Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2015) Volume 5, Issue 5
Aim: Analysis of the timelines in the diagnosis and management of surgically treated ovarian torsion will provide novel information on significant time intervals that may be amenable to future improvement which will optimize ovarian salvage rates.
Methods: A retrospective review was performed of all patients who had surgically confirmed adnexal torsion over 12 years. The following four times were extracted for each patient (1) Emergency Department (ED) Triage (2) ED physician assessment (3) Generation of ultrasound report (4) Operating room (OR) start time. Overall time from ED triage to surgery and ovarian salvage rates were also documented.
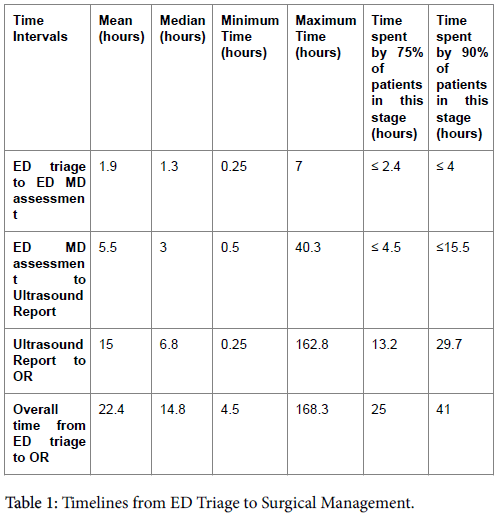
Results: Of 86 surgically proven ovarian torsion cases, 63 (73%) had documentation of all timelines and were included in the study. The overall median time from ED triage to surgery was 14.8 hours. Individual median times were as follows: from ED triage to ED physician assessment 1.3 hours; ED physician assessment to ultrasound imaging report provision 3 hours and imaging report provision to surgical intervention 6.8 hours. Overall ovarian salvage with detorsion occurred in 34 (54%) of cases. Lengthier time delays to surgery were associated with lower ovarian salvage rates.
Conclusion: This study is the first to quantify the time contribution of four major steps in a patient's journey from ED triage to surgical intervention thus providing an opportunity to identify potential targets for quality improvements and serve as a baseline for measuring future improvements. The study confirms that lengthier time delays to surgery are associated with lower ovarian salvage rates.
ED: Emergency department; OR: Operating Room.
Torsion of the ovary is a rare but important gynecological emergency. The incidence may vary from 3% in a series of acute gynecological complaints [1] to as high as 14.8% of surgically treated adnexal tumors [2]. Adnexal torsion can occur in patients of any age, but is most commonly found in women of reproductive age. The true incidence is unknown as the diagnosis can only be made definitively at surgery. Adnexal torsion, involving both the ovary and fallopian tube is the most common situation although isolated ovarian torsion or less commonly isolated fallopian tube torsion may occur. Adnexal torsion, with the accompanying twist on its pedicle, may result in vascular compromise and eventual necrosis of the adnexal structures with consequent negative impact on fertility and potential premature menopause [3]. The clinical presentation of ovarian torsion is often non-specific, thus ultrasound imaging is widely utilized to make a pre-operative diagnosis [4-6]. Although there is a large body of literature describing clinical presentation, imaging features and treatment options for ovarian torsion, there is limited information on which steps are responsible for potential delay of surgical treatment. We were only able to identify one paper that referred more directly to the impact of timelines on ovarian salvage [7], however the correlation was related to accuracy of diagnosis rather than ovarian salvage rates.
Ovarian torsion is considered a surgical emergency. Conservative treatment includes untwisting the adnexa and confirming viable adnexal tissue, although recent literature suggests that detorsion, in particular in the paediatric population, is associated with good outcome for ovarian salvage even when the ovary appears purple or dark black [8-10]. Rather than gross appearance or color of the ovary some studies have suggested that time from onset of pain to surgical intervention may provide a good proxy marker for necrosis. In a retrospective study of 70 patients by Chen et al., they suggested that the likelihood of ovarian salvage is decreased after 48 hours of symptoms [11], otherwise, there are no published studies directly addressing the issue of what is an acceptable timeline from the point of initial suspected diagnosis in the ED to surgical intervention.
The aim of this paper is to analyze the overall length of time spent from initial ED Triage until surgical intervention and correlate these times with ovarian salvage rates. The following four times were extracted for each patient [1] ED triage [2] ED MD assessment [3]. Generation of ultrasound report [4] OR start time. We anticipate such a study would highlight the possible delaying step or steps which can aid in directing efforts at optimizing timelines in order to increase ovarian salvage rates. Early diagnosis and timely intervention are important in order to restore blood flow and preserve ovarian function and future fertility [10,12].
Research Ethics Board approval for a retrospective chart review was obtained from two affiliated urban academic hospitals in Toronto, Ontario, Canada; Sunnybrook Health Sciences Centre and Women’s College Hospital. All patients with surgically proven adnexal torsion between October 2000 and February 2012 across the two affiliated hospitals in Toronto, Canada were identified. We excluded patients who were less than 15 years of age, those who had no imaging provided at either of the two centres, and those who were directly admitted to the Gynecology service.
Demographic and clinical information including age, menstrual status, and gravidity were documented for each patient. Peri-menopausal status was defined as age 48-51 and post-menopausal status was defined as ages 53 and above [13,14].
Data were obtained from several sources: the electronic patient record (EPR) and hospital chart records, emergency department information system (EDIS), and Picture Archiving and Communications System (PACS) and the operative record. From these data sources, the following four times were extracted for each patient [1] ED triage [2] ED physician assessment [3] Generation of ultrasound report [4] OR start time. Overall time was also calculated. Ovarian salvage rates were documented.
Descriptive statistics for each of these waiting times were computed along with their 95% confidence intervals. We also computed the cumulative distributions of waiting times to show the percentage of patients whose waiting times were less than any particular value. We also determined the percentage of patients whose waiting times were less than some predefined targets; e.g. a previous study (4) examined outcomes according to a total wait-time of 10 hours or less, so we computed the percentage of patients meeting this target. We used the Wilcoxon rank sum test to compare waiting times between the following pairs of groups (a) patients with and without salvageable ovaries; (b) patients aged 15-32 and patients aged 32-63; (c) pregnant and non-pregnant premenopasual women. The Kruskal-Wallis test was used to compare waiting times in the three groups formed by menopausal status. All analyses were done using R 3.1 (R Core Team (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/.)
In total, 86 surgically proven adnexal torsion cases were identified and 63 cases fulfilled the inclusion criteria. The mean age was 33.7 ranging between 15-63 years. Most (n=53, 84%) cases were premenopausal, 6 cases (10%) were pregnant at the time of ovarian torsion, and 4 (6%) cases were post-menopausal. About half (52%) were nulliparous at the time of the study. Mean gestational age in the pregnant group was 16.5 weeks (range: 6-36 weeks). All patients underwent a pelvic ultrasound which included a transvaginal component and 20.6% also underwent a CT study of which 69.2% (n=9) were performed prior to the ultrasound evaluation. One patient underwent an MRI study.
The times spent in each stage and also the times for the overall journey from ED triage to the operating room are documented (Table 1). The shortest step was the time from ED triage to the time seen by ED physician and the longest time was spent from generation of an ultrasound report to the patient’s arrival in the operating room (Figure 1).
Overall timelines were compared to the outcomes of adnexal surgery with regards to ovarian salvageability. In 34 cases (54%), the adnexa was considered salvageable at surgery and detorsion was performed. Both mean and median timelines (from ED triage to OR) were significantly longer (p<0.01) in the group with non-salvageable adnexa (Table 2).
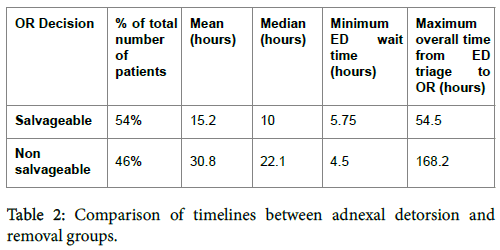
Comparison of recorded timelines with regards to age groups and menstrual state revealed: a significant relationship between a patient’s age and total journey time (p=0.028); a significant difference between median overall times between pregnant (7.25 hours), pre-menopausal (14.5 hours) and peri or post-menopausal (22.5 hours) women (Kruskal Wallis test, p=0.05); a significant difference between median overall times for detorted (10 hours) and removed adnexa/ovaries (22.1 hours) at surgery (Wilcoxon rank sum test p-value=0.0047).
Surgical management was received at the initial admitting site for some patients while others were transferred to the affiliated hospital for surgical management. Timelines for overall journey were compared between these two groups. Median time for initial site treated patients was 14.9 (95% CI 10-22.5) hours and for transferred patients was 14.2 (95% CI 11-28.5) hours with no significant difference noted.
This study is the first to quantify the time contribution of four major steps in a patient’s journey from ED triage to surgical intervention thus providing an opportunity to identify potential targets for quality improvements and serve as a baseline for measuring future improvements. The study confirms that lengthier time delays to surgery are associated with lower ovarian salvage rates.
Time to treatment is an important filter in urgent medical situations. This is typified by literature on other medical emergencies such as trauma systems [15]. In our study we demonstrated that reducing the time from suspected diagnosis to surgical intervention below 10 hours was associated with improved rates of ovarian salvage, as high as 53%. The 10 hour discriminating time point was chosen as it is the only other baseline we could find for comparison in the literature [7]. We were able to identify limited data on comparative rates of ovarian salvage, however Spinelli et al. reported in their pediatric sample of 30 cases they were able to perform conservative detorsion salvage in 14 or 46.7% [16] and Piper et al. demonstrated in their pediatric review that boys were taken to the OR with a median time of 2.3 hours versus girls with a median time to OR of 6.3 hours with a relatively high salvage rate in boys of 30.3% versus girls of 14.4%. This is likely related in part to greater difficulty in pre-operative diagnosis and longer pre-admission symptom durations.
In the group with a salvageable ovary at surgery, the mean and median times for overall journey were significantly shorter when compared to the non-salvageable group (p<0.02). This reemphasizes the importance of avoiding delays in the diagnosis and management of this entity in order to preserve potential ovarian function and fertility.
Adnexal torsion mainly occurs in women of reproductive age [17], 15% during childhood and 15% in the postmenopausal group [18]. Age distribution in our study is overall comparable to these figures. No children were included in our series. A total of 52% of patients were nulliparous at the time of diagnosis compared to 55.6% quoted in the literature [19].
In our study, mean time from admission to operation was 22.4 hours (range of 4.5 – 168.2 hours) compared to 11.4 hours (range of 0.5 - 60 hours) in the study by Bar et al. Their shorter timelines to surgery are likely related to a younger population with a greater percentage of pregnant and infertility patients, and patients with pre-admission imaging
at 14.8 hours. Seventy-five % of the groups were treated by 25 hours, with 90% of the group treated surgically by 41 hours. Furthermore, the timelines are significantly shorter in the younger premenopausal population (p<0.05) under the age of 32 years, which we speculate is related to the greater clinical importance placed on ovarian salvage and preservation of fertility in this age group. The shortest timelines of 7.25 hours were in the pregnant group [20]. We speculate that this is related to the combined urgency of a desire to preserve future fertility and minimize the risk of pregnancy loss or preterm labor associated with untreated ovarian torsion [21]. In contrast, the two longest total journey times of more than 65 hours (Figure 2) occurred in 2 postmenopausal women with atypical presentations in whom alternate diagnosis were initially investigated.
The longest time interval was from provision of ultrasound imaging report to the operating room start time (mean time of 15 hours ranging between 0.25 to 162.8 hours, Figure 1), highlighting a need to assess the surgical priority of cases with suspicion of ovarian torsion. The variability in this time may be explained by the many factors that come into play in this time interval including availability of operating rooms, surgeon, patient preference, and consultations with other services. Nonetheless it highlights an important point in the time journey from ED triage to surgical interventional that may be amenable to quality improvement manoeuvres. For example, the simple existence of the documentation of an institutional time interval may open the window to discussion of improved OR access in a timely fashion, particularly when combined with the documentation of improved ovarian salvage rates with shorter time interval to surgical intervention. Twenty-two% (n=14) of patients underwent a second imaging study of which the majority were CT with one MRI performed. We speculate that the performance of a CT scan in 9 patients prior to the ultrasound was likely related to non-specific clinical findings, whereas the CT’s performed post ultrasound evaluation were related to non-specific ultrasound findings.
The mean time from ED triage to visit by the ED physician was 1.9 hours with a median of 1.3 hours (Table 1), reflecting average times for ED triage to ED physician assessments [22]. The mean time from ED physician assessment to provision of ultrasound imaging report was 5.5 hours with a median time of 3 hours. The length of this time interval may be related to factors such as peak hour volume delays or waiting for the arrival of an on-call ultrasound technologist. This timeline interval is supportive of the need for on-site availability of sonographers on a 24/7 basis. Although point-of-care ultrasound within an ED will likely decrease this time interval, it should be noted that even in experienced hands, ovarian torsion can be a challenging sonographic diagnosis.
There are several limitations to this study. The key limitation is the design with a 12 year retrospective study over which many changing factors may have influenced changes in timelines. Factors which may have inadvertently prolonged a particular stage could not always be evaluated. Some of these may include an individual patient preference for delaying surgery, the need for preoperative fasting, operating room availability, time delay waiting for specialty consultations and the routine of a given surgeon. Another limitation is that from the years 2003 to 2010 some patients were transferred from one site to an affiliate site for surgical intervention. Despite the additional steps involved in patient transfer, no significant difference was noted in the timelines between the two groups. It is difficult to determine the reason, but we speculate that this is related to the high clinical indication associated with patient transfer or the greater operating room availability at the affiliate site. A second important limitation is the definition of ovarian salvage as detorted in surgery with “pinking up” (an ovary was considered salvaged if the surgeon detorsed the ovary saw evidence of good circulation and decided it was salvaged or salvageable). We have no long term follow up on these cases. However, the adult laparoscopic detorsion literature suggests detorsed ovaries do well on long term follow up even if they appear visually ischemic at surgery [8,23]. Shalev et al. demonstrated that 92.4% of adult torsion managed by laparoscopic detorsion were normal in follow-up. Wang et al. demonstrated in a pediatric population ovarian recovery after surgical detorsion with normal size and follicular development in 33/35(94.3%) cases treated conservatively [24].
This study of 63 cases remains one of the largest adult series in the literature [25]. This study has demonstrated that ovarian salvage has a clear relationship to shorter time intervals from suspected diagnosis in the ED to surgical intervention. The longest time interval in the diagnosis and management of ovarian torsion at our institution was the step from ultrasound evaluation and report to the operating room. Given the importance of early diagnosis and operative intervention for ovarian salvage, efforts aimed at optimization of this step will likely result in better outcomes at our centre. It should be noted that a short delay of several hours is considered by many authorities not detrimental to the future viability of the ovary [26]. While most radiology departments monitor their “turnaround times” or TAT, this project uniquely integrates radiology time interval information with the patient ED length of stay until operative intervention. We recognize that the timeline outcomes analyzed in this study may not be applicable to other centres or be generalizable; however we believe that individual departments should assess the time to surgery in their own setting and take measures to ensure that unnecessary delays are reduced to a minimum.