Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research - (2021)Volume 12, Issue 5
Background: To understand the awareness and knowledge about eye donation in the employees of a tertiary hospital. Methods: A structures Google form based cross sectional survey was conducted among 678 employees comprising of medical, nursing, students and paramedical staff. The responses were evaluated in Excel spreadsheet and tabulated. Results: 86% of the employees had awareness about eye donation however their knowledge regarding the same was either inadequate or incorrect. Only 63% had pledged their eyes and of the remaining about 63.5% were willing to pledge.
Conclusion: Awareness levels are high among the hospital workers but the lack of basic information is alarming. These need to be improved so that common people can be motivated to pledge and donate their eyes and correct the disparity between the need and availability of donor eyes for transplants.
Corneal blindness; Eye donation; Keratoplasty; Awareness; Willingness to pledge
Blindness and visual impairment are the terms used to label a decrease in vision from various diseases. The definition of blindness adopted by the national programme for control of blindness and visual impairment in the ministry of health and family welfare is visual acuity <3/60 in the better eye with available correction or visual acuity of <3/60 in the better eye [1].
In India, there are 8 million blind and 62 million visually impaired people which amounts to roughly one-fourth of the global burden [2]. Of these, corneal blindness remains to be the third leading cause of avoidable blindness. This encompasses both preventable and treatable corneal diseases. Approximately 68 lakh people suffer from corneal blindness in at least one eye; of these, 10 lakh people are blind in both their eyes [3]. The national blindness and visual impairment survey 2019 reported that corneal blindness was the leading cause of blindness among patients aged less than 50 years in India, accounting for 37.5% of the cases and was the second leading cause of blindness among patients above the age of 50 years [4]. Every year around 25000-30000 people with corneal blindness are being added which increases the prevalence to 0.16%. The major causes of corneal blindness noted are post-surgical bullous keratopathy, corneal dystrophy and degeneration and trachoma. Apart from these, infectious keratitis during childhood and adulthood, trauma and vitamin A deficiency plays a role as well. The final treatment option for such causes of blindness is a corneal transplant or keratoplasty. This depends on a matching supplydemand cycle which is not seen in India. Around 2.7 lakh corneas are in demand with the availability of only 63,000 annually [5]. This disparity begs the question about the cognizance of eye donation in the country.
It is imperative that healthcare personnel have adequate information about the same as they are the first point of communication with the kin of the deceased. The shortage of eye donations needs to be addressed at all levels of healthcare and hence all workers should be given proper education. We conducted this survey to assess the level of information hospital employees have despite working in the medical field. We hope to improve their knowledge so that it can have some contribution to improving the dismay in eye donations.
A community-based cross-sectional study was conducted amongst employees working in a tertiary care center in western India between 27 August 2021 and 29 August 2021. A standard pre-designed, close-ended, structured questionnaire was created using google forms and circulated through social media and email to all the employees, including doctors. The in house transplant coordinator was explained the content and purpose of the study as he was the single point of communication amongst the participants. The questions ranged from basic demographics, awareness and knowledge about eye donation and ultimately their willingness to pledge their eyes. The participants included doctors, nurses, paramedical staff, students, and managers working within the hospital premises. The results were extrapolated from the Google forms into a Microsoft Excel spreadsheet and analyzed.
A community-based cross-sectional study was conducted amongst employees working in a tertiary care center in western India between 27 August 2021 and 29 August 2021. A standard pre-designed, close-ended, structured questionnaire was created using google forms and circulated through social media and email to all the employees, including doctors. The in house transplant coordinator was explained the content and purpose of the study as he was the single point of communication amongst the participants. The questions ranged from basic demographics, awareness and knowledge about eye donation and ultimately their willingness to pledge their eyes. The participants included doctors, nurses, paramedical staff, students, and managers working within the hospital premises. The results were extrapolated from the Google forms into a Microsoft Excel spreadsheet and analyzed.
The primary aim of our study was to assess the level of information that the employees had regarding eye donation. We conducted the survey among 678 employees of the hospital of which 178 (26.25%) were nurses or nursing tutors, 126 (18.58%) were nursing college students, 99 (14.60%) were paramedical technicians, 76 (11.21%) were executives, 65 (9.59%) were senior consultants, 50 (7.37%) were interns or trainees, 47 (6.93%) were managers and 37 (5.46%) were medical officers. Detailed age-wise distribution is shown in Table 1. These included 380 (56%) females and 298 (44%) males with a mean age of 35.5 ± 1.2 years and 42.1 ± 1.1 years respectively.
| Designation | Age | Grand total | |||||
|---|---|---|---|---|---|---|---|
| 18-24 | 25-34 | 35-44 | 45-54 | 55-64 | 65+ | ||
| Executive | 16 | 33 | 21 | 4 | 1 | 1 | 76 (11.21%) |
| Interns/trainee | 33 | 9 | 4 | 3 | 1 | 0 | 50 (7.37%) |
| Manager | 1 | 19 | 17 | 10 | 0 | 0 | 47 (6.93%) |
| Medical officer | 4 | 20 | 8 | 4 | 1 | 0 | 37 (5.46%) |
| Nurse/nurse tutor | 79 | 82 | 15 | 1 | 1 | 0 | 178 (26.25%) |
| Nursing college student | 110 | 14 | 0 | 1 | 1 | 0 | 126 (18.58) |
| Paramedical technician | 18 | 52 | 23 | 4 | 2 | 0 | 99 (14.60%) |
| Senior consultant | 1 | 18 | 26 | 12 | 7 | 1 | 65 (9.59%) |
| Grand total | 262 (38.64%) | 247 (36.43%) | 114 (16.81%) | 39 (5.75%) | 14 (2.06%) | 2 (0.29%) | 678 |
Table 1: Age-wise distribution of participants across the organization.
The questions in the survey were divided into demographic data, eye donation awareness and willingness to pledge. Table 2 shows the responses to the questions about eye donation. We found that 580 responders who account for 86% of the employees were aware that eye donation is possible. However, there were a lot of people who had inadequate information about other questions. Notably, 50% believed that the entire eye can be transplanted. Also, 25% of respondents had misconceptions about eye donation (Figure 1).
| Sr. no. | Questions | Responses (n=678) |
|---|---|---|
| 1 | Can eyes be donated? | |
| No | 98 (14%) | |
| Yes | 580 (86%) | |
| 2 | Is there an age limit for eye donation? | |
| No | 462 (68%) | |
| Yes | 216 (32%) | |
| 3 | Can a living person donate his/her eyes? | |
| No | 328 (48%) | |
| Yes | 350 (52%) | |
| 4 | Within how many hours of death can eyes be removed? | |
| <8 hours | 523 (77%) | |
| >12 hours | 29 (4%) | |
| 8-12 hours | 126 (19%) | |
| 5 | Can my blood relatives give consent for donation after my death? | |
| No | 97 (14%) | |
| Yes | 581 (86%) | |
| 6 | Is buying/selling of eyes legal? | |
| No | 459 (68%) | |
| Yes | 219 (32%) | |
| 7 | Does the removal of eye cause facial disfigurement? | |
| No | 408 (60%) | |
| Yes | 270 (40%) | |
| 8 | If I donate my eyes when I die, I will be blind by birth in my next life. | |
| False | 511 (75%) | |
| True | 167 (25%) | |
| 9 | Can the entire eye be transplanted? | |
| No | 340 (50%) | |
| Yes | 338 (50%) | |
| 10 | If I have cataract or have been operated for cataract, my eyes cannot be donated. | |
| False | 366 (54%) | |
| True | 312 (46%) | |
| 11 | Living human beings can pledge their eyes. Have you pledged your eyes? | |
| No | 250 (37%) | |
| Yes | 428 (63%) |
Table 2: Survey responses from the participants.
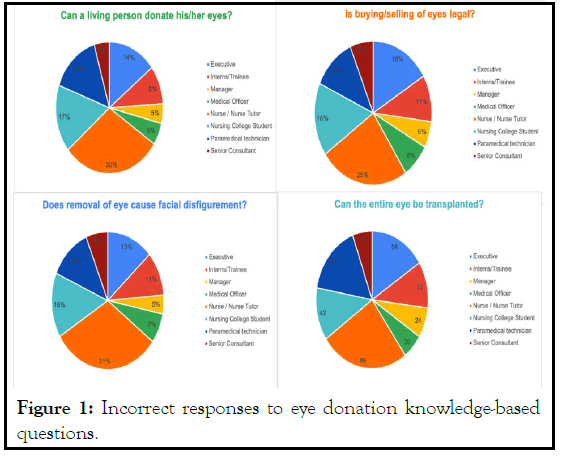
Figure 1: Incorrect responses to eye donation knowledge-based questions.
The four questions with incorrect responses are tabulated below with responses from different employees based on their work designation. These questions constitute the most common myths that people have about donating eyes. When asked if a living person can donate eyes, 30% of nurses, nursing tutors and 17% of nursing college students responded with a yes. 25% of nurses and 16% of executives said that buying/selling of eyes is legal. 31% of nurses and 15% of nursing students were of the opinion that eye donation causes facial disfigurement and scarring. A whopping 86% of the nurses and 56% of paramedical technicians believed that the entire eye can be transplanted.
Corneal blindness includes a large proportion of avoidable blindness in India. This also depends on the prevalence of endemic corneal diseases in the country and the community awareness of eye donation. Community awareness begins at the level of healthcare personnel who are the first responders in times of organ donation. If they are adequately informed about eye donation, only then they can educate locals, and that will, in turn, lead to more pledges for eye donation and encourage blood relatives to honor that pledge at the time of death.
This study aimed to address the significant disparity between the perception and awareness about eye donation among different healthcare workers. Doctors and particularly ophthalmologists have detailed knowledge about eye donation. Still, the data from our study shows a lack of the same in other groups despite working in a hospital with eye retrieval facilities and programs. These differences can be attributed to differences in the level of information grasped by non-medico subjects. A study from a hospital set up in India revealed that 59.4% of their staff had significant misconceptions about different organ transplants, including the eye [6]. This study reinforces the same issue about rampant myths not only about eye donation but also other organs.
63% of our participants have already pledged their eyes. Of the remaining 37% participants, 67.5% were willing to pledge their eyes, demonstrating that awareness needs to be initiated at their level to proportionately include their families, which can create a mass chain of communication. In other population-based surveys from India, 41.5% from Delhi, 52% from north-western India and 44.9% from Hyderabad were willing to donate [7,8].
Our study reported 86% of subjects being aware regarding eye donation. In a study among the south Indian population, around 50.7% of the subjects had awareness about eye donation [9]. A sizeable urban population-based survey showed that only 30.7% had information about eye donation, and only 0.1% had pledged [10]. Similarly, a large study from rural Andhra Pradesh (32.9%) showed very little population awareness regarding eye donation [11]. This shows the imbalance in awareness of eye donation and also the inadequate spread of knowledge between rural and urban areas.
There are many misconceptions about different aspects of eye donation that need to be addressed at grassroots levels. Lack of knowledge and purpose, along with myths of eye donation, can be considered a hurdle in convincing the people and obtaining enough pledges. Mass media needs to be utilized more if we increase the number of donor corneas each year. For multispeciality hospitals with eye departments, whether governmental or not, their employees of all levels must actively spread accurate information among the patients and their kin [12]. This will proactively increase the rates of donation across the country in rural as well as urban areas. Apart from the who, what, when and how of eye donation, people need to understand the importance of discussion with family members, should the need arise. They will be the linchpin to motivate from within the family and surrounding community.
Many countries have the concept of “presumed consent”, where the dead person is assumed to be a donor even if they have not registered themselves when alive. After appropriate consent from the next-of-kin, eye donation is carried out. This concept in India is not yet materialized, and there have been no known efforts to do so. India has the “opt-in” system where the donor has to register themselves, and then only eye donation can be made with prior consent from the donor or legal next of kin. If we are to balance the awareness to action ratio for corneas, we need some specific changes in the legislation [13,14].
This survey attests to the fact that awareness regarding eye donation is lacking in some proportion among the employees of a tertiary care hospital. The underutilization of the hospital workforce can be a hindrance in spreading awareness. It is important to guide them with proper information so that they can be a source to the general population.
None
None
None
Citation: Desai AK, Mehta PK (2021) Perception and Stigma Regarding Eye Donation among Employees in a Tertiary Care Centre. J Clin Exp Ophthalmol. 12: 890
Received: 10-Sep-2021 Accepted: 24-Sep-2021 Published: 01-Oct-2021 , DOI: 10.35248/2155-9570.21.12.890
Copyright: © 2021 Desai AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.