Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2022)Volume 11, Issue 4
Background: In Ethiopia, the levels of maternal and infant morbidity and mortality are among the highest in the world. This is attributed to, among the major three delays contributing to maternal mortality other factors, lack of service access predisposing them to delay reaching health facilities none use of modern health care services by women. Despite the advances in modern obstetrics care, maternal morbidity and mortality remain a big problem. Proper place and choice in the mode of delivery are necessary to tackle this problem. An integrated Emergency surgical officer is a health professional qualified and authorized to perform emergency obstetrical-gynecological and emergency general surgical procedures. The training has started in 2010 in 3 universities and 10 affiliated sites with an intake of 43 students. Objective: This study aimed to assess Indication, maternal and fetal outcome of cesarean section and associated factors, in Felegemeles Health center, Addis Ababa Ethiopia. Methods: Facility-based two-year retrospective descriptive cross-sectional study design was employed and data was collected from January 2017 to January 2019 at Felegemeles Health center, Addis Ababa Ethiopia. A total of 465 mothers who delivered by cesarean delivery from January 2017 to January 2019 and complete data were included in the study. Data were extracted using structured data collection format and cleaned, entered into Epi data software version 3.1, and exported into SPSS version 26 for further descriptive analysis. Result: Among 1583 deliveries in the two years of retrospective data, a total of 465 mothers were delivered by cesarean section, giving a cesarean delivery rate of 29 %. The leading indication for cesarean delivery was CPD followed by fetal distress. Among the total cesarean delivery, 09 neonates were died, giving the proportion of neonate mortality rate 5.6 per 1000 live births. Independent risk factors found to be statistically associated with cesarean section were Spinal anesthesia (AOR=15.6, 95%CI: 6.12, 40.0), un-booked ANC (AOR=3.5, 95%CI: 1.24, 10.33), and maternal age 35 years and above (AOR=3.2, 95%CI: 1.47, 6.85). Conclusion: Zero maternal mortality in our finding shows, CEMONC health center task sharing has impacts on the reduction of maternal mortality even though, the cesarean delivery rate in this study was above the WHO recommended range. Age 19-29, Residency and Spinal Anesthesia have an association with adverse neonatal outcomes following cesarean delivery. The neonatal mortality following cesarean delivery was 5.6 per 1000 live births respectively and the main cause of neonatal death was birth asphyxia. maternal delay for seeking care needs to be improved in communication with health extension care workers and ANC care providers while Skills of anesthesia care providers, management of hypotension at time of spinal anesthesia provision needs improvement which among all needs further study at other CEMONC Health centers before the conclusion of findings.
Cesarean section rate, CEMONC health center, IESO, cross-sectional, Task shift & Addis Ababa Ethiopia.
Reduction of maternal and neonatal mortality remains a major challenge to attaining global social and economic development. Worldwide, more than 515,000 women die each year from pregnancy and childbirth complications while four million babies die within the first week (neonatal period) of life. Almost all of the maternal deaths occur across all developing countries where 450 women per every 100,000 live births die during pregnancy, childbirth, or at postpartum period [1,2].
The maternal mortality ratio (MMR) and proportion of births attended by skilled personnel are important indicators of quality maternal health. Maternal and child health care begins with the immediate health problems of mothers and children and extends to health throughout life and the health of the community [3].
Ethiopian Ministry of Health (EMOH) has applied multi-pronged approaches to reduce maternal and newborn morbidity and mortality, improve access to and strengthen facility-based maternal and newborn services is one such approach and is also a major issue of concern in Health Sector Transformation Plan II 2015/16– 2019/20 of Ethiopia [4].
Childbirth is a normal physiological process and a significant emotional event in a woman's life. While the proper choice of interventions is proven to be associated with the highest safety and effectiveness to reduce maternal and neonatal morbidity and mortality [5].
Cesarean section (C/S) is a surgical intervention designed to prevent or treat life-threatening maternal or fetal complications [6]. A Caesarean section is often performed when a vaginal delivery would put the baby's or mother's life or health in danger. Some are also performed upon request without a medical reason to do [7].
Establishing and functioning Operating Theater at the health center level is an innovative idea for Ethiopia as it changes the working culture. According to the Ethiopian health care tier system, Health Centers is defined as Primary health care unit constructed to address preventive, curative, and rehabilitative health care services for the community of 25,000 populations in rural and 40,000 populations in urban society respectively.
In Ethiopia, around 4000 health centers have been constructed among 420 Operating theater blocks had been innovated on prior health centers providing the basic services and functioning with limited numbers of Operating Theater Blocks are providing emergency surgical services due to lack of budget, equipment's and supplies and number of human resources especially trained Integrated Emergency surgical officers [8,9].
Establishing Operating Theater Blocks at the health centers level is expected to share the surgical and Anesthesia burdens from tertiary and general hospitals as a mechanism to bring Access to surgical services at the district/woreda level attributed to the reduction of morbid complications for both mothers and newborns by enabling timely surgical interventions, avoid delay in reaching a health facility, bring down unnecessary referrals and finally improves client satisfaction on the health center care facilities [10].
CEmoNC Task shared to health center level gives a room for specialized, tertiary, general, and primary hospitals to deal with major elective and complicated cases enable them to also shorten waiting lists for surgeries and surgical backlogs in return will help the facilities to become center of excellence in teaching medical and paramedical students and do research [11].
Ethiopia is well-known for high maternal, perinatal, and infant mortality rates and traumas related to morbidity and mortality. Therefore, reduction of the morbidities and deaths in our country will require a shift in the strategy that will ensure that majority of emergencies and births are attended by appropriately trained and skilled healthcare professionals including nurses, midwives, health officers, and doctors able to prevent, detect and manage obstetric complications and surgical emergencies [12].
Emergency surgical officers in Ethiopia are capable to handle common emergency obstetrical gynecological and emergency general surgical procedures including trauma at accessible locality after 3 years of intensive training on integrated emergency surgery [13]. Though the safety of cesarean section has improved, to date the morbidity rates are still high compared to vaginal delivery [8]. According to the world health organization, the cesarean section rate in any population should lie within the range of 5–15% [14].
Hence, evidence on the magnitude, indication, and maternal and fetal outcome of cesarean section at the health center level is not available in Ethiopia [15]. This study aimed to assess Indication, maternal and fetal outcome of cesarean section and associated factors, at Felegemeles Health center, Addis Ababa Ethiopia [16,17].
Study Setting
The study was conducted at Felegemeles Health Center located in Addis Ababa, Addis Ketema sub-city. The service has been operating since January 2013. The Health Center provides services for more than 33,182 residents in the catchment areas of sub- city, out of catchment sub-city, and out of Addis; surrounding Oromia special zones at outpatient and inpatients. The health center provides inpatient service with 16 beds and 02 delivery couches. Cesarean section services are the main surgical procedure done at the health center. There are three integrated emergency surgical professional specialists, two General practitioners, three anesthetics, ten midwives, thirty nurses, 7 lab technicians, fourteen health officers, and eighty-three administrative staff.
Study Design
A facility-based cross-sectional retrospective study was conducted from January 2017 to January 2019 at Felegemeles Health center. A total of 1583 mothers are delivered during the period and 465 women were delivered by cesarean section.
Inclusion Criteria
All cesarean sections performed after a period of viability (28 weeks) including elective, emergency, and primary cases are included in the study.
Exclusion criteria
Charts with incomplete information.
Cesarean section has done before or after the specified period of study.
Study Participants, Sample Size and Sampling Procedure
All women who delivered by cesarean section between January 2017 to January 2019 at Felegemeles Health center were the population under the study.
All cesarean deliveries including elective, emergency, and primary cases are included in the study.
The charts of all 465 mothers who gave birth by cesarean section during the retrospective period were reviewed.
Data Collection Tool and Procedure
Data were collected using a pre-tested structured questionnaire using the chart review method. The questionnaire consists of socio- demographic variables, obstetric history, and outcomes of cesarean section.
Mother’s information including age, parity, gestational age, antenatal care, and fetal condition at admission, Information was obtained from operation theatre and labor ward records. The questionnaire was prepared in English. Two BSc midwifery as data collectors and one health officer as supervisors were recruited for the study. Two days of intensive training regarding the objective of the study, confidentiality of information, and techniques to conduct the interview were given to data collectors and supervisors. To address the ethical issues, the data collectors were recruited among the permanent employees of the respective health center.
Data Processing and Analysis
Data were entered into Epi-data version 3.1 and exported to SPSS version 26 for further analysis. Data cleaning was done by running descriptive statistics, including frequency, tables, figures, Measures of central tendency, measures of dispersion, and proportions were computed to summarize the study variables. Bivariate analysis was used to examine the association between dependent and independent variables. A 95 % CI and P-value of < 0.05 were considered to be statistically significant. In addition, adjusted odds ratios were computed to assess the effect of each independent variable on the outcome variables multivariate logistic analysis was carried out and fit the final model.
Ethical clearance
Ethical clearance was obtained from the institutional review board of St. Paul millennium Hospital and Millennium Medical, Public health department. Permission from Felegemeles health center was obtained before activities started. Permission to enter the facility, to consult with employees, and to review registers and patient records were requested at the beginning of data collection. Data collectors were accompanied by an official letter from Felegemeles health center.
Result Socio-demographic, Reproductive and clinical characteristics of Respondents from January 2017 to January 2019, there were a total of 1583 deliveries and 465 pregnant women delivered by a cesarean section giving an overall cesarean section rate of 29%. The proportion of cesarean section delivery was higher among Addis ketema sub-city residents, which was 65.2 %. A majority of cesarean section deliveries (71.4%) were in the age between 19 and 29 years of age. The mean age of pregnant women who undergo cesarean section delivery was 29.5 years (+2.2) (Table 1).
| S.no | variable | Frequency | Percent | |
|---|---|---|---|---|
| 1 | Age | <18 | 6 | 1.3 |
| 19 – 29 | 353 | 75.9 | ||
| 30 -39 | 103 | 22.2 | ||
| >40 | 4 | 0.9 | ||
| 2 | Residency | Within sub-city | 300 | 64.5 |
| Out of sub-city | 92 | 19.8 | ||
| Out of Addis Ababa | 73 | 15.7 | ||
| 3 | Gravidity | Primi | 268 | 57.6 |
| Multi gravid | 182 | 39.1 | ||
| Grand multi | 15 | 3.2 | ||
| 4 | ANC status | UnBooked | 65 | 14.0 |
| Booked | 400 | 86.0 | ||
| 5 | Type of surgery | Emergency | 365 | 78.5 |
| Elective | 100 | 21.5 | ||
| 6 | Type of Anesthesia | Spinal | 433 | 93.1 |
| General | 32 | 6.9 | ||
Table 1: Reproductive history of mothers who underwent cesarean section from January 2017 to January 2019 Felegemeles Health center Addis Ababa, Ethiopia, 2014.
Two hundred eight two out of four hundred sixty-five (40.1%) of the study subjects were in their first pregnancy (60.6 %) followed by Multi gravid (37.8%) and grand multi gravid (1.5%). Among the study subjects, one hundred forty-four (91.3%) mothers had antenatal care services registered or were booked. while Seventy- seven (16.6%) of mothers were had a primary previous cesarean section. Among the total mothers who underwent cesarean section, the majority (79.8%) of these women had an emergency procedure. More than half (96.3%) of cesarean sections were made by spinal anesthesia and the remaining were general anesthesia.
Rate and Neonatal Outcomes of Cesarean Section
Among 1583 deliveries in the two years of retrospective data from January 2017 to January 2019, a total of 456 mothers were delivered by cesarean section, giving cesarean section rate 29 %. Among the total deliveries (1583), only nine (1.9 %) neonates were died, giving the overall neonatal mortality rate of the hospital as 5.6 per 1000 live births. Birth asphyxia was the major responsible cause of neonatal deaths accounting for 55.5 %. Of the total mothers who conduct cesarean section procedure; the leading indications of admission for cesarean section delivery were cephalo pelvic disproportionation (26.7 %), none reassuring fetal heart rate pattern (18.3%) previous primary scar (16.6%) arrest cervical disorder (12.3 %) antepartum hemorrhage (3.4%).
Fetal outcome
Nearly all fetuses (98.8%) had a positive fetal heartbeat at the time of admission, and the majority (81.9%) of them presented with the vertex. Three-fourths of newborn babies (74.2%) had normal birth weight (2500-4000 gm). Higher than two-thirds of (87.5%) fetuses had normal Apgar scores. Among the total deliveries, 248 (53.3 %) newborns were males. There were 9 (1.9%) neonatal deaths following cesarean section. The causes of neonatal mortality were birth asphyxia and meconium aspiration syndrome 5, 4 respectively (Figure 1 and 2).
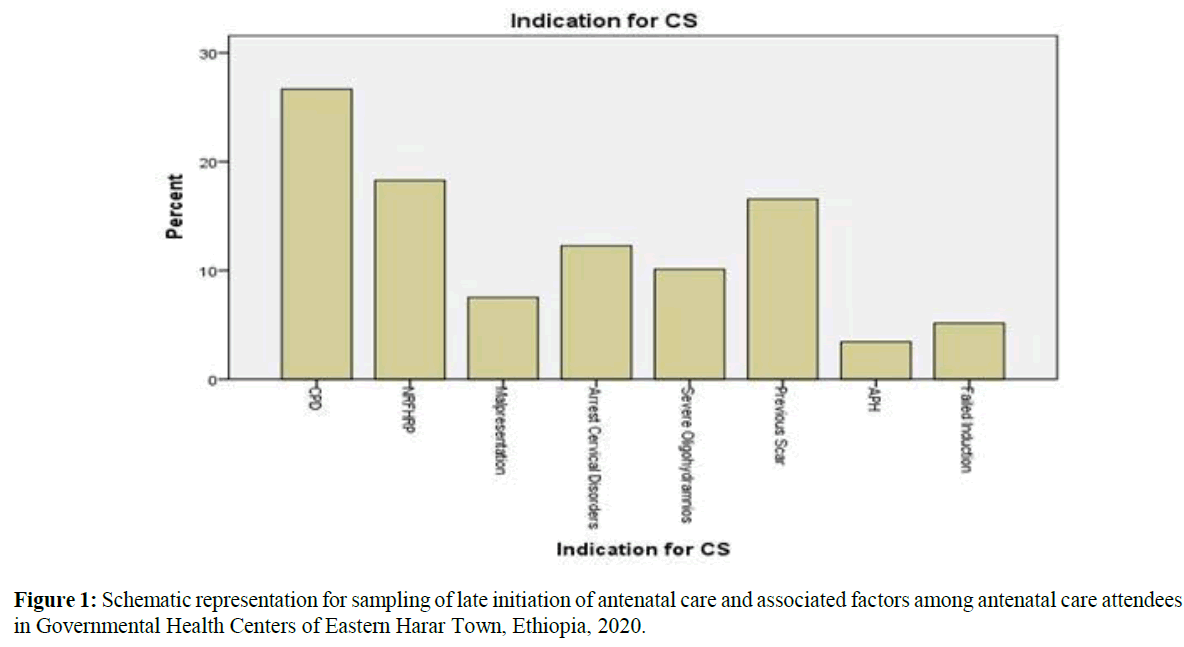
Figure 1. Schematic representation for sampling of late initiation of antenatal care and associated factors among antenatal care attendees in Governmental Health Centers of Eastern Harar Town, Ethiopia, 2020.
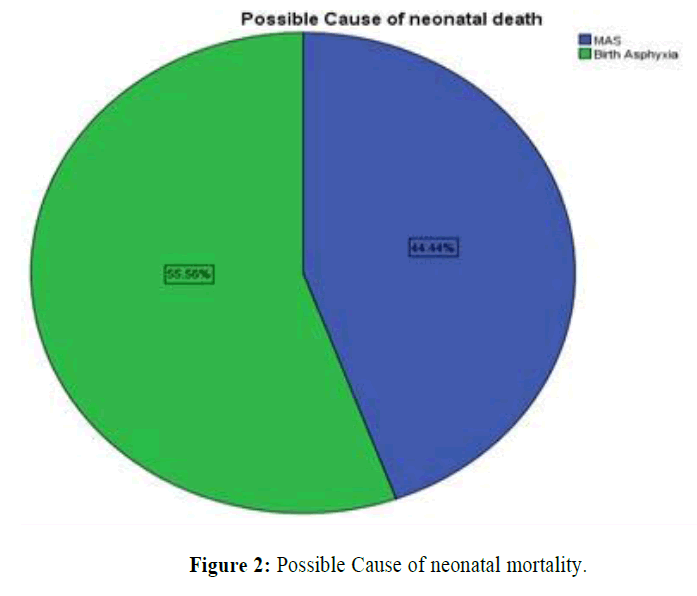
Figure 2. Possible Cause of neonatal mortality.
Determinant factors of CS
The multivariable logistic regression analysis result showed that mothers who were in the age group between 19-29 have 4.7 times more likely to have bad fetal outcomes as compared to the age range less than eighteen (AOR=3.1, 95% CI: 1.44, 14.48). Mothers who are in the sub-city were 2.1 times more likely to have neonatal death after cesarean delivery compared to those residing out of sub-city and out of Addis Ababa (AOR=2.3, 95% CI: 1.47, 6.85). Mothers who underwent cesarean section with Spinal anesthesia were 2.7 times more likely to have neonatal death as compared to general anesthesia ( AOR=3.7, 95% CI: 6.11, 29.95) (Table 2).
| s.no | Variable | AOR(95%CI) | P- Value |
|---|---|---|---|
| 1 | Age | ||
| 19 – 29 | 3.1 | 0.027 | |
| 30 -39 | 6.4 | 0.996 | |
| >40 | 2.4 | 0.67 | |
| 2 | Residency | ||
| Within sub-city | 2.1 | 0.046 | |
| Out of sub-city | 1.33 | 0.322 | |
| Out of Addis | 4.1 | 0.123 | |
| 3 | Type of anesthesia | ||
| Spinal anesthesia | 3.7 | 0.001 | |
| General anesthesia | 4.7 | 0.76 | |
| 4 | Type of procedure | ||
| Emergency | 4.6 | 0.109 | |
| Elective | 3.5 | 0.23 | |
| 5 | Birth weight | ||
| <2500 | 0.077 | 0.077 | |
| 2500 - 4000 | 0.605 | 0.48 | |
Table 2: The other variables like procedure type and fetal weight were not found to have an association with Neonatal death.
Despite Caesarean section being an essential component of comprehensive obstetric and newborn care for reducing maternal and neonatal mortality, there is a lack of data regarding Caesarean section rates, its indications, and outcomes at CEmONC health center level Addis Ababa, Ethiopia. Studies showed negative or no complications of Caesarean on neonatal mortality in low and middle-income countries where the Caesarean rates are high.
From January 2017 to January 2019, there were a total of 1583 deliveries and 465 pregnant women delivered by a cesarean section giving an overall cesarean section rate of 29%. WHO Recommended cesarean section rates be within the range of 5-15% and interpreted as should not exceed 15% because has no additional benefit for the newborns or the mothers. On the other hand, a rate of less than 5% would reflect the difficulty in surgical access [18-20].
This report is comparable to a study done in Nairobi Public Hospitals 29%, Ethiopia, Bahirdar City public health facilities 27.5% and a systematic review done in Ethiopia which accounts for 29.55%. Our study result shows the prevalence of cesarean section is higher when compared to that of Rwanda which is 21.05%. The study result shows a lower overall prevalence of cesarean section as compared to that of private health facilities in Bahirdar which is 56.3%. This discrepancy might be due to 35% of clients being out of catchment sub-city and from nearby Oromia region who are secondary referred from hospitals due to lack of bed for induction and direct elective cesarean deliveries.
The mean age of the 1583 mothers who delivered during the study period was 29±2.20 years. The mean age at first birth among the women who delivered through a cesarean section in this study was 29 years. This finding is comparable to a previous study in Ghana that found the mean age for nulliparous to be 27.3 years but higher than the median age at first birth in Ghana which is 21.4 years. Again this study result is higher when compared to the study done in Jimma Shanen Gibe Hospital accounting 27.8 Years. This could indicate that nulliparous tend to undergo more cesarean section probably due to more difficult labors [19].
Residence, in the majority of studies and specifically study done in at Negest Elene Mohammed memorial general hospital in Hosanna Town, southwest of Ethiopia rural residence associated with adverse neonatal outcomes which are different from our study findings which shows adverse neonatal outcomes associated with in Sub-city then followed out of sub-city and out of Addis. This is might be also due to delay in seeking service behavior in the catchment and out of the catchment area for that matter laboring mothers present late as the service is nearest to them needs further studies before justifications [20].
Our study shows the leading indications of admission for cesarean section delivery were cephalo pelvic disproportionation and non- reassuring fetal heart rate pattern which is consistence with a study done in Cameroon, Dessie, and Meta-analysis done in Ethiopia shows Cephalopelvic disproportion was the most common indication of Caesarean section followed by non-reassuring fetal heart rate pattern. The study is different from the study done in Jimma shenen Gibe hospital which is none reassuring followed by the previous scar. This might be due to correctly identifying and making a decision by a health professional [17,21].
The finding in this study is inconsistent with the Study done in Egypt 2019 & 2021 sections case-control studies [citation], and another study shows that Spinal Anesthesia is safest; associated with good maternal and Neonatal outcomes [22,23].
Systematic reviews and Meta-analysis done by Iranians in 2021 shows that spinal anesthesia is associated with good maternal and neonatal outcomes [24]. The difference is might be due to spinal hypotension in case of fetal distress, compromise of the feto-maternal circulation, and emergency case handling practice for referral in mothers with deep non-reassuring fetal heart rate pattern study before [25-28].
Zero maternal mortality in our study shows CEMONC at health center task sharing has its impacts on the reduction of maternal mortality which needs further studies at remaining facilities but the cesarean delivery rate in this study found was 29.9 % and higher as compared to WHO recommended range, which shows secondary referrals needs attention while Age 19-29, Residency and Spinal Anesthesia have an association with adverse neonatal outcome following cesarean delivery. The neonatal mortality following cesarean delivery was 5.6 per 1000 live births which may to attribute T birth asphyxia. As Access for Obstetric care intervention has shown no maternal mortalities we consider Neonatal Care ICU Needs to be considered for improvements of neonatal mortalities. Maternal delay for seeking care needs to be improved in communication with health extension care workers and ANC care providers while Skills of anesthesia care providers, management of hypotension at time of spinal anesthesia provision needs improvement.
There is no conflict of interest.
There is no financial support.
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Citation: Fitsum N (2022) Outcomes of Cesarean Deliveries and Determining Factors, at Felegemeles Health Center, Addis Ababa, Ethiopia: Retrospective Study Design. J Women's Health Care 11(1):576.
Received: 21-Jan-2022, Manuscript No. JWH-22-15572; Editor assigned: 24-Jan-2022, Pre QC No. JWH-22-15572(PQ); Reviewed: 17-Feb-2022, QC No. JWH-22-15572; Revised: 15-Mar-2022, Manuscript No. JWH-22-15572(R); Published: 12-Apr-2022 , DOI: 10.35248/2167-0420.22.11.576
Copyright: © 2022 Fitsum N, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.