Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2022)Volume 13, Issue 2
We have conducted a small questionnaire among patients struggling with atopic dermatitis (AD). We were interested in their daily living with AD, problems connected with the disease and cooperation with their medical doctors. We have performed the study on polish people population to assess the current treatment effectiveness and control of AD, AD patients’ problems and the most important thing—cooperation with their health care providers. In 2020 one hundred and one patients took part in the study, answering 12 questions via online question sheet. They were selected randomly all over the country. The most interesting result was the cooperation and understanding for both patient and health-giver is crucial and should be regarded as one of the component of treatment.
Atopic; Dermatitis; Treatment; Patient
Atopic Dermatitis (AD) is a common, widespread disease affecting up to 20% children population and 2-10% of adults. The disease affects people of all ethnic groups. The problem is global affecting patient and relatives [1]. There are different manifestations of AD; clinical symptoms of AD manifests from typically localized eczema, through dry and altered skin, pruritus to mental health disturbances like sleep disorder and depression. Etiology and pathophysiology of the disease is complex consists of many different elements: immunologic, skin barrier defect, microbiome dysbiosis and environmental interactions. AD is multifactorial disease [2]. AD can co-exists with different atopic diseases like asthma, atopic allergic rhinitis. Together they are so called atopic diathesis. The common future is local production of IgE which triggers the inflammatory process which is an underlying pathomechanism [3]. Other autoimmune diseases such as vitiligo, celiac disease, inflammatory bowel disease are more frequent in young adults and children with AD but strict pathomechanism is still unclear. There is a positive correlation between upper autoimmune diseases including skin and intestinal mucosa and patients with AD and with systemie lupus erythematous too. [4]. AD also co-exists with non-atopic serious illnesses like cardiovascular. The study from 2015 says adults with atopic diseases are more likely to develop heart attack and stroke. The scientist’s revealed patients with eczema are more at risk to start smoking cigarettes, drink alcohol and live sedentary lifestyle. [5]. Another interesting thing, there is strong association between systemic inflammatory diseases and cardiovascular diseases. The study showed AD may be regarded as an independent risk factor of ischemic stroke and moreover the more severe AD, the higher risk of ischemic stroke [6]. And also science has shown us there is a huge relation between severity of AD and cardiovascular comorbidities in study from 2018, but yet comorbidities in allergic patients are not well characterized [7]. AD is connected with neurologic and psychiatric problems too. Chronic itch developed in AD can caused sleep and psychiatric disturbances including depression, anxiety and speech disorders. All of them should be considered by doctors during treatment. Some studies show there is connection AD with osteoporosis and injuries and fractures too [8]. Another significant problem connected with AD is suicidal ideation. The survey showed symptoms of suicidality in patients with AD were high. It seems that psychiatric diagnosing of AD patients should be involved into regular treatment process, because symptoms like depression, anxiety, lower age and high severity of AD may occur before suicidal behavior and can help to predict suicidality in AD patients [9]. Moreover, AD contributes to economic loss. In one study, found AD causes 76 hours of absence per year, which translates to loss of performance of the business [10]. It shows AD has a huge socioeconomic impact but yet these studies are limited. Another study found in its estimations the extra many spending for treatment necessities of atopic eczema cost was 927€ per patient per year. The costs in AD are much higher than in other chronic diseases. And indicates this cost should be always considered individual with patient [11]. Another example of economic loss is the study published in 2021 about expenses on AD in the UK. Model of healthcare resources used and drug costs of 462.99M € over the 5 years on AD. When considering comorbidity burden the cost increased to 1,2B € and with production loss the cost increased to 7,06B € [12].
People struggling with AD have mental and other non-atopic disturbances and are pushed to seek a help of a psychiatrist. They also lower their self-esteem and become socially withdrawn. This paper provides only patients with AD point of view on their disease, treatment process and cooperation with their medical doctors. Our aim of this article is to enhance underlying problems patients are struggling with, and help to encourage both sites doctor and patients to involve in treatment process. We are going to show AD viewed by patients in Poland 2020/2021 step by step
Etiology
Etiology of AD is complex and multifactorial. It consists of disturbances in skin barrier, immunology disorders and skin microbiome disorders, environmental and personal factors. Skin barrier defect allows allergens penetrate through epidermis and it can cause allergy development [13]. It also restores inflammation, immunology disorders base on Th2 (T-helper cells) axis pathway that cause activation of inflammation. Other cells like Th17, Th22 and Th1 cytokines are also contributing to develop AD in cooperation with patient age and ethnic background [14]. Dysbiosis within the skin layer in AD patients and little microbiome variety is a next well known factor of AD. Studies proved Staphylococcus aureus domination is connected with AD degree of severity [15]. Normal skin without lesions is colonized by commensal bacteria and it maintains the skin defenses and produce antimicrobial peptides. Lack of these peptides favors Staphylococcus aureus colonization and contributes to AD development [16]. The disease is heterogenic and is a challenge to the treatment. Knowing patients unmet need is facilitating the treatment process. It also improves the compliance and adherence. Finally improves the effectiveness of the treatment.
The study was conducted in Poland on April to September 2020. One hundred and one patients (>16 years) and caregivers of children with all forms of AD randomly selected all over the country responded online to our 12-question sheet. In total 80.2% female and 19.8% male took part in questionnaire. The questionnaire composed of 12 single and multiple questions for patients and caregivers of children aged 5 to 16 years. The whole study took a year of collecting and analysing data. We proposed an online form for our questionnaire. Thanks to this, we obtained a cross-section of responses from people from all over the country. And this made it possible to avoid the influence of single factors such as place of residence or exposure to factors only in a specific area. As a result, we managed to obtain a wide variety of responses. The section below called “results” presents the exact questions together of our questionnaire with a percentage of the answers. Moreover, we illustrated the answers to the questions using graphs that we created ourselves in order to show the percentage distribution of answers. Each graph has been assigned to the corresponding question in the paragraph below and described with the appropriate number. Our questionnaire was addressed to people participating in AD support websites and fanpages mainly via facebook.
We present below the outcome of most important and fascinating questions from our survey. Respondents were asked about time of duration of the disease and average duration time is 8.23 years for 90 answers (11 rejected because of ambiguous answers) with most common answer 21 years of struggling with AD. The majority 78% started to be sick in the childhood. We can say that out of 101 people who took part in our questionnaire 81 people were woman, and this was the majority -82%. It may be due to the greater frankness of female than male, rather than predilection of AD to female gender. We focused our questions on the treatment process and burdensome factors of AD. Our Survey unveiled that the treatment process was conducted (53.8% only topical, 40.8% topical and systemic and 4.4% only systemic) (Figure 1). This graph pertains to treatment by drugs only excluding emollients usage.
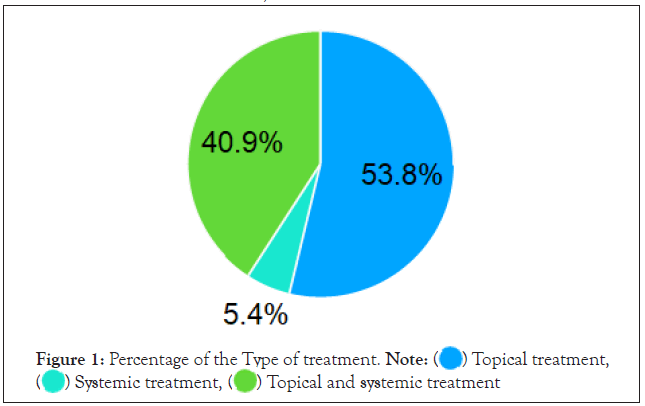
Figure 1: Percentage of the Type of treatment. 
Another aspect that we asked about was the feeling. Majority picked pain and itch of the skin 57.4%, only pruritus 37,6%, only pain 3% and none of possible options 2% (Figure 2). It shows that Polish population struggle mostly with both pain and itch feeling. The most burdensome factor turned out to be pruritus, picked 87 times (Figure 3). Other symptoms that were possible to pick were dry skin, image of lesionaly changed skin, skin pain, the extent of lesions, sleep disorders and lichenification of the skin ( from the most frequently to the least frequently selected). Pruritus as the most frequent symptom picked by respondents has various origin and components. It consists of metal component, somatic component and can by caused by external factors. We focused on this most frequent symptom and then we asked about it in more detail.
Figure 2: Most feel symptoms. 
Figure 3: Frequency of burdensome symptoms in AD. 
One of most important question for this manuscript was confirmation or negation the thing that medical doctor asked about most burden factor of the disease for the patient (Figure 4). Following by the answers 70.3% respondents picked negation and only 29.7% confirmed.
Figure 4: Focusness on the burdensome factor. 
We used numeric scale with following interpretation 0-10, which 0 - disappointed, 5 - neutral, 10 - very satisfied, as the most common and easy in explanation scale (Figure 5). The outcome of the question was a little surprising. 52.5% people picked numbers below 5, including 4% which chose 0%, as well as number 10 was picked by 4% people and number 5 chose only 14.9% respondents.
Figure 5: Treatment satisfaction - numeric scale.  satisfaction-numeric scale 0-10
satisfaction-numeric scale 0-10
The last question we asked our respondents concerned side effects that are more burden that the therapeutic process itself including drug side effects. 68.3% respondents choose “no” and 31.7% picked “yes” (Figure 6). Yet, it is another amazing outcome showing that almost 1/3 of patients feel worse because of treatment process.
Figure 6: Intensification of adverse effects of treatment. 

Atopic Dermatitis as a multifactorial disease affects many aspects of patients’ life and is followed by other disorders. This compound disease which is global worldwide, can affect the youngest and the oldest. This shows our pediatricians and geriatricians must be involved in therapeutic process of AD because of its prevalence among the population. Prevalence of AD is the highest among children population and because of chronic and visible skin lesions may cause stigmatization and selfesteem problems. But it is still understudied. Problems concern about exhaustion, emotional distress and parents depression. All together leads into vicious circle. Available studies showed stigmatization and self-esteem problems are not crucial among children with AD. Yet, there are a few that need to be pointed out and taken care of them [17]. Greater prevalence among higher educated people may arise from more distress factors and faster pace of life. Moreover, the questionnaire indicated persistent itch as the most burden factor accompanying the disease. Pruritus is another factor that effect on the Quality of Life (QoL) AD patients. Data about QoL and treatment process are rare. In our study 37.6% respondents felt itching and it seems it can be a big problem in everyday life following next citation. In one study scientists have found correlations between pruritus and Pruritus-related Life Quality Index (PLQI). That correlates with psychosocial disturbances and difficulties in everyday life. The outcome of the survey showed chronic itching reduced QoL. There is inverse correlation between severity of the Itch and QoL regardless of cause [18].
Another important study showed the association of AD with pruritus, inflammation of the skin and skin barrier damage can be correlated with skin pain. In the study 42.7% of respondents reported skin pain. From their descriptions the pain seemed to be neuropathic pain. Severe skin pain was correlated with greater AD severity, sleep disturbances, depressive symptoms and low QoL [19].Other study concerning about evaluation importance of symptoms by patients’ perspective unveils
Pain and itch are the most important components in evaluation of treatment process. That study was performed on international group of patients and confirms our results on Polish population. It shows that to evaluate properly treatment process and its effectiveness we have to create questionnaires that include questions about feel of the pain and the itch [20]. In our study we noticed skin pain accompanying to about 60% of respondents. We see it is the most prevalence symptom in AD. And the disease in itself seems to be Associated with increased skin pain. Skin pain affects QoL according to last survey. Pain severity may be promising endpoint of AD treatment and monitoring it. There are necessary future studies about measuring and treating skin pain alone.
Another study focused on evaluation of treatment satisfaction. The survey showed most of parents 56% of AD children was not happy about treatment results. But 40% of them did not follow advices of their health care provider. Study also unveiled the dissatisfied with treatment is associated with worse following of doctor’s advices. Researchers developed important independent factors of dissatisfaction which are lack of psychological support, little knowledge about the disease, dissatisfaction of contact with health care provider and diagnostic process [21].
Comparing to our study we did not asked about treatment satisfaction directly but we distinguished few other factors. First is asking respondent about whether their doctor asked them about most annoying factor in AD. The Outcome of this question is amazing and opening wide field to discussion. We got only 29.7% positive responses. There are many options for that fact from lack of time for each patient to just not having it in mind. Yet it is really hard to the bottom of it. Another factor we wanted to know is asking the patient about how he/ she perceives doctor treating most burden factor and we got 56.4% of respondents who were not happy with it. It may lead to concern about patient’s needs. Because it showed people are not satisfied with it when health care providers skip such questions. It generates dissatisfaction and worsens the whole treatment process. The questionnaire shows we are still lacking in effectiveness of treating AD. We can assume that there is still much to improve in treatment of AD or communication with patient. Hopefully, there is new therapeutics, which is registered like MAB - Dupilumab and JAK Inhibitor-Baricitinib and new monoclonal antibodies and JAK inhibitors are coming. It seems very promising like JAK-STAT inhibitors used in several cases of AD [22] and many more new studies on treatment process of AD and so new drugs.
Nowadays, AD is the disease that medicine treats it but will not completely heal it. We also recommend assess skin pain, pruritus when measuring severity of AD. Another big problem is to find one thing that can evaluate therapeutic process for each patient. Everybody present different manifestation of AD from others and we need to find a universal key that will be both simple and multifactorial which can evaluate that we provide appropriate treatment. This is the next thing we are working on and would have some results in couple of months.
We saw AD occurs at any age as well as 70 years old patient and 5 years old patient. This show how compound and chronic is AD. It may imply other disorders, especially the mental ones, when the disease prolongs. Due to the education AD is seen mostly in high educated people 43 people out of 101, 32 people with secondary education, 3 people with primary education and 23 out of 101 respondents are still studying.
When we asked about the most burden factor of AD, respondents chose persistent itch - 87 people, second most severe factor was dry skin and the third - image of lesionaly change skin. And as the least severe they indicated lichenification. These answers turned our concern to persistent itch, which is very hard and unrewarding in treatment process and persist for long time causing other problems e.g. sleep disorders.
Respondents asked about feeling that accompany to lesions chose pain and itch as most frequent answer - 58 out of 101 people. 38 people indicated only the itch and 3 pains. 2 people did not pick any available answer.
When it comes about doctors concern about patients the most burden problem, 71 people said their doctor did not ask them about it and only 30 respondents confirmed that their doctor asked about what the most annoying problem is.
Then respondents choose how they are satisfied with treatment of AD. We gave them numeric scale 0-10, which 0- disappointed, 5 - neutral, 10 - very satisfied. The outcome of the question was a little surprising. 52.5% people picked numbers below 5, including 4% which chose 0%, as well as number 10 was picked by 4% people and number 5 chose only 14.9% respondents.
The outcome of our last question concerning side effects of treatment that are worse than the disease itself was 69 people, who answered the side effects of treatment are not worse than AD itself, and for only 32 people side effects were worse.
AD is heterogenic, chronic and recurring disease. It needs the strategy and a plan of treatment. The communication between patients and health-care givers is crucial, and should be regarded as one of component of treatment. We need more information campaigns about AD to involve patients into active participation in treatment process. As well as sensitized doctors to problems reported by their patients. This survey showed one of biggest challenge we have to face with is skin pain and itch. Both are among common problems reported by patients and hard to relieve. That is why we must concern it.
Despite the limitations of the study we have information on how many the doctors awareness of patient’s perception of the disease can easily affect the patent’s compliance with the recommendations and increase the effectiveness of the therapy. We take it as an introduction to further research on this topic.
We do not know the severity of the disease in respondents. The disease burden may be different from mild and moderate to severe AD and also we do not have knowledge that has been treating the patients -pediatrician, dermatologist, alergologist? And this is why the group is limited.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
[Crossref] [Google scholar] [Pubmed]
Citation: Szalus K, Trzeciak M. (2022) Patient’s Perspective of Atopic Dermatitis. J Clin Exp Dermatol Res. 13:603.
Received: 03-Mar-2022, Manuscript No. JCEDR-22-16097; Editor assigned: 07-Mar-2022, Pre QC No. JCEDR-22-16097; Reviewed: 21-Mar-2022, QC No. JCEDR-22-16097; Revised: 28-Mar-2022, Manuscript No. JCEDR-22-16097; Published: 04-Apr-2022 , DOI: : 10.35248/2155- 9554.22.13.603
Copyright: © 2022 Szalus K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.