Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2023)Volume 8, Issue 5
Pediatric cancer remains a significant challenge in the field of oncology, with leukemia being one of the most common malignancies in children. This case report explores the diagnosis, treatment and long-term management of a pediatric patient diagnosed with leukemia. Leukemia, specifically Acute Lymphoblastic Leukemia (ALL) is discusse in detail, including its pathophysiology, risk factors, clinical presentation, diagnostic modalities, treatment options and the importance of supportive care. The case of a 7-year-old child diagnosed with ALL is presented to illustrate the clinical course, therapeutic interventions and challenges in managing pediatric leukemia. This case report aims to provide healthcare professionals and researchers with insights into the complexities of pediatric leukemia and the comprehensive approach needed for optimal patient outcomes.
Pediatric leukemia; Acute Lymphoblastic Leukemia (ALL); Childhood cancer; Case report; Pediatric oncology; Chemotherapy; Supportive care
Pediatric cancer is a devastating condition that affects children and their families worldwide. Among various pediatric malignancies, leukemia is one of the most common and poses unique challenges due to its heterogeneity and complexity. Leukemia is characterized by the uncontrolled proliferation of abnormal white blood cells in the bone marrow, leading to a myriad of clinical symptoms and complications. This case report focuses on Acute Lymphoblastic Leukemia is a common subtype of pediatric leukemia and aims to provide an in-depth understanding of its pathophysiology, diagnosis, treatment an long-term management through the presentation of a real-life case [1,2].
Pediatric leukemia
Leukemia is a hematological malignancy that primarily affects the bone marrow and blood. It can be broadly categorized into acute and chronic forms, with acute leukemia being more common in pediatric patients. Acute leukemia is further divide into ALL and Acute Myeloid Leukemia (AML), with ALL being the most prevalent subtype in children. Pediatric leukemia accounts for approximately one-third of all childhood cancers and is a leading cause of cancer-related mortality in this age group (Figure 1).
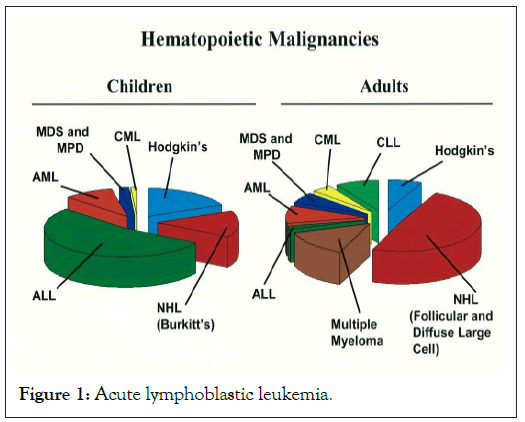
Figure 1: Acute lymphoblastic leukemia.
Acute lymphoblastic leukemia
ALL is characterized by the uncontrolled proliferation of immature lymphoid cells, specifically lymphoblasts, in the bone marrow and blood. The disease primarily affects lymphocytes, a type of white blood cell crucial for the immune system's function. ALL can present with various clinical features, such as anemia, thrombocytopenia an neutropenia, as well as organ infiltration, which can lea to a wide range of symptoms. Although the exact cause of ALL is unknown, several risk factors have been identified, including genetic predisposition, exposure to ionizing radiation and certain genetic syndromes [3-5].
This case report discusses the clinical course of a 7-year-old male patient who was diagnosed with ALL and outlines his diagnostic workup, treatment and long-term management.
Initial presentation
The patient, whom one will refer to as Tom to protect his privacy, presented to the pediatric oncology clinic with a two-month history of unexplained fatigue, pallor and easy bruising. His parents noted that he had become increasingly fatigued, with reduced energy levels and a noticeable decrease in his activity and playfulness. Tom's mother reported that he had developed multiple bruises over his body, which were not associated with any significant trauma [4].
On physical examination, Tom appeared pale an petechiae were observed on his extremities. He had mild hepatosplenomegaly, which raised suspicion of an underlying hematological disorder. There was no history of fever, recurrent infections or weight loss. Tom's parents reported no family history of cancer or hematological disorders. His growth and development had been normal until the onset of these symptoms [5].
Given the clinical presentation, a Blood Complete Count (CBC) was ordered, revealing the following abnormalities:
Hemoglobin: 7.2 g/dL (reference range: 11.5g/dL -15.5g/dL)
Platelet count: 30,000/μL (reference range: 150,000/μL -450,000/μL)
White blood cell count: 8,500/μL (reference range: 4,500/μL -11,000/μL)
Absolute neutrophil count: 1,200/μL (reference range: 1,500/μL -8,000/L)
Absolute lymphocyte count: 5,000/μL (reference range: 1,000/μL -3,500/μL)
Blast cells in the peripheral blood: 12%
These findings raised concerns about a hematological malignancy and further investigations were promptly initiated.
Diagnostic workup
Bone marrow aspiration and biopsy: Tom underwent a bone marrow aspiration and biopsy, which revealed hyper cellular marrow with a significantly increased number of lymphoblast’s (80% of nucleated cells). Immunophenotyping of the blast cells indicated that they were B-cell precursor lymphoblast’s consistent with a diagnosis of B-cell precursor ALL. Cytogenetic analysis showed a normal karyotype, which is typical in the majority of pediatric ALL cases.
Lumbar puncture: In addition to bone marrow evaluation, a lumbar puncture was performed to assess the presence of Central Nervous System (CNS) involvement. Cerebro Spinal Fluid (CSF) analysis showed no evidence of leukemic infiltration.
Additional investigations: Further tests, including flow cytometry and molecular genetics, were conducted to determine the subtype and risk stratification of Tom's ALL. The findings indicated that he had a standard-risk B-cell precursor ALL without any high-risk features.
Treatment
Chemotherapy: Tom was initiated on a standard induction chemotherapy regimen, which is the initial phase of treatment for ALL. This included a combination of chemotherapeutic agents such as vincristine, prednisone, daunorubicin an asparaginase. The goal of induction chemotherapy is to achieve a complete remission by eliminating the majority of leukemic cells from the bone marrow and blood.
During this phase, Tom experienced some common side effects of chemotherapy, including nausea, vomiting and transient hair loss. He also developed neutropenia, which required close monitoring for infections and the administration of prophylactic antibiotics [6-8].
Consolidation and maintenance therapy: Following the successful completion of induction chemotherapy, Tom proceeded to consolidation therapy, which aims to further reduce the number of residual leukemic cells. Consolidation involves high-dose methotrexate and cytarabine, among other agents. After consolidation, he entered the maintenance phase, which is a prolonged and less intensive treatment period aime at preventing disease relapse [9]. Maintenance therapy typically lasts for two to three years and includes oral chemotherapy (mercaptopurine and methotrexate) as well as periodic intrathecal chemotherapy to prevent CNS relapse [10].
Throughout his treatment, Tom received regular follow-up assessments, including CBC monitoring, liver function tests an renal function tests, to manage and mitigate potential treatmentrelate toxicities. Pediatric cancer is a term that encompasses a range of malignancies affecting children, adolescents and young adults. These cancers differ from adult cancers in many ways, including their types, causes and treatment approaches. Pediatric cancer poses unique challenges and requires a multidisciplinary approach to provide the best care and improve outcomes.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref ] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Bitzman M, Takano T, Williams S, Ciriaco H (2023) Pediatric Leukemia: Its Importance in Oncology and Interventions of Treatments in Supportive care. Clin Pediat. 08:248.
Received: 17-Nov-2023, Manuscript No. CPOA-23-28057; Editor assigned: 20-Nov-2023, Pre QC No. CPOA-23-28057; Reviewed: 04-Dec-2023, QC No. CPOA-23-28057; Revised: 11-Dec-2023, Manuscript No. CPOA-23-28057; Published: 18-Dec-2023 , DOI: 10.35248/2572-0775.23.08.248
Copyright: © 2023 Bitzman M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.