Advanced Techniques in Biology & Medicine
Open Access
ISSN: 2379-1764
ISSN: 2379-1764
Research Article - (2018) Volume 6, Issue 3
Keywords: Patient safety; Safety practice; Health care provider
Patient safety practice is a process, or structure which can reduces the probability of adverse events resulting from exposure to the health care system across a range of diseases and procedures [1]. It is the cornerstone of high-quality health care. An effort defining patient safety practices includes prevention of harmful events and negative health care outcomes, such as mortality and morbidity [2].
Patient safety practices have been defined as “those actions implemented to reduce the risk of adverse events related to exposure to health care across a range of diagnoses or conditions” [3]. The healthcare industry involves high risk of morbidity and mortality thus it is considered to be a high hazard industry and it needs assessment of safety culture [4,5].
Patient safety forms the foundation of healthcare delivery as biological, physiological, and safety needs form the Maslow’s hierarchy. Improving the safety of healthcare delivery saves lives, helps to avoid unnecessary complications, and increases the confidence in receiving health care [6,7].
Even though unintended harm to patients is not a new phenomenon, the solutions proposed to improve patient safety is determined by how well health care providers perceive and practice patient safety, how well caregivers work together as a team, how effectively they communicate with one another and with patients, how carefully the care delivery processes and supporting systems of care are designed [8,9].
Health care providers still face many challenges which include negative perception about patient safety practice while they are trying to keep safety [2,8].
Safety of the health care is the heart of health care system thus improving safe care delivery saves live, avoids unnecessary complication, and saves unnecessary health care costs and increase trust of patient on receiving medical care. Even though more or less documented methods to prevent the occurrence of many of the health care errors are available, these errors and the result of adverse events are causes of death and injury in health care organization [10].
Even though attention has been given to safe practices that reduce the risk of harm resulting from the processes, systems, or environments of care but uniformly reliable safety in healthcare has not yet been achieved. Due to that every day, patients are still harmed or nearly harmed, in healthcare institutions [11]. This harm is not intentional rather it can be due to health care system failures, leadership shortfalls or human behavioral factors which can be avoided. One of the factors that related to health care system failures is negative perception of health care providers towards patient safety [6,12].
International study findings revealed that low practice and perception of patient safety can increase preventable errors, health care associated infection, physical and psychological disability, health care cost, hospital stay, patient dissatisfaction and may lead to death [13-16].
According to USA government agency organization reports on the patient safety, unsafe health care can harm the patient and leads to adverse, but data related to perception of health care providers are unavailable or unreliable [15,17].
WHO regional director stated report on the African Region revealed most countries lack national policies on safe health-care practices. Economy and unavailability of clear strategies, guidelines, tools and patient safety standards remain major concerns. Furthermore, understanding of the problems associated with patient safety and patient safety practice were hindered by inadequate data [18].
Study done by Assefa T at Jimma University Specialized Hospital indicated the presence of low patient safety practice and presence of preventable medical errors in the hospital. The investigator relates patient safety with prevalence of medical errors [19].
Study conducted at Hawassa town health facilities indicated that, low level of quality of work life is associated with low quality of care, lower patient satisfaction, negatively affect public image, and as a whole hinders positive perception for safe health care practice decrease safety in health care improvement [20].
Even though one of the ultimate aims of Ethiopian National Health Care Quality Strategy is to consistently ensure and improve patient safety practice, the country is not an exception to this problem [20]. Achieving an acceptable standard of patient safety practice requires all healthcare settings develop patient safety culture that include both a positive perception on culture of safety and organizational support for safety practice. This will not be possible unless the perceptions of the health care providers and management are positively managed and directed.
Therefore, the main aim of this study was to assess perception of patient safety practice and associated factors among health care providers of Jimma zone public hospitals, South West Ethiopia.
Study area and Period: The study was conducted at public hospitals found in Jimma Zone, Oromia Regional state. Jimma zone is one of the 18 zones of the Oromia Regional State found at 352 km from Addis Ababa, the capital city of Ethiopia, in the South western part [20,21]. This Zone has a total population of 2,486,155 of whom 1,250,527 are men and 1,235,628 women. Jimma zone has four primary (Limmu Genet, Agaro, Seka hospitals and Shenen Gibe Hospital) and one referral and teaching Hospitals (Jimma University Medical Center (JUMC)). The population being served by the hospitals is estimated to be more than fifteen million including people from border zones and southern part of Sudan. The hospital has out-patient and inpatient services, maternal and child health services, referral and follow-up services, physiotherapy and rehabilitative services, intensive care and recovery services .These hospitals have a total of 1092 health care providers [22-26]. The study was conducted from March 15 to April 9, 2017.
Study design: Facility based cross-sectional study was employed.
The sample size was determined using a formula for estimation of single population proportion of assumptions of: an expected proportion perception of patient safety practice (p) of 50% since no previous study done in the country, Z a/2 is Z value at 95% Confidence level (1.96) and 0.05 margin of error (d):
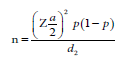
Using finite population correction formula and adding 10% non -response rate the final sample size was 312.
Sampling technique /Sampling procedures
Stratified random sampling techniques based on the hospital of the participant were used to select the required sample size. After the sample size proportionally allocated to each hospital then it was allocated proportionally to each profession in that hospital. Simple random sampling method was used to select study participants from each profession. The study was targeted clinical and non-clinical staff of hospitals, like physicians, nurses, midwives, psychiatrist, pharmacy, laboratory staff, radiology staff, anesthesia staff, dentistry staff, supervisors, and hospital managers.
Data collection instrument and collection procedure
Validated data collection instrument was adapted from previous similar studies and modified and contextualized to the local situation (adapted) [1,9,27]. A total of 42 items categorized into 12 dimensions. These dimensions are overall perception of patient safety practice which was measured by four items, teamwork with in the unit measured by four items, non-punitive response to error measured by three items, staffing measured by four items, supervisor expectation and action promoting patient safety containing five items, feedback and communication about error comprising six items, frequency of event report which was measured by three items, management support for patient safety contains four items, teamwork across the unit measured by four items, hospitals handoff and transfer of patient contain three items, organizational learning-continuous improvement containing three items, patient safety grade measured by one item and one item which asks number of event report within the last one year. Items were scored using a four-point Likert-type response scale reflecting the agreement.
Data collection procedures
Data were collected using a self-administered questionnaire. Trained five BSc and one MSc nurses were facilitated the data collection procedure. The principal investigator supervised the overall data collection.
Data quality management
Pre-testing of the data collection instrument was conducted at Bedelle Hospital using 5% of the total sample size. Following the pretest, the instrument was revised in terms of its clarity, understandability and simplicity. Reliability was checked and found to be Cronbach’s alpha (α=0.81). Two days training and supervision were provided for the data facilitators and supervisor. Each filled questionnaire was checked for completeness by data facilitators and supervisor every day.
Data analysis procedures
The collected data was sorted, checked, arranged and enterred into the Epi-Data version 3.1 then exported to IBM SPSS version 20 for analysis. Descriptive statistics, Bivariate and Linear regression analysis was performed. All variables with p-value less than or equal to 0.25 in bivariate analysis was entered into multivariable linear regression model. Finally, multivariable linear regression was done to see the association of dependent and independent variables. P-value of less than and equal to 0.05 were considered to declare statistical significance.
Ethical consideration
Ethical clearance was obtained from Institutional Review Board (IRB) of Institute of Health, Jimma University. Permission letters were also obtained from each of the Jimma zone public hospitals Chief Executive Officer. The respondent’s privacy and confidentiality of the information was assured throughout the study procedure, and they have been told that they have all the right not to involve in the study or not to answer any of the questions. The research team had made sure that any data is collected after taking full consent of participants.
A total of 306 health care providers from 5 hospitals of the Jimma zone was included in the study with a response rate of 98.1%. Slightly more than half 173 (56.4%) of the study participants were male. The mean age of the respondents was 27.01 with minimum age of 20 and maximum age of 54 years. About forty six percent 140 (45.8%) of the study participants earn 4001-10000 Ethiopian Birr monthly. From these, 188 (61.4%) of them found in the age category of 26-35 years. More than half of the respondents 169 (55.2%) were single. Regarding educational status, the majority of the respondents 208 (68%) had bachelor degree and a relatively low proportion 2 (0.7%) had certificate (health assistant). About sixty percent 183 (59.8%) of them had 1-5 years of work experience and 103 (33.7%) of them were working minimum of half a year and maximum of one year in their current working units. Majority 175 (57.2%) was nurses while the lowest proportion 6 (2%) was radiographers and higher proportion 48 (15.7%) of them was working in medical ward. More than one-half 179 (58.3%) of the study participants are Oromo ethnic group. About two-thirds of respondents 195 (63.7%) worked greater than 40 h per week with minimum of 32 and maximum of 126 h. From the total study participants 294 (96.1%) of them had direct interaction with patient care (Table 1).
| Variable | Category | F | % |
|---|---|---|---|
| Sex | Male | 173 | 56.5% |
| Female | 133 | 43.5% | |
| Marital status | Single | 169 | 55.2% |
| Married | 134 | 43.8% | |
| Divorced | 3 | 1.0% | |
| Educational status | Health assistant (certificate) | 2 | 0.7% |
| Diploma | 82 | 26.8% | |
| Bachelor degree | 208 | 68.0% | |
| Graduate degree | 14 | 4.6% | |
| Ethnicity | Oromo | 179 | 58.5% |
| Amhara | 70 | 22.5% | |
| Kafa | 8 | 2.6% | |
| Tigre | 6 | 2.0% | |
| Dawuro | 3 | 1.0% | |
| Yem | 18 | 5.9 % | |
| Gurage | 20 | 6.55% | |
| Other | 2 | 0.65% | |
| Age category | 18-25 years | 106 | 34.6% |
| 26-35years | 188 | 61.4% | |
| 36-45 years | 9 | 2.9% | |
| >45 years | 3 | 1.0% | |
| Salary in Ethiopian Birr | 1400- 2500 | 29 | 9.5% |
| 2501- 4000 | 132 | 43.8% | |
| 4001-10000 | 140 | 45.8% | |
| >10000 | 5 | 1.6% | |
| Profession/Job title | Nurses | 175 | 57.2% |
| Physician | 22 | 7.2% | |
| Laboratory Technician | 22 | 7.2% | |
| Pharmacist | 25 | 8.2% | |
| Manager/Supervisors | 24 | 7.8% | |
| Midwifery | 25 | 8.2% | |
| Radiologist | 6 | 2.0% | |
| Anesthesiologist | 7 | 2.3% | |
| Working unit in the Hospitals | Medical ward | 48 | 15.7% |
| Surgical ward | 42 | 13.7% | |
| Operation Theatre | 13 | 4.2% | |
| Gynecology ward | 15 | 4.9% | |
| Maternity and labor | 28 | 9.2% | |
| Pediatric OPD and ward | 25 | 8.2% | |
| Emergency OPD | 15 | 4.9% | |
| Cold OPD | 11 | 3.6% | |
| Ophthalmology | 4 | 1.3% | |
| Psychiatry | 8 | 2.6% | |
| ICU | 5 | 1.6% | |
| Radiology | 6 | 2.0% | |
| Anesthesia | 5 | 1.6% | |
| Dental clinic | 8 | 2.6% | |
| Pharmacy | 23 | 7.5% | |
| Laboratory | 23 | 7.5% | |
| Chronic illness follow up | 21 | 6.9% | |
| Administrative | 6 | 2.0% | |
| Year of experience | <1 year | 90 | 29.4% |
| 1-5 years | 183 | 59.8% | |
| 5-10 years | 23 | 7.5% | |
| >10years | 10 | 3.8% | |
| Experience in the current unit | <0.5 year | 53 | 17.3% |
| 0.5-1year | 103 | 33.7% | |
| >1 year | 150 | 49.0% | |
| Work hour per week | <=40 h | 111 | 36.3% |
| >40 h | 195 | 63.7% | |
| Direct interaction with patient | Yes | 294 | 96.1% |
| No | 12 | 3.9% |
Table 1: Socio-demographic characteristics of health care providers of Jimma zone public hospitals, March, 2017 (n=306).
Composite frequency of positive responses
From the all dimension only teamwork within the unit had areas of strength (79.40%) which is above 75%. Areas that need improvement those with composite percentage of positive response less than 50% were frequency of event report (28.32%), hospital management support for patient safety (34.75%), overall perception of patient safety (36.77%), hospitals handoffs and transfer of patients (41.39%), nonpunitive response to error (44.77%), teamwork across the unit (47.47%) and feedback and communication about error (48.75%) Table 2.
| S. No. | Dimensions | (%) |
| 1 | Composite percentage of perception of patient safety practice. | 36.77% |
| 2 | Team Work within Units | 79.40% |
| 3 | Team Work across the Units | 47.47% |
| 4 | Non-punitive Response to Error | 44.77% |
| 5 | Supervisor Expectations and Actions Promoting Patient Safety | 59.28% |
| 6 | Feedback and Communications about Error | 48.75% |
| 7 | Frequency of Event Reporting | 28.32% |
| 8 | Staffing | 59.80% |
| 9 | Hospital management support for patient safety | 34.75% |
| 10 | Hospital handoffs and transition | 41.39% |
| 11 | Organizational learning/continuous improvement | 54.25% |
| 12 | Over all patient safety grade | 65.36% |
Table 2: Composite frequency of positive responses for each dimension on perception towards patient safety practice among health care providers of Jimma zone public hospitals, March 2017 (n=306).
Bivariate analysis was done to select candidate variables for multivariable linear regression. Accordingly, all socio-demographic, teamwork within the unit, teamwork across the unit, supervisors’ expectation and action promoting patient, communication openness feedback and communication about error, frequency of event reporting, non-punitive response to error, staffing, hospital management support, hospitals handoffs and transfer of the patient and organizational learning-continuous improvement were interred one by one. From these, 07 variables were selected for multivariable linear regression analysis having p value of less or equal to 0.25 (Table 3).
| Unstandardized Coefficients | t | P | 95% CI for B | |||
|---|---|---|---|---|---|---|
| Model | β | Std. Error | LB | UB | ||
| Age | -0.007 | 0.023 | -0.301 | 0.764 | -0.053 | 0.039 |
| sex** | 0.211 | 0.168 | 1.251 | 0.212 | -0.121 | 0.542 |
| Marital status | -0.15 | 0.168 | -0.893 | 0.373 | -0.481 | 0.181 |
| Ethnicity | 0.049 | 0.048 | 1.034 | 0.302 | -0.044 | 0.143 |
| Educational status | 0.006 | 0.202 | 0.032 | 0.975 | -0.392 | 0.404 |
| Monthly income | -2.68 | 0 | -0.424 | 0.672 | 0 | 0 |
| Profession/Job title | -0.004 | 0.039 | -0.106 | 0.915 | -0.081 | 0.073 |
| Years of Experience | 0.04 | 0.036 | 1.128 | 0.26 | -0.03 | 0.111 |
| Teamwork within the unit** | 0.102 | 0.044 | 2.32 | 0.021 | 0.016 | 0.189 |
| Teamwork across the unit** | 0.189 | 0.079 | 2.38 | 0.018 | 0.033 | 0.346 |
| Supervisors expectation & action promoting patient safety | -0.043 | 0.048 | -0.897 | 0.37 | -0.136 | 0.051 |
| Communication openness feedback ** | 0.083 | 0.035 | 2.333 | 0.02 | 0.013 | 0.152 |
| Frequency of event reporting | -0.001 | 0.048 | -0.026 | 0.979 | -0.096 | 0.093 |
| Non-punitive response to error** | 0.19 | 0.055 | 3.462 | 0.001 | 0.082 | 0.297 |
| Staffing** | 0.104 | 0.055 | 1.879 | 0.061 | -0.005 | 0.213 |
| Hospital management support for patient safety | -0.008 | 0.087 | -0.093 | 0.926 | -0.179 | 0.162 |
| Hospitals handoffs and transfer of patient** | 0.072 | 0.059 | 1.225 | 0.222 | -0.044 | 0.187 |
| Organizational learning-continuous improvement | 0.004 | 0.067 | 0.053 | 0.958 | -0.129 | 0.136 |
Table 3: Bivariate Analysis Showing lists of candidate variables for multivariable linear regression in the study of Perception of patient safety practice and associated factors among health care providers of Jimma zone public hospitals, March, 2017 (n=306). (Outcome variable: Perception of patient safety practice **=Candidate variables for multivariable linear regression, LB=Lower Bound and UB=Upper Bound).
Seven variables with p-value less than or equal to 0.25 in bivariate analysis were entered in the final model. From those variables teamwork within the unit, teamwork across the unit, staffing, non-punitive response to error and communication openness were found to have a significant association with overall perception of patient safety practice. As non-punitive response to error increases by one unit perception of patient safety practice increase by 0.190 (p<0.001), CI (0.090, 0.290)). Perception of patient safety practices increase by 0.168 as teamwork across the unit score increases by a unit (p=0.023), CI (0.023, 0.313), by 0.113 (p=0.026), CI (0.013, 0.212). As staffing score increase by one unit, similarly perception of patient safety practice also increases by 0.095 (p=0.012), CI (0.021, 0.170)) for one unit increases in score of teamwork with in the unit, perception of patient safety practice will increase by 0.065 (p= 0.030), CI (0.006, 0.124)) for communication and feedback about error score by keeping other variables constant (Table 4).
| Study variables | Unstandardized Coefficients | t | p | 95% CI for β | ||
|---|---|---|---|---|---|---|
| β | Std. E | LB | UB | |||
| Sex | 0.204 | 0.154 | 1.32 | 0.188 | -0.1 | 0.507 |
| Teamwork within the unit | 0.095 | 0.038 | 2.522 | 0.012** | 0.021 | 0.17 |
| Teamwork across the unit | 0.168 | 0.074 | 2.279 | 0.023** | 0.023 | 0.313 |
| Communication openness and feedback aboto error | 0.065 | 0.03 | 2.182 | 0.030** | 0.006 | 0.124 |
| Non-punitive response to error | 0.19 | 0.051 | 3.753 | <0.0 <0.001** | 0.09 | 0.29 |
| Staffing | 0.113 | 0.05 | 2.23 | 0.026** | 0.013 | 0.212 |
| Hospitals handoffs and transfer of | 0.072 | 0.057 | 1.265 | 0.207 | -0.04 | 0.184 |
Table 4: Multivariable Linear Regression Analysis final model for the study perception of patient safety practice among health care providers of Jimma zone public hospitals, March 2017 (n=306). (Outcome variable: Perception of patient safety practice, **= significantly associated study variables).
Concerning perception of patient safety the result showed that composite percentage of positive response (36.77%). This result showed that the hospitals had low patient safety practice. This result is comparable with study done in Egypt at teaching hospital in Cairo [28], but inconsistent with study in Saudi Arabia Riyadh [29].
Overall perception of patient safety (36.77%), non-punitive response to error (44.77%), frequency of event report (28.32%), teamwork across the unit (47.47%), hospital management support for patient safety (34.75%), hospital handoffs and patient transfer (41.39%) and communication openness and feedback about error (48.75%). This result is in line with study conducted in Qatar [30,31].
This study revealed the highest frequency of patient safety as team work within the unit which was 79.4%. This shows participants are positive about supporting one another, working together as a team and doing things to improve patient safety. The result is similar with the study done in Jordan [32] and Sri Lanka [33].
According to this study finding positive perception of the dimension of hospital management support for patient safety was (34.75%). This shows that hospital managers do not provide work climate that promotes patient safety and their actions do not show patient safety as priority. The result is inconsistent with the study done in Nigeria [34,35]. This variation might be due to the differences in location and size of hospitals, level of staffing, style of leadership, management strategy and relationships with in-hospital staff. The finding on communication openness and feedback about error composite positive percentage is about (48.75%) which shows poor communication between staff, managers and staff as well poor feedback giving system about error. These hinder patient safety practice. The result is similar with study done in Jordan [31] and Turkey [36].
The non-punitive response to error (44.77%) received below 50% scores revealing that employees are not at ease when it comes to reporting errors. The event reporting which is an essential component for achieving a learning culture, can happen only to a non-punitive environment where events can be reported to people being blamed but this result show response to error is through shaming and blaming. The result is similar with study conducted in Egypt [28].
Another dimension with the lowest composite percentage of this study is frequency of event reporting (28.32%) means that only 28.32% of the Health care provider’s responses reflected positive opinion about the frequency of event report. This indicates that there is a fear of reporting an event which might be due to punishment, a culture of blame or it might be due to absence of reporting system. This result is similar with study at Gondar University Comprehensive Specialized Hospital [37].
Factors associated to patient safety perception
In this study communication and feedback about errors were identified as factors that have significant association with perception of patient safety practice. This shows proper communication with and across healthcare teams, among staffs and managers as well between managers and supervisors are vital at least to minimize threats to patient safety. This result is consistent with study done in Saudi Arabia [29,38] and in Jimma University specialized hospital [20].
Non-punitive response to error is also one of the factors that have significant association with perception of patient safety practice in this study. This indicates response to an error should be in a way of learning from it rather than blaming others. It is similar with study done in Lebanese [37-39] but inconsistent with study done in Saudi Arabia [30]. The variation might be due to difference in location, level of hospitals or organizational behavior. According to this study finding, both teamwork within the unit and across the unit are significantly associated with perception of patient safety practice which implies in healthcare environment, teamwork plays crucial role [40,41]. The result is consistent with study conducted in Jordan [31], Saudi Arabia [29,36] and Lebanese [37] which may suggest every concerned body the importance of the team in health service delivery. In this study staffing on work condition is also significantly associated with perception of patient safety. This suggests proper distribution of staff in the unit facilitate working condition and important to handle work load. It is consistent with study done in Qatar [30,42] and Egypt [28].
The current study provides insight into how health care providers perceive patient safety practice and results from this study point out low perception towards patient safety practice among health care providers. The result also highlighted areas that required improvement, as perceived by health care providers. These areas include frequency of event report, hospital management support for patient safety, communication openness, hospital handoff and transition, nonpunitive responses to errors and teamwork across units. Patient safety is an integral part of the delivery of quality patient care, and achieving an acceptable standard of patient safety requires that all healthcare settings develop patient safety systems including both a positive culture of safety and an organizational support for safety processes. Thus to increase the positive perception of patient safety practice among health care providers and management’s building safety culture that eliminate blame, fear and silence regarding errors might be mandatory.
All authors declared that they have no conflict of interests.
The authors would like to thank Jimma University for financial support, all the respondents of this study at each Hospitals and data collector.