Family Medicine & Medical Science Research
Open Access
ISSN: 2327-4972
ISSN: 2327-4972
Research Article - (2019)Volume 8, Issue 2
Background: Women continue to experience various problems utilizing skilled attendants help at delivery. The clinical causes of maternal deaths, the characteristics of women who die and the causes inherent to the health care system are well known in Ethiopia and elsewhere. Less is known about the perception of risk that may contribute to
women’s deaths during pregnancy and childbirth.
Methods: A community based cross-sectional study was undertaken on 610 pregnant women who were in their third trimester in January 2015. Systematic random sampling technique was applied. Data were collected using a modified version of the Champion’s Health Belief Model Constructs Instrument to assess the perception of risk of home
delivery among pregnant women.
Result: Among women with a last live birth delivered anytime within two years prior to the survey, 55.6% (95% CI: 1.07-1.47) had been assisted by Non-skilled birth attendants. It was shown that home delivery was significantly associated with perceived susceptibility (AOR=4.93, 95% CI: 2.94-8.20), perceived barrier (AOR=5.00 95% CI: 3.05-8.20) and perceived severity (AOR=1.62, 95% CI: 1.04-2.54). The largest variance of intention to give birth at home was explained by Perceived Seriousness (46.2%) and followed by Perceive Susceptibility (32.2%) and perceived barrier (26.4%) among pregnant mothers.
Conclusion: Given the perceived susceptibility, perceived severity and perceived barriers roles in home delivery prediction, it is recommended to consider these structures in designing educational interventions in order to promote institutional delivery in the research area.
HBM; Risk; Non-skilled Birth Attendants; Perception
HBM: Health Belief Model; NSBA: Non-Skilled Birth Attendants
Maternal mortality is a sensitive indicator of maternal health and well-being in any country. The World Health Organization (WHO) has defined maternal mortality as “The death of a woman while pregnant or within 42 days of a termination of a pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental and incidental causes” [1].
Globally, it is estimated that 10.7 million died in the 25 years between 1990 and 2015 due to maternal causes. Although substantial progress has been made in reducing maternal mortality, the World Health Organization (WHO) estimated that in 2015, 303,000 women died from potentially avoidable problems in pregnancy or childbirth worldwide [2].
In comparison to other countries found in Africa, Ethiopia has one of the highest rates of maternal mortality. Progress on reducing maternal mortality has stalled since 2005 when the country managed to reduce Maternal Mortality Ratio (MMR) to 676 per 100,000 births in 2010/11 from 871 in 2000/01 [3]. In Ethiopia, the percentage of deliveries attended by skilled birth attendants was only 20.4% in 2011/12, much lower than skilled delivery of 74% and 44% respectively for urban and rural communities in the Southern and Eastern African region [4,5]. To strengthen maternal health components, Ethiopia has adapted the current global development agenda (SDGs) which has 17 goals, with Goal 3 focusing on health (ensure healthy lives and promote well-being for all at all ages) [6]. In many lowincome countries including Ethiopia, Nepal, pregnancy and childbirth are often perceived as normal life events without justification to seek professional help [7,8]. In fact, need factors can be driven by pregnancy-related factors such as perception [9], Those women who perceive the need for professional help and recognize the risk of pregnancy and delivery, are expected to make antenatal visits and prepare and arrange for childbirth [10].Though, Home deliveries are chosen or occur for a variety of reasons [8,9], it has been associated with adverse infant and maternal outcome [11,12].
Extant research has pointed to some possible explanation. A range of factors such as knowledge of pregnancy and health risks, importance given to pregnancy, earlier health facility use, pre-birth visits and pregnancy complications, can affect whether a woman perceives the need for institutional delivery. Some studies reported that multiparity was perceived as a significant risk factor for a home delivery [13,14] and associated with use of postnatal care [15]. The other main reasons for low utilization of health care services was due to lack of response by health professionals to the perceived risk of the women [16].
Culture plays a major role in the way a woman perceives and prepares for her birthing experience. If healthcare providers are familiar with different Ideas, rituals and behavioral restrictions and proscriptions, and communicate with the women for whom they care, then women from rural backgrounds will have a choice [17]. Local myths and misconceptions about pregnancy and birth have been noted as factors deterring health care seeking [18,19]. Specifically, some authors argue that careseeking during pregnancy is highly influenced by the perception adverse outcomes result from witchcraft [20].
On the other hand, several previous studies have examined the factors contributing to poor maternal and child health outcome and access to care in Ethiopia [13,14,21-24]. A positive perception of the added value of delivery in a facility is usually the motivating factor for women and families to seek maternity care [25]. On the other hand, since pregnancy and childbirth are often considered normal events, if this value is not perceived, professional care is unlikely to be sought [26].
According to the behavioral model proposed by Andersen, [27,28] need factors are essential to health care seeking behavior. For facility delivery service utilization, this means that the pregnant woman and her family must perceive that pregnancy and childbirth as abnormal events, where life-threatening situations may arise without any prediction [29].
An extensive body of literature exists on factors that influence facility delivery [30-34]. Majority of studies have focused on the demand side-for example, the characteristics of women and their families. Few studies have attempted the complex task of assessing women’s perceived need for health-facility delivery. But has not been comprehensively assessed in Ethiopia in relation to the health belief model developed by Hochbaum, Rosen stock and Becker. Many of the studies have not linked the perception of mothers to home delivery risks. Therefore, this study assesses the perceptions of home delivery risk and associated factors among pregnant mothers in Amhara regional state, Ethiopia.
The HBM has been used extensively in the study of health screening behaviors ranging from influenza inoculations, seatbelt use, nutrition, chronic illness, smoking, breast cancer screening-both self-examination and mammography, to health beliefs and AIDS-related health behaviors; however, it has been seldom used in home delivery-related behaviors. Perceived Susceptibility and Perceived Severity Threat perception is highlighted in this model as an important step in recognizing the value in taking a recommended action to reduce the threat. Earlier versions of the model, in fact, combined perceived susceptibility and perceived severity and labeled the component as perceived threat. Perceptions of susceptibility and severity are highly subjective (Figure 1). Where some people will see a particular health problem as imminent and life-threatening, and are prepared to take preventive action, others will see themselves as immune and preventive measures are unnecessary. If the perception of severity is low, then “ there might be no subsequent consideration of susceptibility, ” but when the perception of severity reaches a certain point, then susceptibility becomes more real and preventive measures are considered [19-21,35-37].
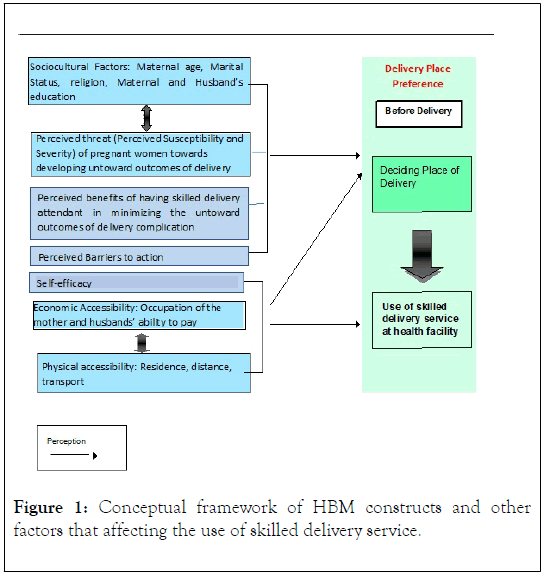
Figure 1. Conceptual framework of HBM constructs and other factors that affecting the use of skilled delivery service.
Study design
A cross-sectional community-based study was employed in January2015. The study was conducted in North Achefer district, which is located 110 km far away from Bahir Dar, to the Southeast direction of Ethiopia. The total population of the district is estimated to be 215,723 of which 50.3% are males and 49.7% are females (according to 2015 population estimation of the district) [23]. There are 27 Kebeles (sub districts). Concerning to the health service facilities, there are 7 health centres, two higher clinics, 24 health posts, 1 district hospital, 14 private health institutions. The lowest level of referral system in Ethiopia is the primary health care unit, which is composed of five satellite health posts, one health center and one primary hospital [24].
The study subjects were pregnant women who were in their third trimester of pregnancy and who gave birth in the last two years prior to the survey.
Sample size determination
The Sample size for the study was calculated using a single population proportion formula, at 95% level of confidence, 5% of margin error, and taking perception of home delivery risk 25.6% [26]. To determine sample size some important factors like Educational status, age, occupation and perceived barriers [26,27] were also considered and the one which gives the highest sample size was used. Therefore; perception of home delivery risks was used for sample size calculation since it gave maximum figure which can address all study objectives. With these assumptions, the resulting sample size becomes 584. Considering 5% non-response rate, the final sample size became 614.
Sampling procedure
Out of 15 districts of West Gojjam zone, North Achefer district was selected by convenience because it represents the whole zone. Then all the 24 Kebeles of North Achefer district was included in the sampling frame and out of which 6 Kebeles were randomly selected using simple random sampling (lottery) method. The total population size of the six Keble’s was 56,110, out of which 1545 were estimated to be pregnant women. It is from these target population that the required sample size was taken according to the size of the sample frame in each Keble.
To get the individual sample units (subjects) at household level, a map of each Keble was taken from the district Administration Office. The center of each Keble was located and to start the first house a lottery method was used. If eligible person was not found, the consecutive households were selected until eligible person is found by jumping every 3 house in the same direction.
Data collection instruments
The data were collected using a modified champion’s health belief model questionnaire. The questioner included two parts: 1. Socio-demographic characteristics of participants; 2. Health belief model constructs: HBM scales were measured in relation to perception of home delivery risk and 22 item questions where composed under 5 major HBM constructs that is perceived susceptibility, perceived severity, perceived benefit, perceived barrier and self-efficacy.
Data were collected by ten trained diploma nurses and supervised by three BSc health workers. The questionnaire was prepared first in English and translated to Amharic (The official language that is fluently spoken by all participants) and then translated back to English for the purpose of checking consistency. Lastly, the Amharic version was used for data collection.
Data quality assurance
For data quality assurance, data collectors and three supervisors were trained for two days on interviewing technique, the logical order of the questionnaire, ways to approach and collect data, keeping confidentiality and privacy. Questionnaire forms were piloted on 31 (5% of 614) volunteer women out of the main sampling of the study and any necessary modifications were done. Daily information exchange was conducted to correct problems during the course of data collection. All collected data were checked for completeness, accuracy, and consistency by the principal investigator each day. Anything which was unclear were corrected and communicated to the data collectors on the next day and dummy tables and tallying were used to clarify and maintain collected data.
Data management, processing and analysis
Data clean up and cross-checking were done before analysis. Data were checked, coded and entered to EPI INFO version 6 then it was exported to SPSS version 20 for analysis. Both descriptive and analytical statistical procedures were utilized. Descriptive statistics was described by tabulation; percent, mean and standard deviation were used for the presentation of demographic data.
Binary logistic regression was used to identify factors associated with home delivery among the pregnant mothers. Variables with p-value less than or equal to 0.25 were fitted in to multiple logistic regression models for controlling the possible effect of confounders and finally the variables which had independent association with home delivery were identified on the basis of OR, with 95% CI and p-value less than 0.05.
Socio demographic characteristics of the respondents
A total of 610 pregnant women from rural areas of North Achefere district voluntarily responded, making the response rate 99.4%. The age of the respondents ranges from 15-49 years. The mean age of the respondents was 30 (SD ± 8.5) years. About 110 (18.0%) were within the age of 25-29 years. From the total study participants, 555 (91.0%) of respondents were Orthodox Christian and 55 (9%) were Muslim religion followers. The great majority (99.1%) ethnically identified themselves as Amhara.
Regarding the marital status, 53 (8.6%) were single, 486 (79.6%) were married and in union, 33 (5.4%) were married and not in union, 23 (3.7%) were divorced and 15 (2.4%) were widowed. School attendance among the respondents was very low in the study area. About 392 (64.3%) of all the respondents never attended formal schooling (Table 1).
| Variables | Frequency (%) |
|---|---|
| Age (N=610) | |
| 15-19 | 100 (16.5) |
| 20-24 | 74 (12.1) |
| 25-29 | 110 (18.0) |
| 30-34 | 105 (17.2) |
| 35-39 | 143 (23.4) |
| >40 | 70 (12.8) |
| Religion (N=610) | |
| Orthodox | 555 (91.0) |
| Muslim/Islam | 55 (9.0) |
| Ethnicity (N=610) | |
| Amhara | 605 (99.1) |
| Marital Status (N=610) | |
| Single | 53 (8.6) |
| Married (union) | 486 (79.6) |
| Married (separately) | 33 (5.4) |
| Divorced | 23 (3.7) |
| Widowed | 15 (2.4) |
| Educational status (N=610) | |
| No formal education | 514 (84.3) |
| Elementary school | 44 (7.2) |
| Secondary and above school | 52 (8.5) |
| Educational status of husband (N=610) | |
| No formal education | 392 (64.3) |
| Elementary school | 135 (22.1) |
| Secondary and above school | 83 (13.6) |
| Occupational status (N=610) | |
| Housewife | 536 (87.9) |
| Employee/Gov’t & non-gov’t | 10 (1.6) |
| Merchant | 38 (6.2) |
| Student | 26 (4.3) |
| Occupation status of husband (N=610) | |
| Farmer | 409 (67.0) |
| Employee/Gov’t & non-gov’t | 14 (2.4) |
| Merchant | 177 (29.0) |
| Student | 10 (1.6) |
| Annual income (N=610) | |
| <16000 | 75 (12.3) |
| 16001-32000 | 332 (54.4) |
| 32001-48000 | 132 (21.6) |
| >48000 | 71 (11.7) |
| Media exposure (N=610) | |
| Radio only | 87 (31.0) |
| None | 523 (69.0) |
| Age at first marriage (N=610) | |
| <18 | 405 (66.4) |
| ≥18 | 205 (33.6) |
| Age of first child delivered (N=507) | |
| <18 | 214 (42.2) |
| >18 | 293 (57.8) |
| Number of children ever born during life (N=507) | |
| <5 | 382 (75.3) |
| >5 | 125 (24.7) |
| Experience child death (N=507) | |
| Yes | 179 (35.3) |
| No | 328 (64.7) |
| *1 Ethiopian Birr=27.01 US$ | |
Table 1: Socio-demographic characteristics of mothers (N=610) in North Achefer district, Amhara Region, Ethiopia, 2015.
Utilization of maternal health services
In this study, respondents have an average of two live children. More than half 55.5% (95% CI:1.07-1.47) of the mothers delivered their children in their own home, 28.5% at governmental health centers, while 5.4%, delivered at the governmental hospital and 10.5% at Private/NGO clinics. More than half (55.6%) of the deliveries are assisted by non-skilled birth attendants (Table 2). Regarding the source of information and support to delivery, 228 (37.3%) reported receiving from traditional birth attendants, 99 (16.2%) from husbands/ partners, 96 (15.7%) from mothers/grandmothers, 74 (12.1%) from neighbors, 87 (14.2%) from health professionals and 26 (4.2%) from mass media.
| Variables | Number (%) |
|---|---|
| Delivery place in the last 24 months | |
| Own home | 339 (55.6) |
| Government hospital | 33 (5.4) |
| Government health center | 174 (28.5) |
| Private/ngos | 64 (10.5) |
| Delivery assisted | |
| Trained Birth Attendants | 271 (44.4) |
| Non- Skilled Birth Attendants | 339 (55.6) |
| Source of information on place of delivery | |
| Traditional Birth Attendants | 228 (37.3) |
| Husbands/partners | 99 (16.2) |
| Mothers/grandmothers | 96 (15.7) |
| Neighbors | 74 (12.1) |
| Health workers | 87 (14.2) |
| Mass media | 26 (4.2) |
Table 2: Distribution of mothers (N=610) by utilization of maternal health and other related services, North Achefer district, West Gojjam zone, ANRS, Ethiopia, 2015.
Factors association with home delivery
In bivariate logistic regression analysis; variables that fulfill the requirement (p<0.2) were exported for multivariate logistic regression to examine the effects of potential cofounders. Age, respondents and partner educational status, discussion about delivery with health workers, perceived susceptibility, perceived barriers and perceived severity were independent predictors of home delivery. By controlling possible cofounders, respondents in the age group of 15-19 and 20-24 were 4.13 (AOR=4.13, 95% CI: 1.86-9.17) and 3.85 (1.66-8.93) times more likely to give birth at home than respondents in the age group of 30 and above years. Respondents whose husband who had no formal education were 2.20 (AOR=2.20, 95% CI: 1.08-4.48) times more likely to give birth at home compared to partners with educational level of secondary and above. Pregnant women who hadn’t discussed delivery issues with health workers were 2.11 (AOR=2.11, 95% CI: 1.28-3.50) times more likely to give birth at home than their counterparts.
Pregnant women’s who had low perceived susceptibility were more likely to give birth at home than those having high perception (AOR=4.93, 95% CI: 2.94-8.20). Those who had a low perception of severity were more likely to have the intention to give birth at home compared to those who had high perception, (AOR=1.62, 95% CI: 1.04-2.54). Those who had a high perception on barriers were less likely to have the intention to give birth at institution compared to those having a low perception on barriers, (AOR=5.00 95% CI:3.05-8.20) (Table 3). Self-efficacy and cues to action did not reveal a statistically significant association with home delivery when adjusted.
| Explanatory variable | Home Delivery | OR with 95% CI | P-value (Overall) | ||
|---|---|---|---|---|---|
| Yes | No | COR (95% C.I) | AOR (95% C.I) | ||
| Age of respondents | |||||
| 15-19 | 36 | 64 | 2.18 (1.10-4.33)* | 4.13 (1.86-9.17)* | <0.001 |
| 20-24 | 26 | 48 | 2.10 (1.10-4.34)* | 3.85 (1.66-8.93)* | |
| 25-29 | 20 | 90 | 0.86 (0.41-1.80) | 1.01 (0.45-2.25) | |
| 30-34 | 17 | 88 | 0.75 (0.35-1.60) | 0.77 (0.33-1.75) | |
| 35-39 | 30 | 113 | 1.03 (0.52-2.03) | 1.37 (0.64-2.92) | |
| ≥40 | 16 | 62 | 1 | 1 | |
| Educational status of respondent | |||||
| No formal education | 131 | 383 | 2.62 (1.10-6.30)* | 2.18 (0.78-6.02) | 0.22 |
| Elementary school | 8 | 36 | 1.70 (0.54-5.35) | 2.78 (0.57-9.10) | |
| Secondary & above | 6 | 46 | 1 | 1 | |
| Educational status of husband | |||||
| No formal education | 111 | 281 | 2.34 (1.22-4.48)* | 2.20 (1.08-4.48)* | 0.04 |
| Elementary school | 22 | 113 | 1.15 (0.54-2.47) | 1.30 (0.56-2.98) | |
| Secondary& above | 12 | 71 | 1 | 1 | |
| Discussion with health workers about delivery | |||||
| Yes | 116 | 289 | 1 | 1 | 0.008 |
| No | 29 | 176 | 2.44 (1.56-3.813)** | 2.11 (1.28-3.50)* | |
| Perceived Susceptibility | |||||
| Low | 215 | 24 | 4.33 (2.70-6.94)** | 4.93 (2.94-8.20)** | >0.001 |
| High | 250 | 121 | 1 | 1 | |
| Perceived Severity | |||||
| Low | 200 | 47 | 1.57 (1.06-2.33)* | 1.62 (1.04-2.54)* | 0.04 |
| High | 265 | 98 | 1 | 1 | |
| Perceived Barrier | |||||
| Low | 260 | 40 | 1 | 1 | >0.001 |
| High | 203 | 105 | 3.36 (2.24-5.05)** | 5.00 (3.05-8.20)** | |
| *p-value significant at low perception; **p-value significant at high perception | |||||
Table 3: Home delivery among pregnant women versus socio-demographic and theoretical variables, North Achefer, 2015.
Health belief model constructs
Cronbach's coefficient alphas were computed to obtain internal consistency estimates of reliability for the seven constructs. The results showed that all seven constructs met the minimum Cronbach's coefficient reliability of 0.70 (alphas between 0.66 and 0.88), which indicated satisfactory internal consistency of each construct.
The largest variance of intention to give birth at home was explained by Perceived Seriousness (46.2%) and followed by Perceived Susceptibility (32.2%) and perceived barrier (26.4%) among pregnant mothers.
The three predictors of the HBM (Perceived Seriousness, Perceived Barrier, and Perceived Susceptibility) explain 71.3% of the total variance of HBM. Perceived Susceptibility and Perceived Seriousness explained only 51.7% of the variance in intention to give birth at home or the perception.
The strongest predictor of perception to give birth at home was Perceived Barrier (β=0.53, p<0.001) followed by Perceived seriousness (β=0.47, p<0.001) and Perceived Susceptibility (β=0.39, p<0.001) in descending order. Nevertheless, in the simple linear regression, the strongest predictor was Perceived Seriousness (β=0.69, p<0.000) as of the Perceived Susceptibility (β=0.57, p<0.000) and the perceived barrier was (β=0.49, p<0.000) (Table 4).
| Variables | R | R2 | Adj. R2 |
R2 Change |
F Change |
P-Value | Standard β Coefficient | ||
|---|---|---|---|---|---|---|---|---|---|
| Β PS | Β PSE | Β PB | |||||||
| Socio-demographic variables# | 0.47 | 0.24 | 0.24 | 0.24 | 34.25 | 0.001* | |||
| Perceived Susceptibility | 0.57 | 0.32 | 0.32 | 0.32 | 53.34 | 0.001* | 0.57* | ||
| Perceived Seriousness (PS) | 0.67 | 0.46 | 0.46 | 0.46 | 62.56 | 0.001* | 0.69* | ||
| Perceived Barrier (PB) | 0.47 | 0.26 | 0.26 | 0.26 | 74.79 | 0.000* | 0.49* | ||
| Perceived Susceptibility + Perceived Seriousness | 0.75 | 0.52 | 0.51 | 0.17 | 26.69 | 0.000* | 0.49* | 0.68* | |
| Perceived Susceptibility + Perceived Seriousness + Perceived Barrier | 0.89 | 0.72 | 0.71 | 0.15 | 21.29 | 0.000* | 0.39* | 0.47* | 0.53* |
Table 4: Linear regression analysis for socio-demographic variables and HBM constructs among pregnant mothers with home delivery risks, North Achefere District, West Gojjam Zone, ANRS Ethiopia, 2015.
The present study used a questionnaire, specifically a modified version of Champion ’ s Health Belief Model Constructs Instrument, to assess the perceptions of pregnant women on home delivery risks.
In this study, the direct determinants of home delivery; perceived susceptibility, perceived severity, and perceived barrier were statistically significant to predict the intention to give birth at home. The more pregnant women’s have the perception of not being at risk and believe that getting delivery complication and its outcome would not have serious consequences and the higher perceived barriers to action; the greater will be their intention to give birth at home.
Out of 610 mothers who gave birth during the last 24 months prior this survey, 271 (44.4%) gave birth on health facilities and 339 (55.6%) delivered at home. This finding is consistent with other studies conducted in Woldia Woreda, Ethiopia [38], and Southern Tanzania [39] where the proportion of women who gave birth on health facilities was 48.3% and 46.7%, respectively. However, it is higher as compared to similar community-based studies conducted in Dodota Woreda [40] and Sekela District [41], where the proportion of women who gave birth at health facilities was, only 18%, 12.3%, 12.1% respectively. This discrepancy could be due to the time gap between these studies, difference in study settings and there might have been improvements in accessibility and utilization of health institution delivery service.
Respondents in the age group of 15-19 and 20-24 were 4.13 (AOR=4.13, 95% CI: 1.86-9.17) and 3.85 (1.66-8.93) times more likely to give birth at home than respondents in the age group of 30 and above years. This indicates that most of the pregnant mothers are assisted by non-skilled birth attendants during their delivery. The finding is in line with the study conducted in Nepal, Northern Nigeria [13,14,42]. Women aged 20-34 and those aged 20 years and below were more likely to report assistance by NSBA during their delivery compared with older women aged 35 years and above. We also found that state of residence was positively associated with delivery by NSBA.
Educational status of head of household is one of the factors which affect institutional delivery service utilization. This study showed that respondent ’ s husband who had no formal education were 2.20 (AOR=2.20, 95% CI: 1.08-4.48) times more likely to give birth at home compared to partners with an educational level of secondary and above. This could be due to the reason that the more a husband (household head) is educated, the more he would be aware of the benefits of institutional delivery, so that he could encourage his wife to give birth at health facility. This finding is supported by the other studies done in India, Pradesh, Ethiopia [22-24,40,42-45]. Women who are educated to high school level and higher were more likely to use skilled delivery attendants (AOR=3.4, 95% CI:1.9-6.2) than those who were not educated. Women whose husbands were educated to high school level and higher were also more likely to use skilled delivery attendants.
A positive perception of the added value of delivery in a facility is usually the motivating factor for women and families to seek maternity care. On the other hand, since pregnancy and childbirth are often considered normal events, if this value is not perceived, professional care is unlikely to be sought. In this particular study; pregnant women ’ s who had low perceived susceptibility were 4.93 more likely to have intention give birth at home than those having high perception (AOR=4.93, 95% CI: 2.94-8.20). This finding agrees with the study conducted in India [25], Guatemala [26], Ethiopia [46] and India [47]. This may be due to the fact that, some women did not seek help despite complications they experienced at delivery. For those urban women who experienced some form of complications during delivery and who did not seek help, it was found that about one-third of them felt that the conditions they experienced were normal and did not, therefore, need special attention.
The study also found that home delivery was significantly associated with perceived severity. Pregnant women’s who had a low perception on the seriousness of home delivery risks were 1.62 times more likely to have the intention to give birth at home compared to those who had high perception, (AOR=1.62, 95% CI: 1.04-2.54). This finding is inconsistent with the study conducted in Nepal [27] and Nigeria [43]. This could be due to the fact that, some of the serious pregnancy-related risks were differently perceived by Nigerian women. Many of the women would not perceive these risks as being too serious as they were regarded as normal and to be expected during pregnancy could be the possible causes for the higher prevalence of home delivery among pregnant women.
Perceived barriers are those that are identified to impede the use of skilled attendance. Our study has found that those women who had a high perception on barriers were less likely to have the intention to give birth at institution compared to those having a low perception on barriers, (AOR=5.00 95% CI: 3.05-8.20). This kind of perception could be based on previous self and friends/relative exposures to the service. Perception of poor quality reduces the likelihood of utilizing maternal service and pushes them to take risks by delaying service seeking even in the face of serious complications. This indicates that even if women perceive susceptibility to a home delivery risks to be serious, whether the women will change risky behaviors is influenced by the perception of benefits resulting from making the changes. This is consistent with the study done in Ethiopia [38], wherein it was reported that women don’t use skilled birth care when they had a high perception on barriers.
Perceived Seriousness was the principal and positively correlated variable with a maximum correlation coefficient (r=0.67, p<0.001) followed by a perceived barrier (r=0.49, p<0.001 and Perceived Susceptibility (r=0.43, p<0.001). This finding is in line with a study done among adolescents in Uganda [44] and other previous studies [29-34,48-54]. From this one can deduce that each and every variable has a contribution in explaining the disparities in the perception of home delivery risk [55-63].
This study has some important limitations that should be kept in mind when interpreting the results. First, the cross-sectional nature of the study design does not confirm definitive cause and effect relationship. Furthermore, the study may prone to recall bias since some of the data were collected based on their previous experiences.
Among women with a last live birth delivered anytime within the one year prior to the survey, 55.6% had been assisted by Non-skilled birth attendants. Age, respondents and partner educational status, discussion about delivery with health workers, perceived susceptibility, perceived barriers and perceived severity were significantly associated with home delivery. Although no information source was highly preferred, traditional birth attendants, mothers/grandmothers, husbands/ partners, health professionals, and mass media were the top five sources. In this study, the largest variance of intention to give birth at home was explained by perceived Seriousness (46.2%) and followed by perceive susceptibility (32.2%) and perceived barrier (26.4%) among pregnant mothers.
Endnotes
aHealth post-the smallest unit of health facility at the lower level of administration (kebele).
bKebele is the smallest administrative unit of the Federal Democratic Republic of Ethiopia.
Acknowledgement
The authors are indebted to the Research and Community Service Vice President Office of the University of Gondar for financial support. The authors would also like to thank University of Gondar, facilitators and the study participants for their dedicated cooperation and made the study possible.
Funding
This study was funded by the Research and Community Service Vice President Office of the University of Gondar.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
RB conceived and designed the idea, analyzed the data and wrote the manuscript. AN analyzed the data and critically reviewed the manuscript. All authors read and approved the final draft of the manuscript.
Ethics approval and consent to participate
The protocol for this cross-sectional study was approved by the Institutional Review Board of the University of Gondar on December 15, 2015 (No 1456). All participants gave oral informed consent and parental consent was obtained also for participants under 16 and this form of consent was approved from the ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Citation: Berhe R, Nigusie A (2019) Perceptions of Home Delivery Risk and Associated Factors Among Pregnant Mothers in North Achefer District, Amhara Region of Ethiopia: The Health Belief Model Perspective. Fam Med Med Sci Res 8:238.
Received: 23-Mar-2019 Accepted: 16-May-2019 Published: 23-May-2019
Copyright: © 2019 Berhe R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.