therapists individually in one study each.
The therapist administered clinical global impression scale has two components: severity and improvement. Severity component of the therapist administered clinical global impression scale was used as an assessment measure in an individual study and the improvement component was used in another study. To assess the severity of symptoms faced by the child, the Strength and difficulty quotient scale (SDQ) and Conners 3 questionnaire were used by teachers or therapists whereas Physical and Neurological Examination of Soft Signs (PANESS) was a test administered by psychologists in a study.
The outcome measures used to assess the motor impairments in children were:
Purdue pegboard test: Used in 2 studies.
Motor assessment scale: Used in 1 study.
BOT-2 (Bruininks-Oseretsky Test of motor proficiency): Used in 2 studies.
German Motor Test: Used in 1 study.
Movement assessment battery for children-2 (Mabc-2): Used in 4 studies.
It was found that though motor impairments were included in the studies, psychological and behavioral impairments were preferred areas of consideration as compared to motor impairments. Motor impairments were considered as secondary affections in these studies and were not the primary focus.
This scoping review suggests that there are very few studies done in the Pediatric ADHD population with motor impairments being targeted. Though outcome measures were used in all the studies, the capacity in which they were used or the functions that they targeted differed in each study.
There are studies done that correlate ADHD with motor impairments and studies that compare pharmacological treatment with physiotherapy measures. A study done in 2020 suggests that ADHD medication treatments are associated with decreases in the risks for a wide range of ADHD-associated functional outcomes supporting efforts aimed at early diagnosis and treatment of individuals with ADHD [20]. Studies have shown that without treatment (non-pharmacological and behavioural), people with ADHD had poorer long-term outcomes in all categories compared with people without ADHD. Research also showed that treatment for ADHD improved long-term outcomes when compared with untreated ADHD, although not usually to normal levels [36].
There is strong evidence for the clinically significant co-existence of ADHD and motor coordination problems, several aspects regarding the association remain unclear. There are very few studies that have investigated these motor problems as an integral symptom of ADHD. A review done on impaired motor skills and motor control among children with ADHD concluded that it is important to assess motor skills among children with ADHD because of the risk of reduced participation in activities of daily living that require motor coordination and attention [37].
A study put forth a literature synthesis on the efficacy and effectiveness of guideline-recommended ADHD treatments on patient outcomes which showed that DSM-criteria-based rating scales were used most frequently to measure ADHD treatment outcomes. All included treatments resulted in ADHD improvement. Regardless of outcome measure, tool, or treatment type, symptom reduction and improvement were relatively large [38]. This goes on to show the lack of uniformity in the outcome measures being used and thus can affect the quality of assessment and treatment these patients receive worldwide.
A critical review done in 2017 underlines the highly prevalent link between ADHD and developmental coordination disorder (DCD) and the lack of a clear research consensus about motor difficulties in ADHD. It hypothesizes that even in view of increasing evidence and diagnostic classifications that define DCD by motor impairment, the role of ADHD symptoms in DCD has not been delineated [39].
In view of the increase of ADHD symptoms in children in the last decade, it has become increasingly clear that there is a need to put forward an outline about the assessment and treatment outcomes. There is no classification available to categorize outcome measures that can be adapted universally, and which can help to establish a uniformity in the assessment and treatment methods.
Guidelines regarding outcome measures to be used for motor impairments will help to improve the quality of care and establish universality in management of ADHD. The studies mentioned outcome measures Snap IV and DSM IV which are used on a wide scale to diagnose by clinicians and can be administered by teachers and care takers as well.
The outcome measures that target the motor impairments were different in most of the studies as the motor impairments being targeted were different. Majority of the studies targeted fine motor impairment with gross motor skills being ignored.
This review highlighted the gaps that are present in the definition of motor impairments in association with ADHD, the outcome measures used to assess did not show universality and exposed a paucity of literature with regards to motor impairments and ADHD.
The outcome measures found in the studies showed a divided application with no uniformity in their use as a prognostic or diagnostic measure. This study showed paucity of literature connecting outcome measures with motor impairments in the pediatric ADHD population.
Further studies can be conducted to analyze the psychometric properties of the outcome measures and systematically review the literature relating to Physiotherapy and ADHD.
Studies can also be conducted targeting the motor impairments in the adult ADHD population.
The primary limitation of this scoping review was that it did not involve quality assessment of the included studies. As such, this scoping review cannot be generally regarded as a final or definitive literature synthesis from which practice guidelines or policy decisions can be based. Rather, it can be said that this review was conducted primarily for the purpose of identifying and mapping the breadth, rather than the quality of current literature in an area of research with broad-reaching clinical relevance and/or diverse research directions.
Another issue for this review was that the non-English publications were not captured.
And only articles with open access were included.
No conflict of interest noted by the authors.
Citation: Gadgil RR, Kotwal A, Akulwar IS (2021) Outcome Measures for Motor impairments in Pediatric Attention Deficit Hyperactivity Disorder: A Scoping Review. Int J Phys Med Rehabil. 9:583.
Received: 15-Jan-2021 Accepted: 29-Jan-2021 Published: 05-Feb-2021 , DOI: 10.35248/2329-9096.21.9.583
Copyright: © 2021 Gadgil RR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.