Immunome Research
Open Access
ISSN: 1745-7580
ISSN: 1745-7580
Case Report - (2019)Volume 15, Issue 2
Pemphigus herpetiformis, first described in 1975, is a rare subtype of autoimmune bullous disease that associates clinical features of dermatitis herpetiformis with immunological features of pemphigus. We present a 48-years-old female patient, with pruritic lesions located mainly in the upper limbs with 6 years of evolution. Physical examination revealed erythematous papules, some excoriated and vesicles of translucent content distributed on her arms, trunk and neck. Histological examination of a skin biopsy revealed the presence of sub epidermal vesicles associated with necrosis of the epidermis and perivascular lymphocytic infiltrate in the papillary and reticular dermis. The immunological study was positive for antibodies to intercellular IgG and anti-envoplakin antibodies. Anti-desmoglein 1 and 3 antibodies were negative. Considering these results, the clinical hypothesis of pemphigus herpetiformis was admitted. The positivity of the anti-envoplaquine antibody is often associated with paraneoplastic pemphigus, so a cancer screening was performed which was negative. Prednisolone and dapsone was introduced with resolution of lesions. To our knowledge this is the first clinical case of pemphigus herpetiformis with positive anti-envoplakin antibodies. This rare and often overlooked entity has a good prognosis, although there are cases reports with progression to pemphigus vulgaris or pemphigus foliaceus.
Pemphigus herpetiformis; Anti-envoplaquin antibodies; Autoimmune bullous disease
Pemphigus herpetiformis (PH), first described in 1975 by Jablonska et al, is a rare subtype of bullous autoimmune disease that associates clinical manifestations of dermatitis herpetiformis with immunological features of pemphigus [1]. The diagnosis is based on clinical, histopathological and direct immunofluorescence findings. PH exhibits IgG autoantibodies against desmoglein 1 in most of the cases, rarely IgG autoantibodies against desmoglein [2]. There are some cases with negative anti-desmoglein and positive anti-desmocollin antibodies [3-6].
A 48-years-old woman, previously healthy, presented with a 6- year history of pruritic lesions located mainly in the upper limbs and trunk. Physical examination revealed erythematous papules, some excoriated and translucent vesicles distributed over patient’s arms, trunk and neck. The mucous membranes were unaffected (Figures 1 and 2).
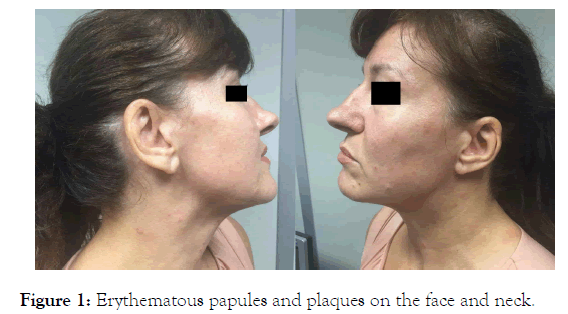
Figure 1. Erythematous papules and plaques on the face and neck.

Figure 2. Erythematous papules, some of them excoriated, on the upper limb.
A skin biopsy specimen revealed the presence of sub epidermal vesicles associated with necrosis of the epidermis and perivascular lymphocytic infiltrate in the papillary and reticular dermis (Figure 3). Serum indirect immunofluorescence (IIF) to human skin revealed IgG antikeratinocyte cell surface antibodies with titers 1/160 (normal<1/10). Enzyme-linked immunosorbent assay (ELISA) was negative for desmoglein (Dsg) 1, Dsg 2, bullous pemphigoid (BP) 180, BP230, desmocollin (Dsc) 1, Dsc 2, Dsc 3 and positive for envoplakin.
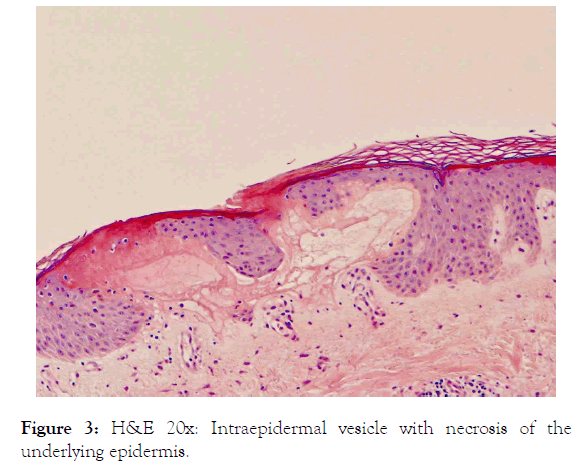
Figure 3. H&E 20x: Intraepidermal vesicle with necrosis of the underlying epidermis.
The positivity of the anti-envoplaquine antibody is often associated with paraneoplastic pemphigus, so a cancer screening was performed which was negative. Based on the clinical, histopathological and immunological findings, a PH with exclusive anti-envoplaquine antibodies was diagnosed.
Oral prednisolone (20 mg/day) and dapsone (50 mg/day) were introduced, with complete resolution of the lesions after 3 weeks, and then tapered off over 2 months without relapse. The patient remains in complete remission after 24 months of follow-up.
Pemphigus herpetiformis is a rare subtype of pemphigus [7]. This can occur at any age, more commonly between the 5th and 6th decade of life [8]. Of the few cases described, the clinical presentation varies between urticariform plaques to pruritic vesicle or blisters. The mucous membrane is usually intact. Histologically, the most common characteristic is an eosinophilic or neutrophilic spongiosis with variable acantholysis [5]. Direct immunofluorescence shows intercellular IgG and C3 in the epidermis, in 100% and 65% of the cases respectively [8]. The most frequent antibody is anti-desmoglein 1, although cases with negative anti-desmoglein and positive anti-desmocollin are reported [3-6]. As far as we know, our case is the first clinical case of pemphigus herpetiformis with high titers IgG antikeratinocyte cell surface antibodies, negative antidesmoglein and only positive anti-envoplakin.
Systemic corticosteroids alone or in combination with dapsone are described as effective in controlling lesions and pruritus. However, the evidence for the treatment of PH is limited, based only on case reports and series [4-8].
The prognosis is favorable, with an indolent course although there are cases described with progression to pemphigus vulgaris or pemphigus foliaceus [9-11].
To our knowledge this is the first clinical case of pemphigus herpetiformis with only positive anti-envoplakin antibodies. This rare and often overlooked entity has a wider variability in terms of the autoimmune response. It is important to recognise this disease since it was a good prognosis, and responses well to dapsone and/or low doses of steroids.
The authors declare no conflicts of interests.
Citation: Sousa C, Campos M, Lopes J, Baptista A, Oliveira A (2019) A Pemphigus Herpetiformis with Only Positive Anti-Envoplakin Antibodies: A Case Report. Immunome Res. 15:170. doi: 10.35248/1745-7580.19.15.170
Received: 31-Oct-2019 Accepted: 14-Nov-2019 Published: 21-Nov-2019
Copyright: © 2019 Sousa C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : none