Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2022)Volume 7, Issue 6
A 10-year-old girl presented to the emergency department with acute pain abdomen. Imaging revealed bilateral polycystic ovaries, bulky right ovary with hyper dense walls, and post-contrast enhancement suggestive of right ovarian torsion with infarction. Endocrine consultation was asked for, to rule out endocrine causes of short stature with ovarian enlargement. Suspecting primary hypothyroidism, related blood samples were collected and TSH turned out to be as high as >150 uIU/ml. The child was given Inj. Hydrocortisone 50 mg to prevent lazy adrenal syndrome along with Tab. Levo-thyroxine 100 mcg and was taken up for Emergency right salpingo-oophorectomy. In this case report, we review about the rare complication, ovarian torsion with infarction in untreated primary hypothyroidism, and elaborate on mechanisms responsible for this phenomenon.
Polycystic ovaries; Ovarian torsion; Primary hypothyroidism
Primary Hypothyroidism in children can be congenital/ Acquired, The prevalence of hypothyroidism in children ranges from 2.5-4%. Hypothyroidism in children could be due to dysgenesis (75%), dyshormonogenesis (20%), and thyroiditis (5%) [1]. In India, autoimmune thyroiditis is the most common cause of acquired hypothyroidism.
Thyroid hormone deficiency can affect the growth and development of a child. Cognitive impairment occurs if hypothyroidism occurs in the first 2 years of life [2]. After 2 years of age it’s mainly the somatic growth and pubertal timing that are affected [3-7].
Primary Hypothyroidism can cause precocious puberty, and ovarian enlargement with delayed bone age called as Van Wyck Grumbach Syndrome [8,9]. Previous case reports have demonstrated bilateral ovarian enlargement which was resolved with levothyroxine replacement.
However, we describe a case of 10-year-old girl with a delayed diagnosis of primary hypothyroidism which resulted in ovarian torsion with infarction and loss of ovary. Our case report throws light on the pathophysiology of ovarian hyperstimulation (Figure 1).

Figure 1: 9 year old girl looking like a 4 year old girl.
A 10-year-old girl was brought to the emergency department with acute pain abdomen. The evaluation was limited due to bowel gas with USG abdomen hence CECT Abdomen was done. CECT Abdomen showed a right ovary of 4.6 × 3.2 ×2.9 cm (Volume of 23 CC), Bulky and walls appear hyperdense with subtle post-contrast enhancement suggestive of right ovarian torsion with infarction. The left ovary was 3.3 × 2.5 ×2.1 cm (Vol 9 CC), both ovaries were polycystic. A consultation was given to me to sort out endocrine causes of short stature with ovarian enlargement. On reviewing her past medical records child has arrested growth and constipation for the past 5 years. At the time of presentation, her vitals were (Temp: 36.5 F, PR: 69/min, BP: 110/80 mm of Hg) which were not corresponding to her suffering (Figure 2).
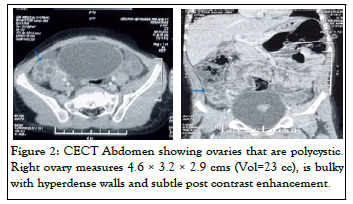
Figure 2: CECT Abdomen showing ovaries that are polycystic. Right ovary measures 4.6 × 3.2 × 2.9 cms (Vol=23 cc), is bulky with hyperdense walls and subtle post contrast enhancement. General examination-Ht: 102 cm, Wt: 15 kg, Primary dentition
General examination-Ht: 102 cm, Wt: 15 kg, Primary dentition still preserved, No goitre, Sexual Maturity Rating–No Axillary and Pubic hair, Breast-B2 (Tanners), the skin was dry.
Systemic examination
P/A: Abdomen was distended, diffuse tenderness present over the abdomen, No palpable masses.
CNS: Deep tendon reflexes showed a delayed relaxation phase and other systemic examinations were normal.
Suspecting primary hypothyroidism, related blood samples were collected and the TSH turned out to be as high as>150 uIU/ml. The child was given Inj. Hydrocortisone 50 mg to prevent lazy adrenal syndrome along with Tab. Levo-thyroxine 100 mcg and was taken up for Emergency right salpingo-oophorectomy.
Investigations
Hemoglobin was 10 g/dl with microcytic hypochromic anemia, liver and renal function tests were normal, Serum cholesterol was 210 mg/dl, LDL-C 180 mg/dl, HDL-C 35 mg/dl, and triglyceride 200 mg/dl. Hormonal profile revealed T3–44.4 ng/dl (N 90–240), T4–2.6 ug/dl (N 5.5–12.8), TSH- >150 uIU/ml (N 0.7–6.4), Anti Tpo antibodies 850 IU/ml (N<8). Prolactin–19.3 ng/ml (N 4.7–23.3), LH–0.32 mIU/ml, FSH– 2.26 mIU/ml, Oestradiol–37.36 pg/ml and Sr. Cortisol–206 nmol/l (N 171–536). Her bone age was 2 years.
With this clinical and biochemical profile, she was diagnosed as a case of long-standing, untreated juvenile primary hypothyroidism of autoimmune origin (Hashimoto’s thyroiditis) with multicystic ovaries, right ovarian torsion with ovarian infarction with arrested growth. She was started on L–thyroxine at a dose of 25 mcg/day with a weekly increase of 12.5 mcg till a dose of 75 mcg. Repeat USG Abdomen after 2 months of initiation of L Thyroxine showed normal left ovary. After 2 months her T3, T4, and TSH were normalized. (T3-1.68 ng/ml, T4-12.96 ug/dl , TSH-1.88 uIU/ml) (Figure 3).
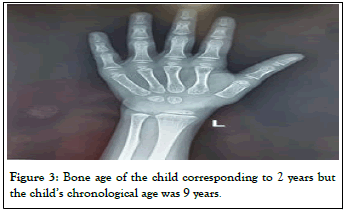
Figure 3: Bone age of the child corresponding to 2 years but the child’s chronological age was 9 years.
Hypothyroidism is not commonly considered as an acute surgical emergency or life-threatening condition. We report a case of acute ovarian torsion evolving into ovarian infarction warranting oophorectomy which is a straight effect of hypothyroidism that was not diagnosed. Many case reports were published earlier describing an array of features including precocious puberty, large bilateral multicystic ovaries, and premature menarche in the background of severe hypothyroidism [10-12]. Nevertheless the catastrophic complication of ovarian loss as in our case is rare. Ovarian removal was executed in a number of cases with ovarian hypertrophy without ovarian torsion. Nearly all oophorectomies can be refrained if the diagnosis was contemplated as hypothyroidism. In cases where bilateral ovarian enlargement prevails, Hypothyroidism must be ruled out as ovaries get back to normal with levothyroxine treatment.
The presence of multicystic ovaries in our patient can be explained by increased FSH secretion which is TRH mediated and diminished FSH clearance, which results in increased FSH and sequential follicular cyst formation. Aditionally high circulating levels of TSH also act on FSH receptors on ovarian follicles due to specificity-spillover, resulting in follicular growth and development. There is homology between glycoprotein hormones and their receptors. Both TSH and FSH receptors belong to the glycoprotein family. Normal levels of TSH when bound to the FSH receptor produce minimal biologic effect. However high concentrations of TSH found in hypothyroidism are sufficient to cause oestrogen secretion, which leads to ovarian stimulation and follicle formation [13-15].
Our patient’s Chronological age was 9 years but the bone age was delayed by 7 years. From this we can understand that hypothyroidism was not suspected early in our patient. This could be prevented by annual growth charting. The usual pattern of hypothyroidism on growth charting would be a plateau in height gain with either unaffected weight or relative weight gain. Distinctly, a late diagnosis of hypothyroidism was the cause of ovarian infarction together with unfavorable final height outcome (Figure 4).
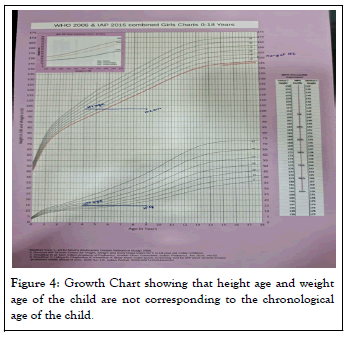
Figure 4: Growth Chart showing that height age and weight age of the child are not corresponding to the chronological age of the child.
Undetected primary hypothyroidism can lead to acute ovarian torsion in children. In any child with ovarian enlargement in addition to growth failure or delayed bone age, primary hypothyroidism should be suspected. Hypothyroidism can be an acute surgical emergency, surveillance prevents this calamitous presentation of a common childhood condition.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Kavya J, Pranav J (2022) Ovarian Torsion: Acute Surgical Emergency in Primary Hypothyroidism. Clin Pediatr. 7:221.
Received: 01-Nov-2022, Manuscript No. CPOA-22-18724; Editor assigned: 03-Nov-2022, Pre QC No. CPOA-22-18724 (PQ); Reviewed: 17-Nov-2022, QC No. CPOA-22-18724; Revised: 23-Nov-2022, Manuscript No. CPOA-22-18724 (R); Published: 30-Nov-2022 , DOI: 10.35248/2572-0775.22.7.221
Copyright: © 2022 Kavya J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.