International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Mini Review - (2022)Volume 10, Issue 4
Acute pain occurs with tissue damage. Chronic pain is of long duration and involves neuronal plasticity. Pain is objectively measured and treatment models for acute and chronic pain involve an integrated approach with different emphasis. Pain adequately managed improves morbidity and Health Related Quality of Life (HRQoL) and is a driver for cost saving. Pain has wide-ranging impact on the sufferer’s quality of life affecting the following aspects of daily living: sleep, behavior and mood as well as the ability to function fully to participate and enjoy work, family life and social activities.
Acute pain; Chronic pain syndromes; Pain pathways; Pharmacological and non-pharmacological management; Costs of pain
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage [1]. This definition proposed by the International Association of the Study of Pain (IASP) in 1979 and adopted by the World Health Organization (WHO) has subsequently been broadened in 2020 [1] to incorporate “or resembling that associated with’’ actual or potential tissue damage and other unique components with emphasis that pain:
• Remains a personal and unique experience
• It should be defined in simple and practical terms
• Has specific components
• The concept of tissue injury must be in keeping with new ideas of pain
This article will broadly describe the types of pain encountered and will include the fundamental pain pathways involved. In doing so, its management in the peri-operative period will be highlighted. It will further distinguish acute from Chronic Pain (CP) and the pharmacological and non-pharmacological strategies available in the management of common CP syndromes. Concluding remarks relate to the costs of pain in terms in of its economic impact on individuals, the wider economy and the availability of newer management strategies.
Types of pain are broadly defined within 3 categories
Nociceptive pain: This pain is associated with actual tissue injury due to trauma or a surgical insult.
Neuropathic pain: Systemic illnesses causing peripheral nerve damage resulting in pain (diabetes) and other inflammatory conditions that affect nerves (herpes zoster)
Neuroplastic pain: These are chronic pain conditions which involving peripheral and central sensitization (wind up) of receptors to give an altered perception of pain. These can become long lasting (fibromyalgia).
Other categories are inflammatory pain and psychogenic pain.
In general pain is defined by two main pathways. They are:
Ascending: The Spino-thalamic (afferent in red)
Descending: The Corticospinal (inhibitory/efferent in blue) (Figure 1).
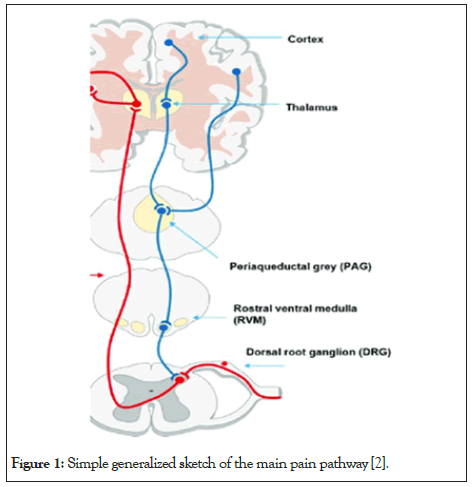
Figure 1: Simple generalized sketch of the main pain pathway [2].
Noxious stimuli stimulate nociceptors in the skin, muscle, bone and organs. These sensory afferent transmission pass via the dorsal horn to supra spinal area in the midbrain, thelamus and the somatic sensory area of the frontal cortex Descending pathways from the frontal cortex and supra spinal areas modulate pain in a downward transmission [2].
Tissue damage causes the release of inflammatory mediators [3]. These include arachidonic acid, histamine, bradykinin, 5-HT, potassium. In the Central Nervous System (CNS) mu, delta and kappa opioid receptors modulate pain. Exogenous opioids act on these to provide analgesia. [3]
Pain assessment is based on history taking and clinical examination. Common validated scales used for its objective measurement is the Numerical Rating Scale (NRS) whereby pain is measured on a scale of 0-10 (Figure 2). Pain is scored as: Zero - Mild- Moderate- Severe Pain [4].
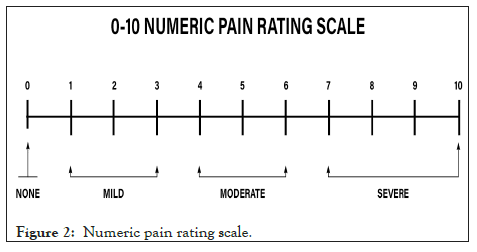
Figure 2: Numeric pain rating scale.
Intra-operative pain management
A multi-model regimen is used that incorporates opioids, non- steroidal anti-inflammatories (NSAIDS) and analgesics such as paracetamol. Target Control Infusions (TCI) with agents such as remifentanil aim at achieving steady state concentrations of the drug in the central compartment based on its pharmacokinetic properties. The depth of analgesia is titrated to the surgical stimulus to give better control of analgesic requirements under anesthesia. The use of opiate free analgesics such as ketamine and dexmedetomidine may be advantageous in patients that are opiate naïve or elderly. There as less untoward side effects such as respiratory depression, nausea/ vomiting and constipation enabling early mobilization and discharge.
Early Release after Surgery (ERAS) is cost saving and avoids added health care burdens.
WHO Analgesic Ladder (1986) for cancer pain [5]. This practical and useful guide served as a framework over many years.
Step 1: Mild Pain-Non-opioid (Paracetamol)
Step 2: Moderate pain-Weak opioid (Tramadol)+Adjuvants (Tricyclic+NSAIDS)
Step 3: Severe Pain-Strong opioid (Morphine)+Adjuvants+Para cetamol.
Recent modification to this guide is proposed which incorporate a multidisciplinary approach for Chronic Non Cancer Pain (CNCP) with less reliance on opioids (Figure 3).
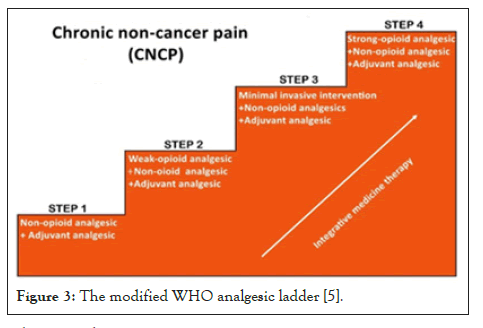
Figure 3: The modified WHO analgesic ladder [5].
Pharmacology
The adequate management of acute pain will prevent its transitioning to chronic pain conditions. In acute pain management the use of multimodal analgesia has the benefit of added analgesia so lowered doses of individual agents are used with fewer side effects [6]. Morphine and synthetic opioids fentanyl/fentanil are potent analgesic agents for severe pain. They are used intravenously, intrathecally and as TCI infusions. They have excellent analgesic properties but cause respiratory depression and have addiction potential.
Tramadol is used in moderate pain it facilitates the inhibitory pathway centrally and acts on the downward transmission to reduce pain by its action on mu receptors. Its abuse potential is not uncommon. Oral and intravenous preparations are used in combination with adjuvants. NSAI and steroids are part of a multi modal therapeutic regimen. These block the inflammatory mediators at the surgical sight in addition to acting centrally along the pain pathway. Cyclo-oxygenase inhibitors (COX 1 and COX 2) have different safety profiles with Cox 2 inhibitors (Celebrex) having fewer systemic side effects on the gastro-intestinal tract, platelet and renal functions. Steroids reduce swelling and have anti-inflammatory effects. Its short-term use avoids the harmful effects of diabetes and adrenal suppression.
Paracetemol Intravenous and oral preparations act peripherally and centrally has a good safety profile. A maximum daily dose of 4 g/24 hours in adults is recommended and 20 mg/kg/24 hours in children. Ketamine is a multipurpose agent can be used intravenously/orally/nasally. It provides analgesia, sedation and dissociation when used and has weak agonist effects at the mu, delta and kappa opiate receptors with a direct effect in modulating pain. It also has opiate sparing effect through its action as an N-Methyl-d-Aspartate (NMDA) receptor antagonist. Combinations of ketamine, lignocaine, magnesium sulphate and dexmedetomidine can be used as a non-opiate analgesic infusion peri operatively to provide analgesia. Local analgesia is infiltration of wounds and regional analgesic techniques add further benefits and improve patient comfort.
Chronic Pain is defined as pain lasting more than 12 weeks. It differs from acute pain in terms of pathology in that there is an altered perception of pain. Hyperalgesia (pain sensations becoming enhanced) and allodynia (a painful response to stimuli previously not painful) occurs. Central sensitization and neural plasticity occur which cause discomfort and pain lasting months or years. Chronic pain is often accompanied by insomnia, mood changes and chronic fatigue. It can lead to anxiety and depression and impact on normal functioning. Chronic pain is measured by a questionnaire like the Brief Pain Inventory (BPI) which incorporates questions related to pain, general activity, mood, walking ability, work, relationships, sleep and enjoyment of life.
Chronic pain illnesses require additional tests to rule out conditions with similar features. Chronic Pain Conditions include Cancer Pain and this may be primary or metastatic disease, Migraine and cluster headaches, Chronic Lower Back Pain (LBP), Long covid and ICU (intensive care) sequelae, Neuralgia is Post Herpes Zoster and Trigeminal neuralgia, Fibromyalgia, Complex Regional Pain Syndrome (CRPS).
Pain interaction with anxiety and depression
Pain which becomes incapacitating and interferes with work, daily activities and life pleasures is a cause of anxiety and mood disorders. Mental health assessment is needed as these disorders expand pain symptoms [7]. Depression and chronic pain are bi- directional with increased risks of suicidal attempts, painkiller misuse and higher tobacco use [8]. A multidisciplinary approach is required in chronic pain management involving life style changes, medical and other non-pharmacological therapies.
Pharmacological therapies in chronic pain conditions
The use of strong opioids for CNCP is widespread in wealthy countries despite its uncertainties with regard to efficacy and safety. Its short-term use may reduce pain in chronic lower back pain (CLBP) but with no effect on disability but its long-term use (>6 months) in CNCP may not be superior to nonopioids in improving pain or disability. It may cause adverse effects in terms of abuse, dependence and possible increase in mortality [9].
Opioids should be reserved for severe cancer pain. Morphine orally can be titrated to comfort with non-narcotic medication. Maximum dose of morphine should seldom exceed 50 mg, and needs supervision in order to reduce opiate side effects, overuse and addiction. Buprenorphine is useful in patients requiring a high daily dose of morphine and still having inadequate analgesia [7]. NSAI, paracetamol and muscle relaxants can be combined with therapies that include treatment for anxiety, mood disorders and depression.
Anti-depressants are beneficial and significantly reduce pain in chronic pain in conditions when required [7]. Duloxetine a Serotonin Noradrenaline Reuptake Inhibitor (SNRI) is useful for LBP, fibromyalgia, neuropathic pain in addition to major depression and generalized anxiety disorder. Tricyclics anti- depressant (amitriptyline) has secondary analgesic effects. Duloxetine used in fibromyalgia improved mood disorders and was found to be safer in the elderly while amitriptyline had low evidence for pain, moderately improved sleep and good evidence for improving QoL [10].
Gabapantinoids (gabelin and pregabalin) are calcium channel alpha-2 delta ligands useful in neuropathic conditions including post herpetic neuralgia and has opioid sparing effects [7]. Carbamazipine a antiepileptic is useful in trigeminal neuralgia [7]. Triptans are serotonin receptor agonist are used for migraine and cluster headaches. Ketamine analgesic effects are effective in intermittent migraine attacks and botulinum toxin injected in the muscle area of the pain effectively release muscle spasm and relieves pain.
Neuromodulation devices (external trigeminal nerve stimulator) have also been approved by the United States Food and Drug Administration (FDA) for the acute and preventive management of migraine [11]. The use of monoclonal antibodies and rimegepant a calcitonin gene-related peptide (CGRP) is now approved for both acute and the preventive management of migraine by the FDA [11]. Interventional therapy can be used diagnostically or therapeutically, and these surgical and neuro- surgical ablation techniques provide relief for fibromyalgia and trigeminal neuralgic pain. Common techniques are epidural steroid injections (LBP), trigger point injections for fibromyalgia and intrathecal pain pumps for chronic LBP [7]. Radiotherapy has proven benefit for pain relief in sufferers with primary and metastatic bone disease.
Non-Pharmocological Therapeutic strategies (NPT)
These complement pharmacological therapies in treating of chronic pain conditions. They include heat and cold therapy, relaxation therapy, exercise and other modalities. Chronic pain management with a strong reliance on opioids has resulted in unintended consequences. The abuse potential of opiates, its aftermath in terms of self-harm, suicidal ideation and addiction has prompted a rethink and an integrated approach incorporated to its medical management. The study of military veterans from Iraq and Afghanistan with chronic pain given NPT like exercise, chiropractor manipulation and massage therapy had less morbidity. They were in addition shown movement techniques like yoga. These subjects had fewer drug and alcohol abuse problems and the tendency to self-harm [12]. LBP is a common disability worldwide for which yoga is a common complementary therapy. It involves breathing techniques, movement, postures and meditation. A systemic review and meta-analysis comparing yoga with non-exercise control and an active comparator (exercise controls) showed robust short term and long-term effects for pain, disability and physical function than in non-exercise controls. Serious side effects were rare but may be associated with extreme practices [13]. Walking as part of an exercise routine is cost effective and beneficial in managing LBP. Pain, disability and fear-avoidance improve with exercise [14].
Lifestyle changes: Healthy eating habits and diets combined with movement and exercise will promote a sense of wellbeing and a positive mind set. The encouragement to develop regular sleep patterns and adopt relaxation techniques such as mindfulness and meditation promote wellness and better pain tolerance. The Impact of social isolation with limited access to movement is harmful and pain can be perceived to be worse. The covid lockdown is a case in point when access to chronic illnesses was severely impacted. Mental health and sleep disturbances were reported [15,16] and other chronic disease impacted including diabetes and hypertension with poorer outcomes.
Cognitive Behavior Therapy (CBT): This modality can be used to manage emotions and de-escalate pain cycles as well as unfounded anxieties that may cause depression. Preventing the catastrophizing of events and slowing down may provide grounding and a proper perspective of life events.
Physical therapy: Maintaining and improving muscle strength and joint flexibility will aid the ability to function and carry out tasks. This will have a positive impact on body image and improve mental strength.
Occupational therapists play a role in creating a friendlier work and home environment so functionally can be improved. Hobbies, sporting interests and movement activities release feel good endorphins. Interaction with friends and community are further aids to happiness and HRQoL [17-20].
The management of acute and chronic pain embraces both pharmacological and non-pharmacological strategies. Best practice guidelines recommend a stepwise approach using multiple strategies depending on the severity and extent of the pain. The cost of pain in terms of direct health care costs and loss of productivity is enormous and may exceed that of other chronic illnesses such as cancer treatment and heart disease. Multimodal programs utilized in cost effective ways within primary health care settings can be a driver to saving costs and improve HRQoL. National data on chronic pain medicine show that most adults in the US prefer a combination of non-drug and non-opioids to control pain, with 55% of adults using non-opioid pain management and 11% both techniques. Complimentary therapies were followed by physical, occupational or rehabilitative therapies with opioid overuse common among older adults. A program to reduce opioid overuse in chronic pain termed Mindfulness Oriented Recovery Enhancement (MORE) showed promising outcomes, with less opioid misuse and improved pain symptoms compared with traditional psychotherapy. The study in a primary setting involved improving self-regulation (Mindfulness), decreasing negative emotions (Reappraisal) and being appreciative of happy experiences (Savoring). In developing societies with restricted health budgets and private health care limits newer strategies for chronic pain management and rehabilitation are recommended.
Author: BA B
Collaboration: AB
Layout and assistance: Mohamed Bulbulia (BA, UNISA)
Authors have no conflict of interest.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Bulbulia BA, Bulbulia A (2022) Pain Management: Perioperative Acute Pain and Chronic Pain Syndromes. Int J Phys Med Rehabil.10:633.
Received: 23-Jun-2022, Manuscript No. JPMR-22-18045; Editor assigned: 27-Jun-2022, Pre QC No. JPMR-22-18045 (PQ); Reviewed: 11-Jul-2022, QC No. JPMR-22-18045; Revised: 20-Jul-2022, Manuscript No. JPMR-22-18045 (R); Published: 28-Jul-2022 , DOI: 10.35248/2329-9096-22.10.633
Copyright: ©2022 Bulbulia BA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.