Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Research Article - (2025)Volume 14, Issue 2
This study explores the use of Penile Doppler Ultrasound (PDU) under pharmacological stimulation to investigate Erectile Dysfunction (ED) in 53 cases in Conakry. The aim is to assess vascular response and identify underlying causes of ED through Doppler imaging after administration of vasoactive agents. The analysis focuses on blood flow dynamics, resistance indices, and peak systolic velocity, providing valuable insights into penile hemodynamics. Results demonstrate that PDU under pharmacological stimulation is an effective diagnostic tool for evaluating ED etiology, contributing to improved patient management and therapeutic decisions in a clinical setting.
Doppler; Ultrasound; ED; Pharmacotest; Etiology
Erectile Dysfunction (ED) is the permanent or partial inability to obtain or maintain sufficient penile rigidity for the performance of a satisfactory sexual act [1]. It currently affects more than 30% of men under 40 and more than 50% of men between 40 and 70 [2]. It is a multifactorial pathology involving functional or mixed organic mechanisms with a significant vascular component. The link between ED and Cardiovascular Risk Factors (CVRF) has been known since the 1980’s. More recently, studies have demonstrated the involvement of vascular causes in the occurrence of this condition [3,4]. Although phosphodiesterase 5 (IPDE-5) inhibitors are accepted as first-line treatment for ED, it is noted that 30 to 40% of men do not respond to this treatment [5,6] and that 40 to 50% of this resistance is of vascular origin [7-9]. This situation brings back to the fore the debate on the need for comprehensive multidisciplinary management of ED, in this era where vascular interventional techniques are experiencing renewed interest. A new therapeutic conceptualization of ED seems become more evident and would invite us to consider the attack no longer as a symptom, but rather as a nosological entity. Therefore, in any case of ED, concern for the etiology in the therapeutic process should lead, in addition to looking for comorbidity factors, to exploring the field of imaging in perpetual progress.
Penile Pharmaco Doppler Ultrasound (PEDP) is the reference examination for diagnosing the vascular-tissue origin of ED [10]. It makes it possible to obtain morphological and functional information of the structures of the penis during erection caused by the intracavernous injection of a pharmacological substance. Like any ultrasonographic exploration, it is operator-dependent. It is also subject to causes of interpretation error, such as patient hyper-adrenergy and anatomical variants of the cavernous arteries [3]. Due to its lack of standardization, the PEDP is rarely used by doctors treating ED. It is prescribed in only 10% of cases by urologists in the United States [11] and in 30% of cases by urologists, psychiatrist sexologists and endocrinologists in France [12]. All the same, it retains its indications and the results remain encouraging both in the early detection of cardiovascular events and in the morphological diagnosis and vascular disorders of the penile structures.
The present study was conducted by a mixed team of urologists and radiologists interacting between medical structures in Conakry. The methodology described by C. Bonnin and P. Bouilly [13] was retained for carrying out the PEDP. As part of a pioneering study with the primary motivation of establishing a vascular-tissue profile of patients with ED, the classic indications for performing PEDP were reviewed. The examination was therefore systematized for all patients presenting with ED. Patients were initially seen in a urology-andrology consultation before being subsequently referred to the imaging pool for PEDP performance.
Creation of the PEDP
The PEDPs were carried out in a comfortable, quiet room, in semi-darkness and in a temperate atmosphere. The patients were previously interviewed about the progress of the examination in order to reassure them and minimize the effect of anxiety, which is an important factor that can influence the results.
The examination took place in three stages
The first stage, or aorto-iliac arterial exploration, consisted of the study of the aorta, the common iliac, external iliac and hypogastric arteries, using a low frequency probe (3.5 MHz), looking for stenosing or occlusive lesions. Complete exploration of the arteries of the lower limbs has not been systematic.
The second stage or pharmacostimulation, also called pharmacotest, consisted of the intracavernous injection of prostaglandin E1 at a dose of 10 μg with the aim of inducing an erection in the subject with normal arterial function.
The third and final phase consisted of the morphological study of the corpora cavernosa and the measurement of velocimetric parameters. A 7.5 MHz probe was used for this purpose. The recording was carried out at 5 and 10 minutes for the arterial parameters and at 15, 20, and 25 minutes in certain patients for the venous parameters. The assessment of arterial function was made by measuring the peak systolic velocity Post Intracavernosal Injection (PSVpi) and the Systolic Rise Time (SRT). Veno- Occlusive Dysfunction (VOD), for its part, was assessed by measuring the Resistance Index (RI) and End-Diastolic Velocity (EDV).
Vasculotissular insufficiency was considered in the presence of a PSVpi value less than 25 cm/s or in the presence of a SRT greater than 110 ms when the PSVpi was between 25 cm/s and 35 cm/s. The absence of arterial insufficiency was considered for any PSVpi value greater than 35 cm/s.
In the absence of arterial insufficiency, the VOD was retained in the case of a EDV greater than 5 cm/s and an RI less than 0.85 on the one hand and in all cases with a EDV greater than 5 cm/s and an RI greater than 0.85 on the other hand. It was considered absent in the presence of a EDV less than 5 cm/s associated with an RI greater than 0.85 with systematic search for cavernous-venous leaks for all cases presenting an RI between 0.85 and 0.9. Table 1 reports the interpretation criteria based on the recorded parameters.
| Search for vascular tissue insufficiency | |||
|---|---|---|---|
| Parameters | Normal | Vasculotissular insufficiency | |
| PSVpi | >35 cm/s | <25 cm/s or 25 cm/s <PSVpi<35 cm/s with SRT>110 ms |
|
| RI | >0,85 | <0,85 | If:RI>0,85 and EDV>5 cm/s VOD or hyperadrenergy? |
| EDV | <5 cm/s | >5 cm/s | If:RI>0,9 No Cavernovenous leaks If:0,85<RI<0,9 Cavernovenous leaks? |
Table 1: Interpretation criteria.
Over a period of 20 months, we performed 53 penile pharmaco-Doppler ultrasounds on subjects with ED. The average age of the patients was 47.8 ± 17.4 years with extremes of 25 and 73 years. The age group of 45 to 64 was the most affected. The average duration of erectile dysfunction was 7 ± 1.7 months (Tables 2 and 3). One to three cardiovascular risk factors were found in 26.4% of patients (n=14). There were more than three in 11.3% of patients (n=6) and absent in the majority of cases (62.3%) (Figure 1). Aorto-iliac arterial exploration was normal in all patients (Figure 3). No abnormality of the corpora cavernosa was found (Table 4).
Overall, PEDP was normal in 54.7% of cases (n=29). Arterial insufficiency was found in 30.1% of patients (n=16) including 12 cases with PSVpi<25 cm/s and 4 cases with PSVpi between 25 cm/s and 35 cm/s and a SRT>110 ms. Veno-occlusive dysfunction was suspected in 15.1% of patients (n=8), including 5 cases with RI<0.85 and EDV>5 cm/s, and 3 cases with RI>0.85 and EDV>5 cm/s. 5.7% of patients were investigated for cavernous-venous leaks without success in all cases (Table 5). Post-procedure incidents were represented by two (02) cases of bruising, three (03) cases of pain at the injection site and three (03) cases of erection prolonged beyond 4 hours (Figure 2). The average duration of post-injection erection was 129 ± 11.6 min. The management of priapism cases did not require the creation of a cavernous-cancellous shunt in all cases. It consisted of the intracavernous injection of etilefrine in the 3 patients, supplemented by drainage with a 30G butterfly needle under local anesthesia with lidocaine spray in one patient.
The penile pharmaco doppler ultrasound examination whose invasive side is limited to the injection of vasoactive substance into the corpora cavernosa. Despite its low safety, it is not routinely used in the treatment of erectile dysfunction. If cost represents a significant obstacle, it is above all the current recommendations which limit its scope of application. Indeed, PEDP is indicated in ED secondary to pelviperineal trauma and in the case of association with a congenital or acquired deformity of the penis. The other indications being the failure of oral treatments, the patient's request, medicolegal reasons or even before penile prosthetic surgery [14].
In our study, we opted for its systematization taking into account its low potential for harm to the patient, but above all with the aim of popularizing its practice which until then was nonexistent. Despite this revision of the indications, we only carried out around fifty examinations over 20 months. A sample that is certainly small, but significant to achieve these preliminary results in our context.
| Age groups (years) | Age groups (years) | % |
|---|---|---|
| 25-34 | 6 | 11,3 |
| 35-44 | 11 | 20,8 |
| 45-54 | 17 | 32,1 |
| 55-64 | 12 | 22,6 |
| 65-74 | 7 | 13,2 |
| Total | 53 | 100 |
| Note: Average age=47.8 ± 17.4 years, Extremes: 25 and 73 years | ||
Table 2: Distribution of patients according to age groups.
| Duration of the DE | Effective | % |
|---|---|---|
| <3 | 12 | 22,6 |
| 3-5 | 16 | 30,2 |
| 6-8 | 11 | 20,8 |
| 9-11 | 9 | 17 |
| ≤ 12 | 5 | 9,4 |
| Total | 53 | 100 |
| Note: Average duration=7 ± 1.7 months, Extremes: 1 and 48 months | ||
Table 3: Distribution of patients according to duration of erectile dysfunction.
| Settings | Effective | % |
|---|---|---|
| Normal aortoiliac arterial exploration | 53 | 100 |
| Normal corpora cavernosa morphology | 53 | 100 |
| Pharmacodoppler ultrasound normal | 29 | 54,7 |
Table 4: Distribution of patients according to the overall result of the penile pharmacodoppler ultrasound.
| Examination’s conclusion | Effective | % | |
|---|---|---|---|
| Vascular tissue insufficiency 30.1% | PSVpi<25 cm/s | 12 | 22.6 |
| 25 cm/s<PSVpi<35 cm/s with SRT>110 ms | 4 | 7.5 | |
| Veno-occlusive dysfunction 15.1% | RI<0,85 and EDV>5 cm/s | 5 | 9.4 |
| RI<0,85 and EDV>5 cm/s | 3 | 5.7 | |
| Absence of caverno-venous leakage | 0,85<RI<0,9 | 3 | 5.7 |
Table 5: Distribution of patients according to vascular abnormalities found on penile pharmacodoppler ultrasound.
The multiplicity of PEDP implementation protocols is the basis of its lack of standardization. If all the protocols seem to be valid, each of them retains its methodology and its interpretation criteria. For our study, we adopted the protocol of C. Bonnin, which offers a clear methodology and interpretation criteria deemed accessible. More recently Sussman H. and his team described a dual-modality protocol combining the mini test and the maxi test, and whose reliability has been proven [1].
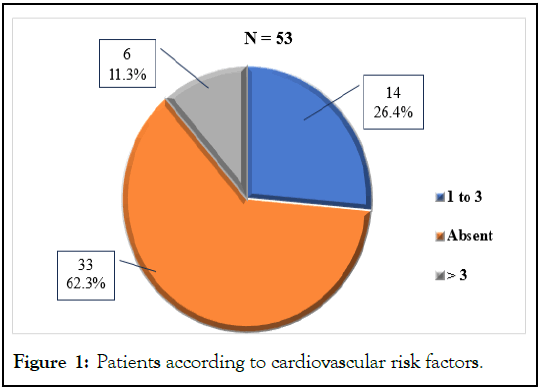
Figure 1: Patients according to cardiovascular risk factors.
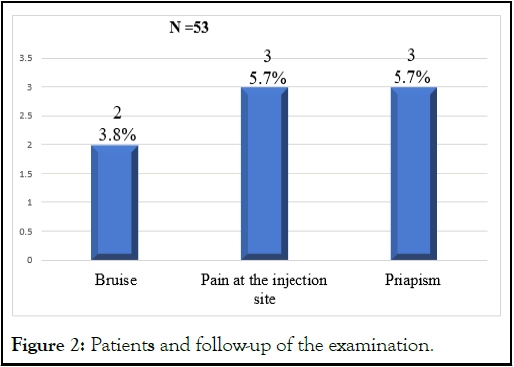
Figure 2: Patients and follow-up of the examination.
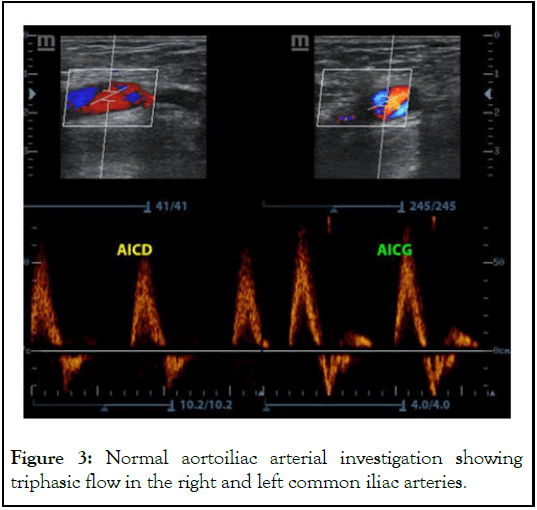
Figure 3: Normal aortoiliac arterial investigation showing triphasic flow in the right and left common iliac arteries.
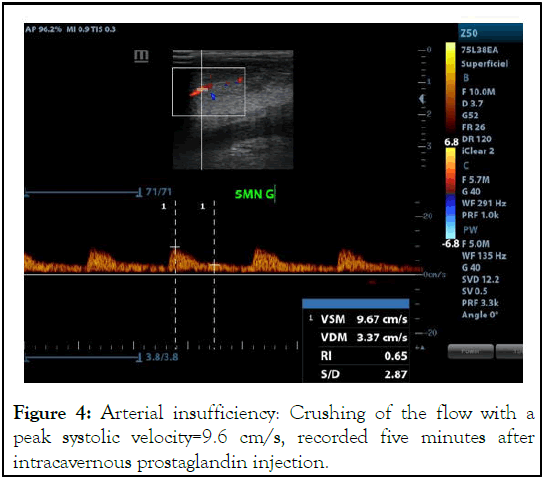
Figure 4: Arterial insufficiency: Crushing of the flow with a peak systolic velocity=9.6 cm/s, recorded five minutes after intracavernous prostaglandin injection.
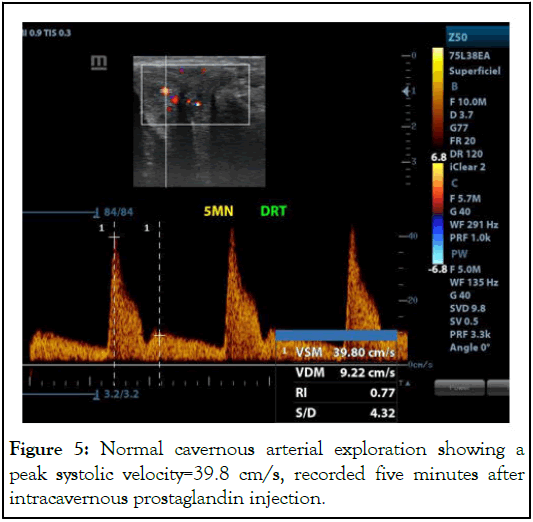
Figure 5: Normal cavernous arterial exploration showing a peak systolic velocity=39.8 cm/s, recorded five minutes after intracavernous prostaglandin injection.
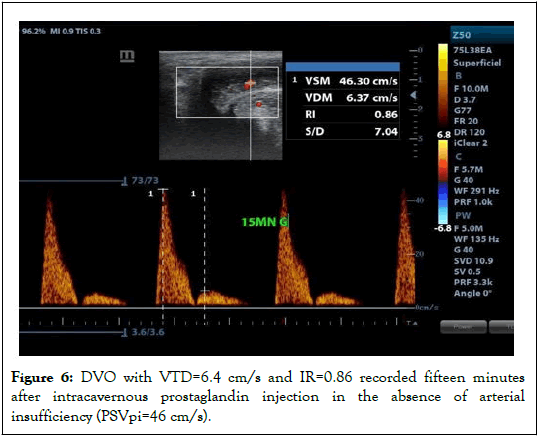
Figure 6: DVO with VTD=6.4 cm/s and IR=0.86 recorded fifteen minutes after intracavernous prostaglandin injection in the absence of arterial insufficiency (PSVpi=46 cm/s).
On average, our patients presented with ED 7 months before their consultation at our level. For extreme cases, this duration was 4 years; which materializes the delay in consulting the first time in the majority of cases. However, it is established that early detection as well as adequate and optimal management make it possible to prevent the progression of ED and improve therapeutic results for a better quality of life for patients [15].
The majority of patients had a normal penile duplex ultrasound assessment, reflected by a strong erection induced by the pharmacotest, which suggests that in a significant proportion of cases, ED could be of psychogenic or neurological origin (Figure 5). In theory, the injection of a vasoactive substance causes an erection in subjects with normal arterial function [16,17].
The main abnormalities observed were vasculotissular insufficiency and veno-occlusive dysfunction (Figures 4-6). Overall, our results are consistent with the work of Khanzada et al. [18] who identified in the majority of cases a psychological cause followed by arterial and then venous causes. Several authors have also identified these arterial and venous abnormalities in ED of organic origin. Vasculotissular insufficiency, characterized by insufficient blood flow in the penile arteries, is often linked to underlying cardiovascular diseases, while veno-occlusive dysfunction, where blood does not remain trapped in the corpora cavernosa, is often due to structural or functional abnormalities of the veins. It should nevertheless be noted that depending on the interpretation of the results in accordance with the adopted protocol, VOD can be mentioned in any case with RI>0.85 and EDV>5 cm/s in the same way as hyperadrenergy. We classified all patients in this situation in the VOD category. Some authors recommend carrying out additional maneuvers consisting of an additional injection of vasoactive substance, without significant modification of the results, at the cost of an increase in the rate of prolonged erections [19].
Cavernovenous Leaks (CVL) are the most common cause of organic ED. They represent the leading somatic cause of severe disability in men aged 25. The PEDP highlights CVL in 50% of patients whose ED is resistant to oral treatments [20]. In our study, we did not object CVL even if the interpretation of the velocimetric variables somewhat suggested their existence. The absence of identification of CVL does not necessarily cancel their existence. For a pioneering study, considerations related to the operator-dependent nature of the examination can be highlighted. Carrying out the cavernoscanner, which is the reference examination in this area, could have made it possible to draw a better conclusion.
Complications recorded following the examination were rare. Mainly these were bruising, pain at the injection site, and priapism. Sussman, et al. reported in their series that no penile hematoma was observed at the end of the examination and that no pressure dressing was useful [1].
Priapism has been reported in similar proportions by other studies [15,16]. The incidence of priapism after intracavernous injection of vasodilators is low but requires careful monitoring and rapid intervention to prevent serious complications [16]. The management of priapism cases did not require the creation of a cavernous-cancellous shunt in all cases. It consisted of the intracavernous injection of etilefrine supplemented by drainage with a 30G butterfly needle under local anesthesia with lidocaine spray in one patient.
Erectile dysfunction is a pathology of young adults around the 5th decade of life, mostly not presenting cardiovascular risk factors and taking on average more than 6 months to consult the first time.
Penile pharmaco-Doppler ultrasound allowed the morpho-structural evaluation of the corpora cavernosa and to differentiate vascular causes from other causes of erectile dysfunction. Vascular abnormalities were found in a little less than half of our patients with a predominance of vascular-tissue insufficiency over veno-occlusive dysfunction.
The results of the examination were simple in the majority of cases. The popularization of this examination will help to improve the early detection and prevention of cardiovascular events in men with erectile dysfunction, while optimizing its management.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Gnammi LR, Gamamou VA, Sabi Couscous H, Bah-Lâ??imam AH, Sy T, Diallo AB (2025) Penile Doppler Ultrasound under Pharmacological Stimulation in the Exploration of Erectile Dysfunction: Analysis of 53 Cases in Conakry. Andrology. 14:339.
Received: 12-Jul-2024, Manuscript No. ANO-24-35666; Editor assigned: 16-Jul-2024, Pre QC No. ANO-24-35666 (PQ); Reviewed: 30-Jul-2024, QC No. ANO-24-35666; Revised: 14-Jan-2025, Manuscript No. ANO-24-35666 (R); Published: 21-Jan-2025 , DOI: 10.35248/2167-0250.25.14.343
Copyright: © 2025 Gnammi LR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.